Panel of Five Serum Biomarkers Identifies COVID-19 Patients at High Risk to Develop Serious Complications
|
By LabMedica International staff writers Posted on 18 Aug 2020 |
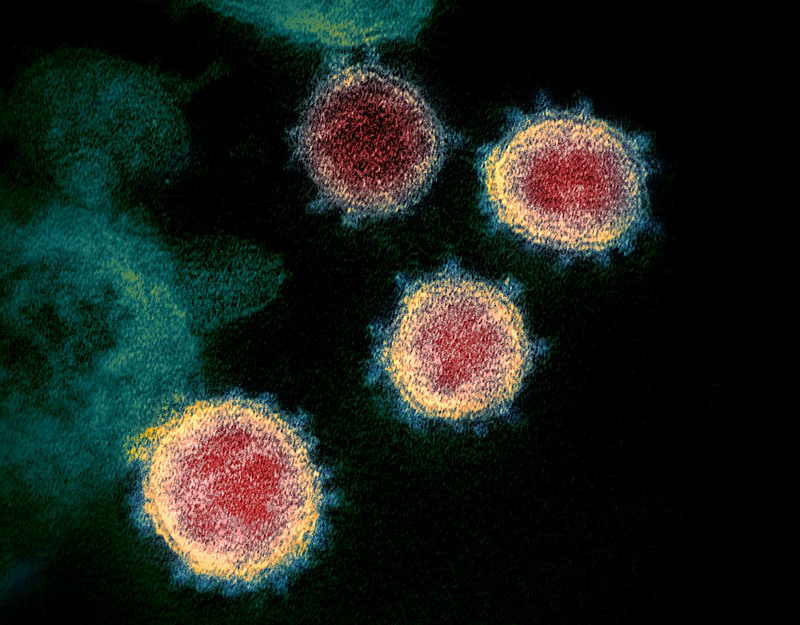
Transmission electron microscope image of SARS-CoV-2 (2019-nCoV), the virus that causes COVID-19, isolated from a patient in the U.S.A. Virus particles are shown emerging from the surface of cells cultured in the laboratory. (Image courtesy of National Institute of Allergy and Infectious Diseases via Wikimedia Commons)
A recent paper suggested that elevated levels of five serum biomarkers could be used to identify COVID-19 patients who are at high risk for serious complications or death.
Based on early Chinese COVID-19 studies showing that certain biomarkers were associated with bad outcomes, investigators at George Washington University (Washington, DC, USA) determined levels of five serum biomarkers in samples obtained from 299 patients diagnosed with COVID-19 admitted to George Washington Hospital between March 12 and May 9, 2020.
The five biomarkers measured were:
1) D-dimer, a fibrin degradation product present in the blood after a blood clot has been degraded by fibrinolysis. It was so named because it contains two D fragments of the fibrin protein joined by a cross-link. D-dimer concentration may be determined by a blood test to help diagnose thrombosis. Since its introduction in the 1990s, it has become an important test performed in patients with suspected thrombotic disorders. A four-fold increase in the protein is a strong indicator of mortality in those suffering from COVID-19.
2) C-reactive protein (CRP) is a ring-shaped, pentameric protein found in blood plasma, whose circulating concentrations rise in response to inflammation. It is an acute-phase protein of hepatic origin that increases following interleukin-6 secretion by macrophages and T-cells.
3) IL-6 (interleukin-6) is an important mediator of fever and of the acute phase response. There is some early evidence that IL-6 can be used as an inflammatory marker for severe COVID-19 infection with poor prognosis, in the context of the wider coronavirus pandemic.
4). Lactate dehydrogenase (LDH) is an enzyme found in nearly all living cells. LDH catalyzes the conversion of lactate to pyruvate and back, as it converts NAD+ to NADH and back. LDH is expressed extensively in body tissues, such as blood cells and heart muscle. Since it is released during tissue damage, LDH is a marker of common injuries and disease such as heart failure.
5) Ferritin is a universal intracellular protein that stores iron and releases it in a controlled fashion. Plasma ferritin is an indirect marker of the total amount of iron stored in the body and is used as a diagnostic test for iron-deficiency anemia.
For each patient, age, sex, BMI, comorbidities, and medications were recorded. Laboratory tests were performed either in the emergency room prior to admission or after the admission orders, and patients were placed in one of the special COVID-19 units. In addition to routine admission laboratory studies, CRP, D-dimer, IL-6, ferritin, and LDH were recorded. Further, the maximum oxygen requirements prior to transfer to ICU, transfer to the ICU, necessity for mechanical ventilation, and discharge status were noted.
Results revealed that elevated levels of these biomarkers were associated with inflammation and bleeding disorder, showing an independent increased risk for ICU admission, invasive ventilatory support, and death. The highest odds of death occurred when the LDH level was greater than 1200 units/liter and a D-dimer level was greater than 3 microgram/milliliter.
"When we first started treating COVID-19 patients, we watched them get better or get worse, but we did not know why," said contributing authour Dr. Juan Reyes, assistant professor of medicine at the George Washington University. "Some initial studies had come out of China showing certain biomarkers were associated with bad outcomes. There was a desire to see if that was true for our patients here in the U.S."
"We hope these biomarkers help physicians determine how aggressively they need to treat patients, whether a patient should be discharged, and how to monitor patients who are going home, among other clinical decisions," said first author Dr. Shant Ayanian, assistant professor of medicine at George Washington University.
The study was published in the July 17, 2020, online edition of the journal Future Medicine.
Related Links:
George Washington University
Based on early Chinese COVID-19 studies showing that certain biomarkers were associated with bad outcomes, investigators at George Washington University (Washington, DC, USA) determined levels of five serum biomarkers in samples obtained from 299 patients diagnosed with COVID-19 admitted to George Washington Hospital between March 12 and May 9, 2020.
The five biomarkers measured were:
1) D-dimer, a fibrin degradation product present in the blood after a blood clot has been degraded by fibrinolysis. It was so named because it contains two D fragments of the fibrin protein joined by a cross-link. D-dimer concentration may be determined by a blood test to help diagnose thrombosis. Since its introduction in the 1990s, it has become an important test performed in patients with suspected thrombotic disorders. A four-fold increase in the protein is a strong indicator of mortality in those suffering from COVID-19.
2) C-reactive protein (CRP) is a ring-shaped, pentameric protein found in blood plasma, whose circulating concentrations rise in response to inflammation. It is an acute-phase protein of hepatic origin that increases following interleukin-6 secretion by macrophages and T-cells.
3) IL-6 (interleukin-6) is an important mediator of fever and of the acute phase response. There is some early evidence that IL-6 can be used as an inflammatory marker for severe COVID-19 infection with poor prognosis, in the context of the wider coronavirus pandemic.
4). Lactate dehydrogenase (LDH) is an enzyme found in nearly all living cells. LDH catalyzes the conversion of lactate to pyruvate and back, as it converts NAD+ to NADH and back. LDH is expressed extensively in body tissues, such as blood cells and heart muscle. Since it is released during tissue damage, LDH is a marker of common injuries and disease such as heart failure.
5) Ferritin is a universal intracellular protein that stores iron and releases it in a controlled fashion. Plasma ferritin is an indirect marker of the total amount of iron stored in the body and is used as a diagnostic test for iron-deficiency anemia.
For each patient, age, sex, BMI, comorbidities, and medications were recorded. Laboratory tests were performed either in the emergency room prior to admission or after the admission orders, and patients were placed in one of the special COVID-19 units. In addition to routine admission laboratory studies, CRP, D-dimer, IL-6, ferritin, and LDH were recorded. Further, the maximum oxygen requirements prior to transfer to ICU, transfer to the ICU, necessity for mechanical ventilation, and discharge status were noted.
Results revealed that elevated levels of these biomarkers were associated with inflammation and bleeding disorder, showing an independent increased risk for ICU admission, invasive ventilatory support, and death. The highest odds of death occurred when the LDH level was greater than 1200 units/liter and a D-dimer level was greater than 3 microgram/milliliter.
"When we first started treating COVID-19 patients, we watched them get better or get worse, but we did not know why," said contributing authour Dr. Juan Reyes, assistant professor of medicine at the George Washington University. "Some initial studies had come out of China showing certain biomarkers were associated with bad outcomes. There was a desire to see if that was true for our patients here in the U.S."
"We hope these biomarkers help physicians determine how aggressively they need to treat patients, whether a patient should be discharged, and how to monitor patients who are going home, among other clinical decisions," said first author Dr. Shant Ayanian, assistant professor of medicine at George Washington University.
The study was published in the July 17, 2020, online edition of the journal Future Medicine.
Related Links:
George Washington University
Latest COVID-19 News
- New Immunosensor Paves Way to Rapid POC Testing for COVID-19 and Emerging Infectious Diseases
- Long COVID Etiologies Found in Acute Infection Blood Samples
- Novel Device Detects COVID-19 Antibodies in Five Minutes
- CRISPR-Powered COVID-19 Test Detects SARS-CoV-2 in 30 Minutes Using Gene Scissors
- Gut Microbiome Dysbiosis Linked to COVID-19
- Novel SARS CoV-2 Rapid Antigen Test Validated for Diagnostic Accuracy
- New COVID + Flu + R.S.V. Test to Help Prepare for `Tripledemic`
- AI Takes Guesswork Out Of Lateral Flow Testing
- Fastest Ever SARS-CoV-2 Antigen Test Designed for Non-Invasive COVID-19 Testing in Any Setting
- Rapid Antigen Tests Detect Omicron, Delta SARS-CoV-2 Variants
- Health Care Professionals Showed Increased Interest in POC Technologies During Pandemic, Finds Study
- Set Up Reserve Lab Capacity Now for Faster Response to Next Pandemic, Say Researchers
- Blood Test Performed During Initial Infection Predicts Long COVID Risk
- Low-Cost COVID-19 Testing Platform Combines Sensitivity of PCR and Speed of Antigen Tests
- Finger-Prick Blood Test Identifies Immunity to COVID-19
- Quick Test Kit Determines Immunity Against COVID-19 and Its Variants
Channels
Clinical Chemistry
view channel
New PSA-Based Prognostic Model Improves Prostate Cancer Risk Assessment
Prostate cancer is the second-leading cause of cancer death among American men, and about one in eight will be diagnosed in their lifetime. Screening relies on blood levels of prostate-specific antigen... Read more
Extracellular Vesicles Linked to Heart Failure Risk in CKD Patients
Chronic kidney disease (CKD) affects more than 1 in 7 Americans and is strongly associated with cardiovascular complications, which account for more than half of deaths among people with CKD.... Read moreHematology
view channel
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read more
Fast and Easy Test Could Revolutionize Blood Transfusions
Blood transfusions are a cornerstone of modern medicine, yet red blood cells can deteriorate quietly while sitting in cold storage for weeks. Although blood units have a fixed expiration date, cells from... Read more
Automated Hemostasis System Helps Labs of All Sizes Optimize Workflow
High-volume hemostasis sections must sustain rapid turnaround while managing reruns and reflex testing. Manual tube handling and preanalytical checks can strain staff time and increase opportunities for error.... Read more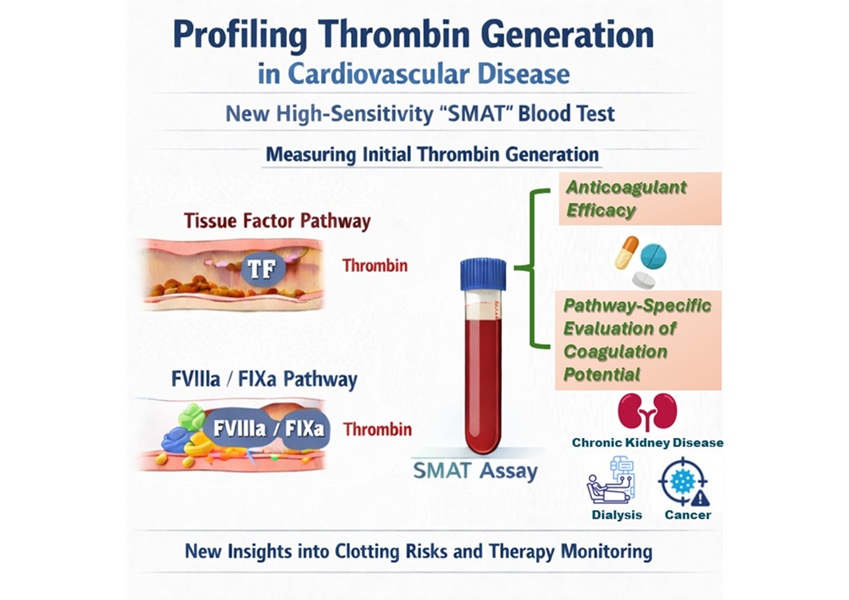
High-Sensitivity Blood Test Improves Assessment of Clotting Risk in Heart Disease Patients
Blood clotting is essential for preventing bleeding, but even small imbalances can lead to serious conditions such as thrombosis or dangerous hemorrhage. In cardiovascular disease, clinicians often struggle... Read moreImmunology
view channelBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read more
Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
Immunotherapy has transformed cancer treatment, but only a small proportion of patients experience lasting benefit, with response rates often remaining between 10% and 20%. Clinicians currently lack reliable... Read moreMicrobiology
view channel
Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
Alzheimer’s disease affects approximately 6.7 million people in the United States and nearly 50 million worldwide, yet early cognitive decline remains difficult to characterize. Increasing evidence suggests... Read moreAI-Powered Platform Enables Rapid Detection of Drug-Resistant C. Auris Pathogens
Infections caused by the pathogenic yeast Candida auris pose a significant threat to hospitalized patients, particularly those with weakened immune systems or those who have invasive medical devices.... Read morePathology
view channel
Engineered Yeast Cells Enable Rapid Testing of Cancer Immunotherapy
Developing new cancer immunotherapies is a slow, costly, and high-risk process, particularly for CAR T cell treatments that must precisely recognize cancer-specific antigens. Small differences in tumor... Read more
First-Of-Its-Kind Test Identifies Autism Risk at Birth
Autism spectrum disorder is treatable, and extensive research shows that early intervention can significantly improve cognitive, social, and behavioral outcomes. Yet in the United States, the average age... Read moreTechnology
view channel
Robotic Technology Unveiled for Automated Diagnostic Blood Draws
Routine diagnostic blood collection is a high‑volume task that can strain staffing and introduce human‑dependent variability, with downstream implications for sample quality and patient experience.... Read more
ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
Clinical laboratories generate billions of test results each year, creating a treasure trove of data with the potential to support more personalized testing, improve operational efficiency, and enhance patient care.... Read moreAptamer Biosensor Technology to Transform Virus Detection
Rapid and reliable virus detection is essential for controlling outbreaks, from seasonal influenza to global pandemics such as COVID-19. Conventional diagnostic methods, including cell culture, antigen... Read more
AI Models Could Predict Pre-Eclampsia and Anemia Earlier Using Routine Blood Tests
Pre-eclampsia and anemia are major contributors to maternal and child mortality worldwide, together accounting for more than half a million deaths each year and leaving millions with long-term health complications.... Read moreIndustry
view channelNew Collaboration Brings Automated Mass Spectrometry to Routine Laboratory Testing
Mass spectrometry is a powerful analytical technique that identifies and quantifies molecules based on their mass and electrical charge. Its high selectivity, sensitivity, and accuracy make it indispensable... Read more
AI-Powered Cervical Cancer Test Set for Major Rollout in Latin America
Noul Co., a Korean company specializing in AI-based blood and cancer diagnostics, announced it will supply its intelligence (AI)-based miLab CER cervical cancer diagnostic solution to Mexico under a multi‑year... Read more
Diasorin and Fisher Scientific Enter into US Distribution Agreement for Molecular POC Platform
Diasorin (Saluggia, Italy) has entered into an exclusive distribution agreement with Fisher Scientific, part of Thermo Fisher Scientific (Waltham, MA, USA), for the LIAISON NES molecular point-of-care... Read more