Blood Test Identifies Inflammatory Breast Cancer Patients at Increased Risk of Brain Metastasis
Posted on 05 Feb 2026
Brain metastasis is a frequent and devastating complication in patients with inflammatory breast cancer, an aggressive subtype with limited treatment options. Despite its high incidence, the biological mechanisms driving cancer spread to the brain remain poorly understood, leaving clinicians without reliable tools to predict or prevent it. This gap has hindered early intervention and contributed to poor survival outcomes. Now, a new study has identified a measurable blood biomarker linked to brain metastasis risk and highlights a druggable pathway that could help prevent or treat this complication.
In research led by The University of Texas MD Anderson Cancer Center (Houston, TX, USA), investigators focused on soluble E-cadherin (sEcad), a circulating form of a cell adhesion protein previously associated with aggressive cancer behavior. Building on earlier clinical observations, the team examined how elevated sEcad levels influence tumor spread, survival, and inflammation in inflammatory breast cancer using advanced preclinical models.
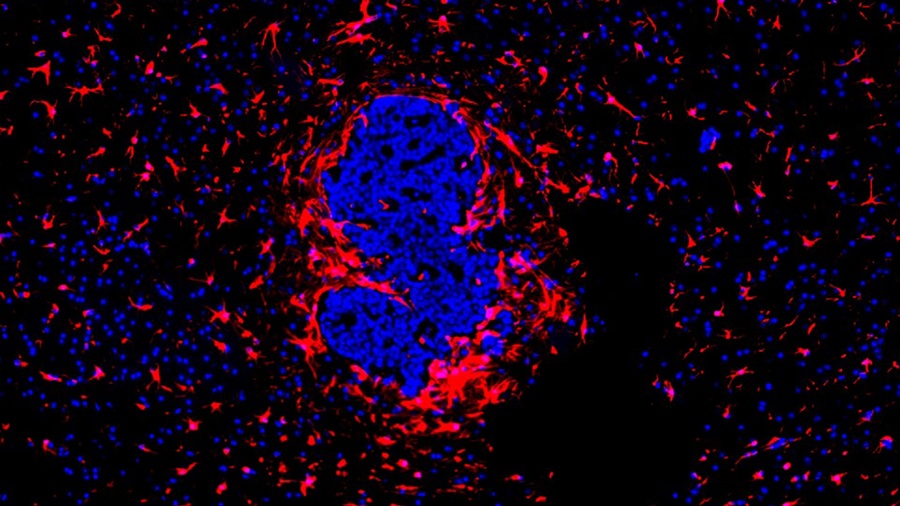
The researchers discovered that sEcad activates the CXCR2 signaling pathway, creating a feedback loop that promotes tumor invasion, helps cancer cells resist programmed cell death, and induces inflammation in the brain microenvironment. This inflammatory state supports metastatic growth, making the brain more susceptible to tumor colonization. The study also explored whether interrupting this pathway could reduce metastasis and improve survival.
In preclinical models overexpressing sEcad, researchers observed increased metastatic burden, reduced overall survival, and significantly higher rates of brain metastasis. Importantly, treatment with a CXCR2 inhibitor markedly reduced metastatic spread and extended survival. These findings, published in Neuro-Oncology, demonstrate both the prognostic value of sEcad and the therapeutic potential of targeting the CXCR2 pathway.
The results suggest that monitoring sEcad levels in blood could help identify inflammatory breast cancer patients at the highest risk of brain metastasis. Targeting the sEcad–CXCR2 axis may offer a new strategy to prevent or treat brain involvement in this aggressive disease. Future studies will focus on validating sEcad as a clinical biomarker and advancing CXCR2 inhibitors toward patient-centered trials.
“This readily measurable blood biomarker plays a key role in driving brain metastasis,” said Bisrat Debeb, D.V.M., Ph.D., co-lead investigator of the study. “Targeting this pathway has tremendous potential to treat and prevent this serious complication and could help guide future therapies.”
Related Links:
MD Anderson Cancer Center














