New Miniature Device to Transform Testing of Blood Cancer Treatments
Posted on 02 Jul 2025
Chimeric antigen receptor (CAR) T cell therapy has emerged as a groundbreaking treatment for blood cancers like leukemia, offering hope to patients when other treatments fail. However, despite its promise, nearly half of leukemia patients relapse, and many suffer from serious side effects. Efforts to improve CAR T therapies have been hampered by the limitations of conventional testing methods. Traditional models fail to accurately replicate the complex human immune response and the bone marrow environment where leukemia develops. Now, researchers have developed a new solution to bridge this gap—a platform that allows for real-time observation of cancer treatment interactions under controlled conditions, offering a more accurate and patient-specific approach to testing blood cancer therapies.
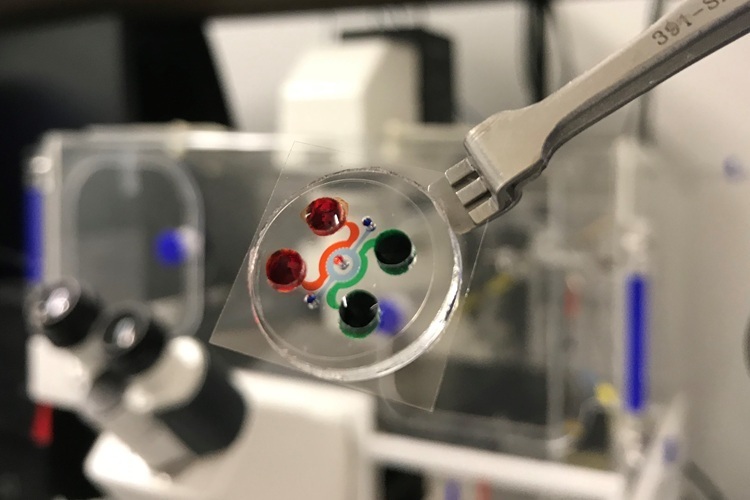
This innovative platform, termed “leukemia-on-a-chip,” was developed through a collaboration between the Perelman School of Medicine at the University of Pennsylvania (Philadelphia, PA, USA) and the Tandon School of Engineering at New York University (Brooklyn, NY, USA). The device is the first to successfully recreate the physical and immunological environment of human bone marrow on a microscope slide-sized chip. It integrates three distinct bone marrow regions—blood vessels, surrounding marrow cavity, and the outer bone lining—and when seeded with patient-derived cells, it self-organizes to produce structural proteins such as collagen, fibronectin, and laminin. Importantly, the device preserves the immune cell activity within the marrow microenvironment. The system incorporates vascular networks to simulate realistic immune interactions in three dimensions, providing a level of insight and accuracy far beyond 2D cultures or animal models. The development is also timely, coinciding with the FDA’s new roadmap to reduce animal testing requirements in drug development.
In their study published in Nature Biomedical Engineering, the researchers used advanced imaging to watch CAR T cells move through blood vessels, detect cancer cells, and destroy them—processes previously impossible to view with this clarity. They observed that engineered immune cells not only targeted leukemia cells but also activated other immune cells nearby in a “bystander effect” that may explain both therapeutic success and some side effects. The team simulated different patient responses, including remission, relapse, and resistance, and demonstrated that newer, fourth-generation CAR T cells performed better than standard versions, even at lower doses. The chip setup takes just half a day to assemble and supports experiments for up to two weeks, in contrast to animal models that require months. Going forward, the researchers aim to use this platform to test individual patient cancer cells against various treatment designs, enabling a personalized approach to therapy selection before treatment begins.
Related Links:
Perelman School of Medicine
Tandon School of Engineering














