Treating Vascular Diseases with Reprogrammed Amniotic Fluid Cells
|
By LabMedica International staff writers Posted on 01 Nov 2012 |
Scientists have devised a way to utilize diagnostic prenatal amniocentesis cells, reprogramming them into plentiful and stable endothelial cells capable of regenerating damaged blood vessels and repairing injured organs.
The study, published online October 2012 in the journal Cell, illustrates future therapy where amniotic fluid gathered from thousands of amniocentesis procedures annually, during mid-pregnancy to study fetal chromosomes, would be gathered with permission from the women tested. These cells, which are not embryonic, would then be treated with three genes that reprogram them rapidly into billions of endothelial cells. The new endothelial cells could then be frozen and banked similar to same way blood is, and patients who require blood vessel repair would be able to receive the cells with only one injection.
If the technology is validated in future studies, it could dramatically improve treatment for disorders associated an injured vascular system, including lung diseases such as emphysema, diabetes, and trauma, and heart disease, stroke, according to the study’s senior investigator, Dr. Shahin Rafii, a professor of genetic medicine at Weill Cornell Medical College (New York, NY, USA) and codirector of its Ansary Stem Cell Institute. “Currently, there is no curative treatment available for patients with vascular diseases, and the common denominator to all these disorders is dysfunction of blood vessels, specifically endothelial cells that are the building blocks of the vessels,” said Dr. Rafii.
But these cells do much more than just provide the accouterments to direct blood. Dr. Rafii has recently shown that endothelial cells in blood vessels generate growth factors that actively participate in organ maintenance, repair, and regeneration. Therefore, whereas damaged vessels cannot repair the organs they nurture with blood, he says an infusion of new endothelial cells could.
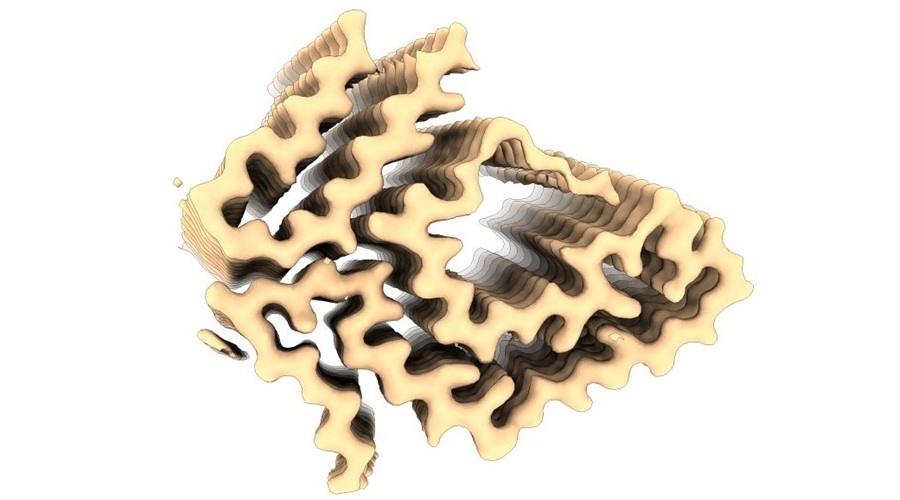
“Replacement of the dysfunctional endothelial cells with transplantation of normal, properly engineered cultured endothelial cells could potentially provide for a novel therapy for many patients,” said study coauthor Dr. Sina Rabbany, adjunct associate professor of bioengineering in genetic medicine at Weill Cornell. “In order to engineer tissues with clinically relevant dimensions, endothelial cells can be assembled into porous three-dimensional scaffolds that, once introduced into a patient’s injured organ, could form true blood vessels.”
According to Dr. Rafii, this study will potentially create a new field of translational vascular medicine. He predicted that only as much as four years are required for the preclinical research to seek US Food and Drug Administration (FDA) approval to begin human clinical trials to further the possibility of reprogrammed endothelial cells for treatment of vascular disorders.
The scientists confirmed, in mice models, that endothelial cells reprogrammed from human amniotic cells could engraft into an injured liver to form healthy, stable, and functional blood vessels. “We have shown that these engrafted endothelial cells have the capacity to produce unique growth factors to promote regeneration of the liver cells,” stated the study’s lead investigator, Dr. Michael Ginsberg, a senior postdoctoral associate in Dr. Rafii’s laboratory.
“The novelty of this technique is that, from 100,000 amniotic cells--a small amount--we grew more than six billion new authentic endothelial cells within a matter of weeks,” Dr. Ginsberg remarked. “And when we injected these cells into mice, a substantial amount of them engrafted into regenerating vessels. It was remarkable to see that these cells went right to work building new blood vessels in the liver as well as producing the right growth factors that could potentially regenerate and repair injured organs.”
In their first research with these cells three years ago, Dr. Ginsberg used cells taken from an amniocentesis given at 16 weeks of gestation. Researchers found that amniotic cells are the “Goldilocks” of cellular programming. “They are not as plastic and unstable as endothelial cells derived from embryonic cells or as stubborn as those produced from reprogramming differentiated adult cells,” Dr. Ginsberg said. Instead, he says amniotic cells provide conditions that are just right--so-called “Goldilocks principle”--for generating endothelial cells.
However, to make that finding, the researchers had to know how to reprogram the amniotic cells. To this end, they looked for the genes that embryonic stem cells use to differentiate into endothelial cells. Dr. Rafii’s group identified three genes that are expressed during vascular development, all of which are members of the E-twenty six (ETS) family of transcription factors known to regulate cellular differentiation, especially blood vessel formation.
Then, the scientists used gene transfer technology to insert the three genes into mature amniotic cells and shut one of them off after a short and vital period of activity by using a special molecular inhibitor. Remarkably, 20% of the amniotic cells could efficiently be reprogrammed into endothelial cells. “This is quite an achievement since current strategies to reprogram adult cells result less than 1% of the time in successful reprogramming into endothelial cells,” said Dr. Rafii.
“These transcription factors do not cause cancer, and the endothelial cells reprogrammed from human amniotic cells are not tumorigenic and could in the future be infused into patients with a large margin of safety,” said Dr. Ginsberg.
The findings suggest that other transcription factors could be used to reprogram the amniotic cells into many other tissue-specific cells, such as those that comprise pancreatic islet cells, muscles, the brain, and other areas of the body. “While our work focused primarily on the reprogramming of amniotic cells into endothelial cells, we surmise that through the use of other transcription factors and growth conditions, our group and others will be able to reprogram mouse and human amniotic cells virtually into every organ cell type, such as hepatocytes in the liver, cardiomyocytes in heart muscle, neurons in the brain and even chondrocytes in cartilage, just to name a few,” Dr. Ginsberg noted.
“Obviously, the implications of these findings would be enormous in the field of translational regenerative medicine,” emphasized study coauthor Dr. Zev Rosenwaks, a professor of reproductive medicine in obstetrics and gynecology at Weill Cornell Medical College and director and physician-in-chief of the Ronald O. Perelman and Claudia Cohen Center for Reproductive Medicine at New York-Presbyterian Hospital/Weill Cornell Medical Center. “The greatest obstacle to overcome in the pursuit to regenerate specific tissues and organs is the requirement for substantial levels of cells--in the billions--that are stable, safe, and durable. Our approach will bring us closer to this milestone.”
“Most importantly, these endothelial cells could be reprogrammed from amniotic cells from genetically diverse individuals,” stated co-author Dr. Venkat R. Pulijaal, director of the cytogenetic laboratory, associate professor of clinical pathology and laboratory medicine at Weill Cornell. What endothelial cells a patient receives would depend on their human leukocyte antigen (HLA) type, which is a set of self-recognition molecules that enable doctors to partner a patient with potential donors of blood or tissue.
A patent has been filed on the discovery.
Related Links:
Weill Cornell Medical College
The study, published online October 2012 in the journal Cell, illustrates future therapy where amniotic fluid gathered from thousands of amniocentesis procedures annually, during mid-pregnancy to study fetal chromosomes, would be gathered with permission from the women tested. These cells, which are not embryonic, would then be treated with three genes that reprogram them rapidly into billions of endothelial cells. The new endothelial cells could then be frozen and banked similar to same way blood is, and patients who require blood vessel repair would be able to receive the cells with only one injection.
If the technology is validated in future studies, it could dramatically improve treatment for disorders associated an injured vascular system, including lung diseases such as emphysema, diabetes, and trauma, and heart disease, stroke, according to the study’s senior investigator, Dr. Shahin Rafii, a professor of genetic medicine at Weill Cornell Medical College (New York, NY, USA) and codirector of its Ansary Stem Cell Institute. “Currently, there is no curative treatment available for patients with vascular diseases, and the common denominator to all these disorders is dysfunction of blood vessels, specifically endothelial cells that are the building blocks of the vessels,” said Dr. Rafii.
But these cells do much more than just provide the accouterments to direct blood. Dr. Rafii has recently shown that endothelial cells in blood vessels generate growth factors that actively participate in organ maintenance, repair, and regeneration. Therefore, whereas damaged vessels cannot repair the organs they nurture with blood, he says an infusion of new endothelial cells could.
“Replacement of the dysfunctional endothelial cells with transplantation of normal, properly engineered cultured endothelial cells could potentially provide for a novel therapy for many patients,” said study coauthor Dr. Sina Rabbany, adjunct associate professor of bioengineering in genetic medicine at Weill Cornell. “In order to engineer tissues with clinically relevant dimensions, endothelial cells can be assembled into porous three-dimensional scaffolds that, once introduced into a patient’s injured organ, could form true blood vessels.”
According to Dr. Rafii, this study will potentially create a new field of translational vascular medicine. He predicted that only as much as four years are required for the preclinical research to seek US Food and Drug Administration (FDA) approval to begin human clinical trials to further the possibility of reprogrammed endothelial cells for treatment of vascular disorders.
The scientists confirmed, in mice models, that endothelial cells reprogrammed from human amniotic cells could engraft into an injured liver to form healthy, stable, and functional blood vessels. “We have shown that these engrafted endothelial cells have the capacity to produce unique growth factors to promote regeneration of the liver cells,” stated the study’s lead investigator, Dr. Michael Ginsberg, a senior postdoctoral associate in Dr. Rafii’s laboratory.
“The novelty of this technique is that, from 100,000 amniotic cells--a small amount--we grew more than six billion new authentic endothelial cells within a matter of weeks,” Dr. Ginsberg remarked. “And when we injected these cells into mice, a substantial amount of them engrafted into regenerating vessels. It was remarkable to see that these cells went right to work building new blood vessels in the liver as well as producing the right growth factors that could potentially regenerate and repair injured organs.”
In their first research with these cells three years ago, Dr. Ginsberg used cells taken from an amniocentesis given at 16 weeks of gestation. Researchers found that amniotic cells are the “Goldilocks” of cellular programming. “They are not as plastic and unstable as endothelial cells derived from embryonic cells or as stubborn as those produced from reprogramming differentiated adult cells,” Dr. Ginsberg said. Instead, he says amniotic cells provide conditions that are just right--so-called “Goldilocks principle”--for generating endothelial cells.
However, to make that finding, the researchers had to know how to reprogram the amniotic cells. To this end, they looked for the genes that embryonic stem cells use to differentiate into endothelial cells. Dr. Rafii’s group identified three genes that are expressed during vascular development, all of which are members of the E-twenty six (ETS) family of transcription factors known to regulate cellular differentiation, especially blood vessel formation.
Then, the scientists used gene transfer technology to insert the three genes into mature amniotic cells and shut one of them off after a short and vital period of activity by using a special molecular inhibitor. Remarkably, 20% of the amniotic cells could efficiently be reprogrammed into endothelial cells. “This is quite an achievement since current strategies to reprogram adult cells result less than 1% of the time in successful reprogramming into endothelial cells,” said Dr. Rafii.
“These transcription factors do not cause cancer, and the endothelial cells reprogrammed from human amniotic cells are not tumorigenic and could in the future be infused into patients with a large margin of safety,” said Dr. Ginsberg.
The findings suggest that other transcription factors could be used to reprogram the amniotic cells into many other tissue-specific cells, such as those that comprise pancreatic islet cells, muscles, the brain, and other areas of the body. “While our work focused primarily on the reprogramming of amniotic cells into endothelial cells, we surmise that through the use of other transcription factors and growth conditions, our group and others will be able to reprogram mouse and human amniotic cells virtually into every organ cell type, such as hepatocytes in the liver, cardiomyocytes in heart muscle, neurons in the brain and even chondrocytes in cartilage, just to name a few,” Dr. Ginsberg noted.
“Obviously, the implications of these findings would be enormous in the field of translational regenerative medicine,” emphasized study coauthor Dr. Zev Rosenwaks, a professor of reproductive medicine in obstetrics and gynecology at Weill Cornell Medical College and director and physician-in-chief of the Ronald O. Perelman and Claudia Cohen Center for Reproductive Medicine at New York-Presbyterian Hospital/Weill Cornell Medical Center. “The greatest obstacle to overcome in the pursuit to regenerate specific tissues and organs is the requirement for substantial levels of cells--in the billions--that are stable, safe, and durable. Our approach will bring us closer to this milestone.”
“Most importantly, these endothelial cells could be reprogrammed from amniotic cells from genetically diverse individuals,” stated co-author Dr. Venkat R. Pulijaal, director of the cytogenetic laboratory, associate professor of clinical pathology and laboratory medicine at Weill Cornell. What endothelial cells a patient receives would depend on their human leukocyte antigen (HLA) type, which is a set of self-recognition molecules that enable doctors to partner a patient with potential donors of blood or tissue.
A patent has been filed on the discovery.
Related Links:
Weill Cornell Medical College
Latest BioResearch News
- Genome Analysis Predicts Likelihood of Neurodisability in Oxygen-Deprived Newborns
- Gene Panel Predicts Disease Progession for Patients with B-cell Lymphoma
- New Method Simplifies Preparation of Tumor Genomic DNA Libraries
- New Tool Developed for Diagnosis of Chronic HBV Infection
- Panel of Genetic Loci Accurately Predicts Risk of Developing Gout
- Disrupted TGFB Signaling Linked to Increased Cancer-Related Bacteria
- Gene Fusion Protein Proposed as Prostate Cancer Biomarker
- NIV Test to Diagnose and Monitor Vascular Complications in Diabetes
- Semen Exosome MicroRNA Proves Biomarker for Prostate Cancer
- Genetic Loci Link Plasma Lipid Levels to CVD Risk
- Newly Identified Gene Network Aids in Early Diagnosis of Autism Spectrum Disorder
- Link Confirmed between Living in Poverty and Developing Diseases
- Genomic Study Identifies Kidney Disease Loci in Type I Diabetes Patients
- Liquid Biopsy More Effective for Analyzing Tumor Drug Resistance Mutations
- New Liquid Biopsy Assay Reveals Host-Pathogen Interactions
- Method Developed for Enriching Trophoblast Population in Samples
Channels
Clinical Chemistry
view channel
New PSA-Based Prognostic Model Improves Prostate Cancer Risk Assessment
Prostate cancer is the second-leading cause of cancer death among American men, and about one in eight will be diagnosed in their lifetime. Screening relies on blood levels of prostate-specific antigen... Read more
Extracellular Vesicles Linked to Heart Failure Risk in CKD Patients
Chronic kidney disease (CKD) affects more than 1 in 7 Americans and is strongly associated with cardiovascular complications, which account for more than half of deaths among people with CKD.... Read moreMolecular Diagnostics
view channel
Diagnostic Device Predicts Treatment Response for Brain Tumors Via Blood Test
Glioblastoma is one of the deadliest forms of brain cancer, largely because doctors have no reliable way to determine whether treatments are working in real time. Assessing therapeutic response currently... Read more
Blood Test Detects Early-Stage Cancers by Measuring Epigenetic Instability
Early-stage cancers are notoriously difficult to detect because molecular changes are subtle and often missed by existing screening tools. Many liquid biopsies rely on measuring absolute DNA methylation... Read more
“Lab-On-A-Disc” Device Paves Way for More Automated Liquid Biopsies
Extracellular vesicles (EVs) are tiny particles released by cells into the bloodstream that carry molecular information about a cell’s condition, including whether it is cancerous. However, EVs are highly... Read more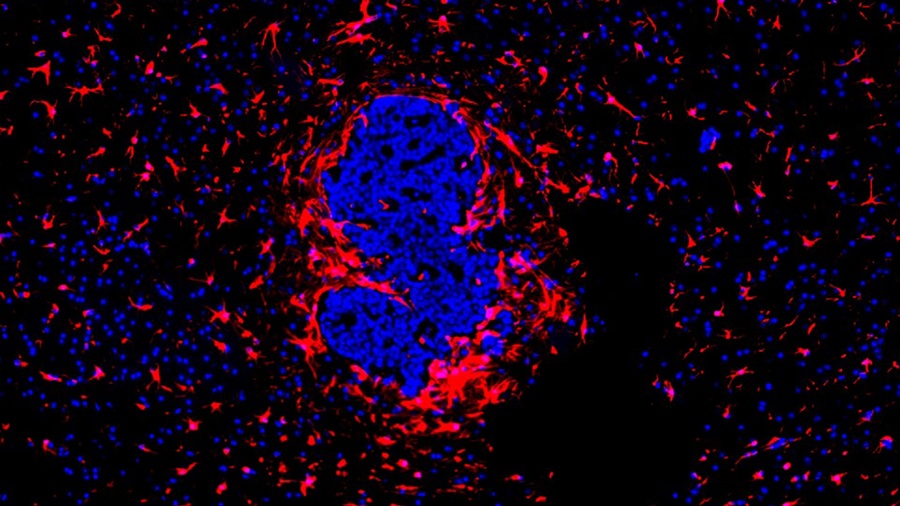
Blood Test Identifies Inflammatory Breast Cancer Patients at Increased Risk of Brain Metastasis
Brain metastasis is a frequent and devastating complication in patients with inflammatory breast cancer, an aggressive subtype with limited treatment options. Despite its high incidence, the biological... Read moreHematology
view channel
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read more
Fast and Easy Test Could Revolutionize Blood Transfusions
Blood transfusions are a cornerstone of modern medicine, yet red blood cells can deteriorate quietly while sitting in cold storage for weeks. Although blood units have a fixed expiration date, cells from... Read more
Automated Hemostasis System Helps Labs of All Sizes Optimize Workflow
High-volume hemostasis sections must sustain rapid turnaround while managing reruns and reflex testing. Manual tube handling and preanalytical checks can strain staff time and increase opportunities for error.... Read more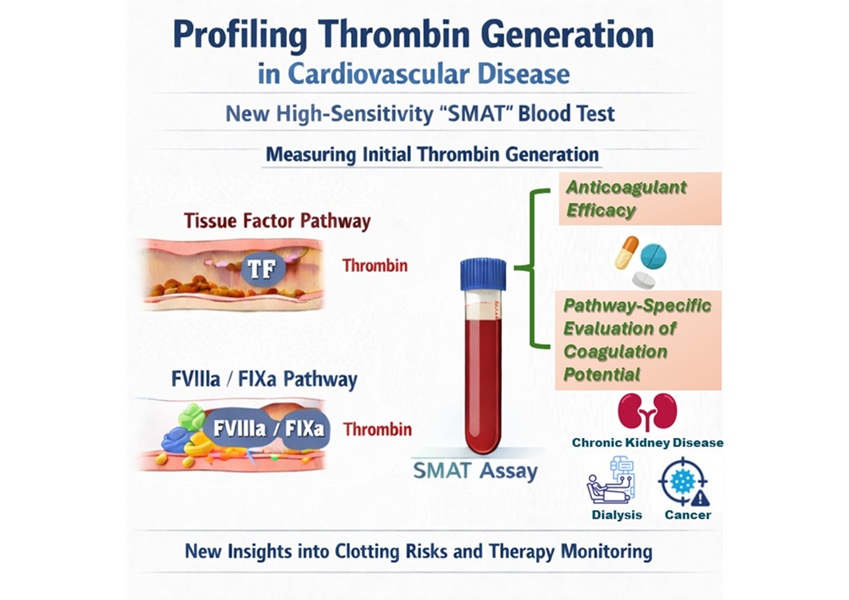
High-Sensitivity Blood Test Improves Assessment of Clotting Risk in Heart Disease Patients
Blood clotting is essential for preventing bleeding, but even small imbalances can lead to serious conditions such as thrombosis or dangerous hemorrhage. In cardiovascular disease, clinicians often struggle... Read moreImmunology
view channelBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read more
Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
Immunotherapy has transformed cancer treatment, but only a small proportion of patients experience lasting benefit, with response rates often remaining between 10% and 20%. Clinicians currently lack reliable... Read moreMicrobiology
view channel
Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
Alzheimer’s disease affects approximately 6.7 million people in the United States and nearly 50 million worldwide, yet early cognitive decline remains difficult to characterize. Increasing evidence suggests... Read moreAI-Powered Platform Enables Rapid Detection of Drug-Resistant C. Auris Pathogens
Infections caused by the pathogenic yeast Candida auris pose a significant threat to hospitalized patients, particularly those with weakened immune systems or those who have invasive medical devices.... Read morePathology
view channel
Engineered Yeast Cells Enable Rapid Testing of Cancer Immunotherapy
Developing new cancer immunotherapies is a slow, costly, and high-risk process, particularly for CAR T cell treatments that must precisely recognize cancer-specific antigens. Small differences in tumor... Read more
First-Of-Its-Kind Test Identifies Autism Risk at Birth
Autism spectrum disorder is treatable, and extensive research shows that early intervention can significantly improve cognitive, social, and behavioral outcomes. Yet in the United States, the average age... Read moreTechnology
view channel
Robotic Technology Unveiled for Automated Diagnostic Blood Draws
Routine diagnostic blood collection is a high‑volume task that can strain staffing and introduce human‑dependent variability, with downstream implications for sample quality and patient experience.... Read more
ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
Clinical laboratories generate billions of test results each year, creating a treasure trove of data with the potential to support more personalized testing, improve operational efficiency, and enhance patient care.... Read moreAptamer Biosensor Technology to Transform Virus Detection
Rapid and reliable virus detection is essential for controlling outbreaks, from seasonal influenza to global pandemics such as COVID-19. Conventional diagnostic methods, including cell culture, antigen... Read more
AI Models Could Predict Pre-Eclampsia and Anemia Earlier Using Routine Blood Tests
Pre-eclampsia and anemia are major contributors to maternal and child mortality worldwide, together accounting for more than half a million deaths each year and leaving millions with long-term health complications.... Read moreIndustry
view channelNew Collaboration Brings Automated Mass Spectrometry to Routine Laboratory Testing
Mass spectrometry is a powerful analytical technique that identifies and quantifies molecules based on their mass and electrical charge. Its high selectivity, sensitivity, and accuracy make it indispensable... Read more
AI-Powered Cervical Cancer Test Set for Major Rollout in Latin America
Noul Co., a Korean company specializing in AI-based blood and cancer diagnostics, announced it will supply its intelligence (AI)-based miLab CER cervical cancer diagnostic solution to Mexico under a multi‑year... Read more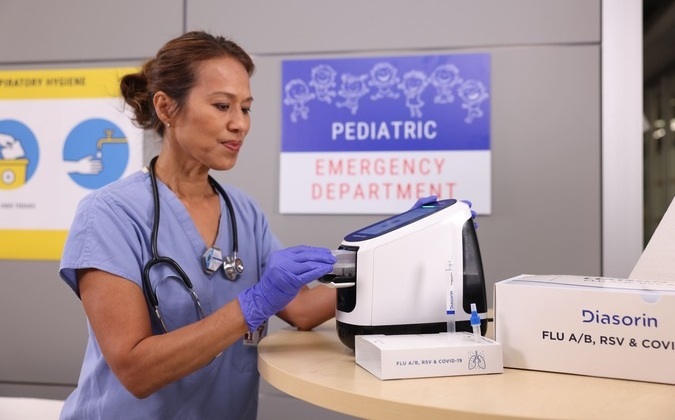
Diasorin and Fisher Scientific Enter into US Distribution Agreement for Molecular POC Platform
Diasorin (Saluggia, Italy) has entered into an exclusive distribution agreement with Fisher Scientific, part of Thermo Fisher Scientific (Waltham, MA, USA), for the LIAISON NES molecular point-of-care... Read more










 (3) (1).png)