D-Dimer Test Can Still Help Rule Out Pulmonary Embolisms in Hospitalized COVID-19 Patients
|
By LabMedica International staff writers Posted on 27 Oct 2021 |

The D-dimer test can still be helpful in ruling out pulmonary embolisms in hospitalized COVID-19 patients, according to a new study.
Researchers at the University of South Florida Health Morsani College of Medicine (USF Health; Tampa, FL, USA) conducted a single-center, diagnostic study to investigate how well D-dimer testing performed at excluding pulmonary embolism in patients hospitalized with COVID-19. They found that the screening blood test originally validated in seriously ill patients without COVID-19 is still clinically useful for ruling out pulmonary embolism in patients hospitalized with the coronavirus.
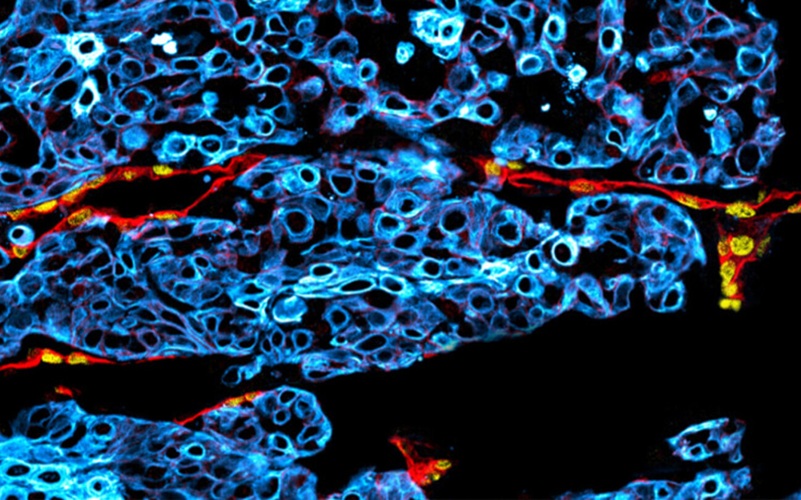
Pulmonary embolisms occur when blood clots that form in another part of the body (often the leg), travel through the bloodstream, and lodge in the blood vessels of the lung, decreasing blood flow and causing low oxygen levels. Research indicates COVID-19 patients are three to 10 times more likely to develop pulmonary embolisms than other hospitalized patients, even when they are not as seriously ill or immobilized. Scientists are still investigating why, but it appears the COVID-19 virus may create a cellular environment that promotes clotting by making the inside of blood vessels uneven, irritated, and prone to microtears.
Doctors who suspect pulmonary embolisms routinely rely on widely available D-dimer screening to rule out the potentially life-threatening blood clotting disorder – most commonly in surgical patients immobilized for long periods and patients admitted to intensive care units. D-dimer is a simple blood test that measures protein fragments of blood clots floating in the bloodstream. D-dimer levels, normally undetectable or detectable at very low levels, rise sharply when the body is breaking down the clots. A negative D-dimer test (one that rules out pulmonary embolism) can help patients avoid more expensive, invasive diagnostic tests, like a computed tomography pulmonary angiogram, or CTPA.
The USF Health researchers wondered if the increased risk for blood clotting in COVID-19 patients, and uncertainty of diverse D-dimer values found in earlier smaller studies, reduced the existing screening tool’s ability to correctly rule out pulmonary embolism in COVID patients. The conventional thinking was that D-dimer levels would almost always be high in COVID-19 patients, therefore the test as originally validated (in non-COVID patients) would not be accurate at differentiating COVID patients without clots.
The restrospective study looked at the records of 1,541 patients hospitalized with COVID-19 at Tampa General Hospital from Jan. 1, 2020, to Feb. 5, 2021. They compared plasma D-dimer concentrations with CTPA, the criterion for diagnosing pulmonary embolism, in 287 of those patients. All COVID-19 patients with CTPA evidence of pulmonary embolism had D-dimer levels of 0.05 μg/mL or greater, as did the majority (91.2%) of patients without CTPA evidence of pulmonary embolism. (Concentrations of 0.05 μg/mL and higher are considered positive for pulmonary embolism, while anything below that D-dimer level is negative). The researchers also analyzed whether changing the cutoff levels defining positive or negative D-dimer test results specifically for the COVID patient population might improve the test’s performance.
Within the limitations of this single-center study, setting higher D-dimer thresholds was associated with improved specificity – but at “the cost of an increased false-negative rate that could be associated with an unacceptable patient safety risk,” the study authors wrote. A false-negative result means that the test does not detect a pulmonary embolism when the serious blood clotting problem is very likely present. While clinicians must maintain heightened suspicion for pulmonary embolisms when evaluating symptoms in COVID-19 patients, the overall USF Health study results indicate that the currently available D-dimer test adequately screens for the likelihood of pulmonary embolism in hospitalized COVID patients.
“Our study found that clinicians can feel confident interpreting the D-dimer levels the same in COVID patients as they do in every other patient; we don’t need a special (different) value for COVID patients,” said principal investigator Asa Oxner, MD, associate professor and vice chair of USF Health Internal Medicine. “So, in hospitalized COVID patients, we can appropriately rule out a pulmonary embolism if d-dimer levels are low.”
“The mechanisms of developing pulmonary embolisms may differ for COVID patients, but the resulting physiology is the same for all patients. The little fragments of (undissolved) blood clots are still detectable with D-dimer,” said Oxner.
Related Links:
USF Health
Latest COVID-19 News
- New Immunosensor Paves Way to Rapid POC Testing for COVID-19 and Emerging Infectious Diseases
- Long COVID Etiologies Found in Acute Infection Blood Samples
- Novel Device Detects COVID-19 Antibodies in Five Minutes
- CRISPR-Powered COVID-19 Test Detects SARS-CoV-2 in 30 Minutes Using Gene Scissors
- Gut Microbiome Dysbiosis Linked to COVID-19
- Novel SARS CoV-2 Rapid Antigen Test Validated for Diagnostic Accuracy
- New COVID + Flu + R.S.V. Test to Help Prepare for `Tripledemic`
- AI Takes Guesswork Out Of Lateral Flow Testing
- Fastest Ever SARS-CoV-2 Antigen Test Designed for Non-Invasive COVID-19 Testing in Any Setting
- Rapid Antigen Tests Detect Omicron, Delta SARS-CoV-2 Variants
- Health Care Professionals Showed Increased Interest in POC Technologies During Pandemic, Finds Study
- Set Up Reserve Lab Capacity Now for Faster Response to Next Pandemic, Say Researchers
- Blood Test Performed During Initial Infection Predicts Long COVID Risk
- Low-Cost COVID-19 Testing Platform Combines Sensitivity of PCR and Speed of Antigen Tests
- Finger-Prick Blood Test Identifies Immunity to COVID-19
- Quick Test Kit Determines Immunity Against COVID-19 and Its Variants
Channels
Clinical Chemistry
view channel
Simple Blood Test Offers New Path to Alzheimer’s Assessment in Primary Care
Timely evaluation of cognitive symptoms in primary care is often limited by restricted access to specialized diagnostics and invasive confirmatory procedures. Clinicians need accessible tools to determine... Read more
Existing Hospital Analyzers Can Identify Fake Liquid Medical Products
Counterfeit and substandard medicines remain a serious global health threat, with World Health Organization estimates suggesting that 10.5% of medicines in low- and middle-income countries are either fake... Read moreMolecular Diagnostics
view channel
Genetic Test Aids Early Detection and Improved Treatment for Cancers
Lynch syndrome is a hereditary genetic condition that significantly increases the risk of several cancers, including those of the bowel and urinary tract. Urinary tract cancers—affecting the kidney, bladder,... Read more
New Genome Sequencing Technique Measures Epstein-Barr Virus in Blood
The Epstein–Barr virus (EBV) infects up to 95% of adults worldwide and remains in the body for life. While usually kept under control, the virus is linked to cancers such as Hodgkin’s lymphoma and autoimmune... Read moreHematology
view channel
Rapid Cartridge-Based Test Aims to Expand Access to Hemoglobin Disorder Diagnosis
Sickle cell disease and beta thalassemia are hemoglobin disorders that often require referral to specialized laboratories for definitive diagnosis, delaying results for patients and clinicians.... Read more
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read moreImmunology
view channel
New Biomarker Predicts Chemotherapy Response in Triple-Negative Breast Cancer
Triple-negative breast cancer is an aggressive form of breast cancer in which patients often show widely varying responses to chemotherapy. Predicting who will benefit from treatment remains challenging,... Read moreBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read more
Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
Immunotherapy has transformed cancer treatment, but only a small proportion of patients experience lasting benefit, with response rates often remaining between 10% and 20%. Clinicians currently lack reliable... Read moreMicrobiology
view channel
Three-Test Panel Launched for Detection of Liver Fluke Infections
Parasitic liver fluke infections remain endemic in parts of Asia, where transmission commonly occurs through consumption of raw freshwater fish or aquatic plants. Chronic infection is a well-established... Read more
Rapid Test Promises Faster Answers for Drug-Resistant Infections
Drug-resistant pathogens continue to pose a growing threat in healthcare facilities, where delayed detection can impede outbreak control and increase mortality. Candida auris is notoriously difficult to... Read more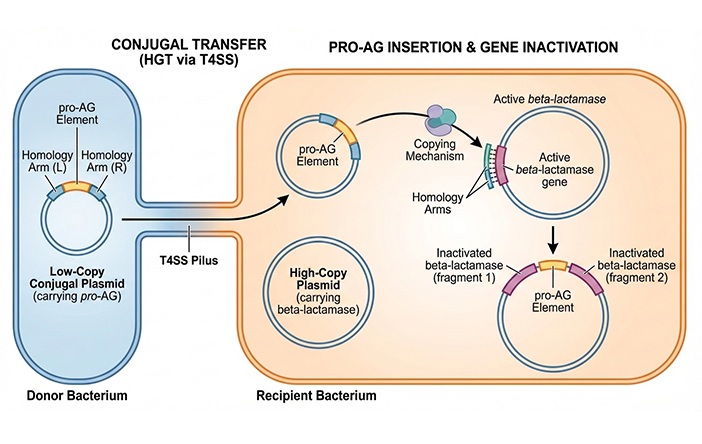
CRISPR-Based Technology Neutralizes Antibiotic-Resistant Bacteria
Antibiotic resistance has accelerated into a global health crisis, with projections estimating more than 10 million deaths per year by 2050 as drug-resistant “superbugs” continue to spread.... Read more
Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
Alzheimer’s disease affects approximately 6.7 million people in the United States and nearly 50 million worldwide, yet early cognitive decline remains difficult to characterize. Increasing evidence suggests... Read morePathology
view channel
AI-Powered 3D Scanning System Speeds Cancer Screening
Cytology remains a cornerstone of cancer detection, requiring specialists to examine bodily fluids and cells under a microscope. This labor-intensive process involves inspecting up to one million cells... Read more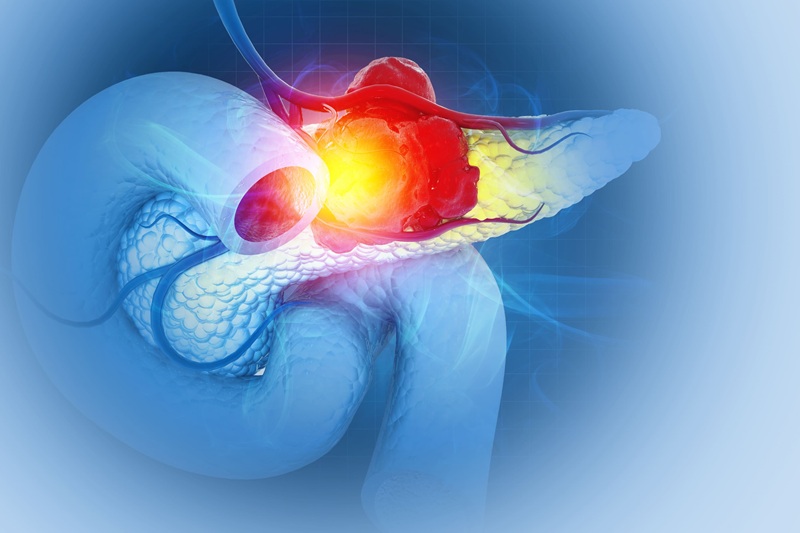
Single Sample Classifier Predicts Cancer-Associated Fibroblast Subtypes in Patient Samples
Pancreatic ductal adenocarcinoma (PDAC) remains one of the deadliest cancers, in part because of its dense tumor microenvironment that influences how tumors grow and respond to treatment.... Read more
New AI-Driven Platform Standardizes Tuberculosis Smear Microscopy Workflow
Sputum smear microscopy remains central to tuberculosis treatment monitoring and follow-up, particularly in high‑burden settings where serial testing is routine. Yet consistent, repeatable bacillary assessment... Read more
AI Tool Uses Blood Biomarkers to Predict Transplant Complications Before Symptoms Appear
Stem cell and bone marrow transplants can be lifesaving, but serious complications may arise months after patients leave the hospital. One of the most dangerous is chronic graft-versus-host disease, in... Read moreTechnology
view channel
Blood Test “Clocks” Predict Start of Alzheimer’s Symptoms
More than 7 million Americans live with Alzheimer’s disease, and related health and long-term care costs are projected to reach nearly USD 400 billion in 2025. The disease has no cure, and symptoms often... Read more
AI-Powered Biomarker Predicts Liver Cancer Risk
Liver cancer, or hepatocellular carcinoma, causes more than 800,000 deaths worldwide each year and often goes undetected until late stages. Even after treatment, recurrence rates reach 70% to 80%, contributing... Read more
Robotic Technology Unveiled for Automated Diagnostic Blood Draws
Routine diagnostic blood collection is a high‑volume task that can strain staffing and introduce human‑dependent variability, with downstream implications for sample quality and patient experience.... Read more
ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
Clinical laboratories generate billions of test results each year, creating a treasure trove of data with the potential to support more personalized testing, improve operational efficiency, and enhance patient care.... Read moreIndustry
view channel
QuidelOrtho Collaborates with Lifotronic to Expand Global Immunoassay Portfolio
QuidelOrtho (San Diego, CA, USA) has entered a long-term strategic supply agreement with Lifotronic Technology (Shenzhen, China) to expand its global immunoassay portfolio and accelerate customer access... Read more