Gut Microbiome Dysbiosis Linked to COVID-19
Posted on 08 Nov 2022
Previous reports have demonstrated that severe COVID-19 is frequently associated with specific inflammatory immune phenotypes, lymphopenia, and a generally disproportionate immune response leading to systemic organ failure.
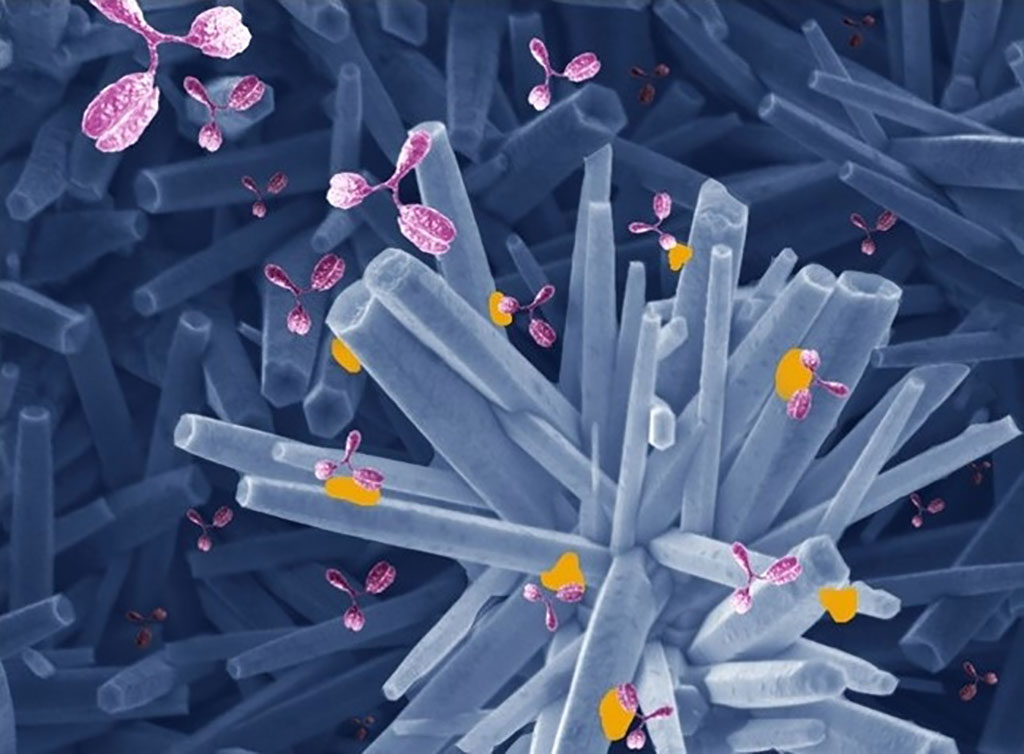
Complex gut microbiota ecosystems can prevent the invasion of potentially pathogenic bacteria. Conversely, when the gut microbiota incurs damage, such as through antibiotics treatment, competitive exclusion of pathogens is weakened and potentially dangerous blooms of antibiotic-resistant bacterial strains can occur.

Medical Microbiologists at the New York University Grossman School of Medicine (New York, NY, USA) and their colleagues demonstrated that SARS-CoV-2 infection induces gut microbiome dysbiosis in mice, which correlated with alterations to Paneth cells and goblet cells, and markers of barrier permeability. They then they analyzed the bacterial composition of stool samples from 96 adults hospitalized with COVID-19 in 2020.
For bacterial DNA extraction 700 µL of SL1 lysis buffer (NucleoSpin Soil kit, Macherey-Nagel, Allentown, PA, USA) was added to the stool samples and tubes were heated at 95 °C for two hours to inactivate SARS-CoV-2. DNA concentration was assessed using a NanoDrop spectrophotometer. Human samples were prepared using KAPA HiFi Polymerase to amplify the V4 region of the 16 S rRNA gene. Libraries were sequenced on a MiSeq (Illumina, San Diego, CA, USA) using paired-end 2 × 250 reads and the MiSeq Reagent Kitv2.
The investigators observed an increase in populations of several microbes known to include antibiotic-resistant species. An analysis of stool samples paired with blood cultures found that antibiotic-resistant bacteria in the gut migrated to the bloodstream in 20% of patients. This migration could be due to a combination of the immune-compromising effects of the viral infection and the antibiotic-driven depletion of commensal gut microbes. The team reported that members of the phyla Firmicutes and Bacteroidetes represented the most abundant bacteria, followed by Proteobacteria.
The authors concluded that their findings support a scenario in which gut-to-blood translocation of microorganisms following microbiome dysbiosis leads to dangerous bloodstream infection during COVID-19, a complication seen in other immunocompromised patients, including patients with cancer, acute respiratory distress syndrome, and in ICU patients receiving probiotics. The study was published November 1, 2022 in the journal Nature Communications.
Related Links:
New York University Grossman School of Medicine
Macherey-Nagel
Illumina