Low-Cost Tabletop Device Detects SARS-CoV-2 Variants from Saliva Sample in an Hour
|
By LabMedica International staff writers Posted on 11 Aug 2021 |

Illustration
Researchers have created an inexpensive, CRISPR-based diagnostic test that allows users to test themselves for SARS-CoV-2 and multiple variants of the virus using a sample of their saliva at home, with no extra instrumentation needed.
The diagnostic device, called Minimally Instrumented SHERLOCK (miSHERLOCK), has been developed by researchers at the Wyss Institute for Biologically Inspired Engineering at Harvard University (Boston, MA, USA) and the Massachusetts Institute of Technology (MIT; Cambridge, MA, USA). It is easy to use and provides results that can be read and verified by an accompanying smartphone app within one hour. It successfully distinguished between three different variants of SARS-CoV-2 in experiments, and can be rapidly reconfigured to detect additional variants like Delta. The device can be assembled using a 3D printer and commonly available components for about USD 15, and re-using the hardware brings the cost of individual assays down to USD 6 each.
For the SARS-CoV-2 detection piece of their diagnostic, the researchers turned to a CRISPR-based technology created in the lab of Wyss Core Faculty member and senior paper author Jim Collins, Ph.D. called “specific high sensitivity enzymatic reporter unlocking” (SHERLOCK). SHERLOCK makes use of CRISPR’s “molecular scissors” to snip DNA or RNA at specific locations, with an added bonus: upon recognizing its target sequence, this specific type of scissors also cuts other pieces of DNA in the surrounding area, allowing it to be engineered to produce a signal indicating that the target has been successfully cut.
The researchers created a SHERLOCK reaction designed to cut SARS-CoV-2 RNA at a specific region of a gene called Nucleoprotein that is conserved across multiple variants of the virus. When the molecular scissors – an enzyme called Cas12a – successfully binds to and cuts the Nucleoprotein gene, single-stranded DNA probes are also cut, producing a fluorescent signal. They also created additional SHERLOCK assays designed to target a panel of viral mutations in Spike protein sequences that represent three SARS-CoV-2 genetic variants: Alpha, Beta, and Gamma.
Armed with assays that could reliably detect viral RNA within the accepted concentration range for FDA-authorized diagnostic tests, the team next focused their efforts on solving what is arguably the most difficult challenge in diagnostics: sample preparation. The team chose to use saliva rather than nasopharyngeal swab samples as their diagnostic source material, because it’s easier for users to collect saliva and studies have shown that SARS-CoV-2 is detectable in saliva for a greater number of days post-infection. But unprocessed saliva presents challenges of its own: it contains enzymes that degrade various molecules, producing a high rate of false positives.
The researchers developed a novel technique to solve that problem. First, they added two chemicals called DTT and EGTA to saliva and heated the sample to 95°C for three minutes, deactivated the enzymes producing the false positive signal from the untreated saliva and sliced open any viral particles. They then incorporated a porous membrane that was engineered to trap RNA on its surface, which could finally be added directly to the SHERLOCK reaction to generate a result.
To integrate the saliva sample preparation and the SHERLOCK reaction into one diagnostic, the team designed a simple battery-powered device with two chambers: a heated sample preparation chamber, and an unheated reaction chamber. A user spits into the sample preparation chamber, turns on the heat, and waits three to six minutes for the saliva to be wicked into the filter. The user removes the filter and transfers it to the reaction chamber column, then pushes a plunger that deposits the filter into the chamber and punctures a water reservoir to activate the SHERLOCK reaction. 55 minutes later, the user looks through the tinted transilluminator window into the reaction chamber and confirms the presence of a fluorescent signal. They can also use an accompanying smartphone app that analyzes the pixels being registered by the smartphone’s camera to provide a clear positive or negative diagnosis.
The researchers tested their diagnostic device using clinical saliva samples from 27 COVID-19 patients and 21 healthy patients, and found that miSHERLOCK correctly identified COVID-19-positive patients 96% of the time and patients without the disease 95% of the time. They also tested its performance against the Alpha, Beta, and Gamma SARS-CoV-2 variants by spiking healthy human saliva with full-length synthetic viral RNA containing mutations representing each variant, and found that the device was effective across a range of viral RNA concentrations.
“One of the great things about miSHERLOCK is that it’s entirely modular. The device itself is separate from the assays, so you can plug in different assays for the specific sequence of RNA or DNA you’re trying to detect,” said co-first author Devora Najjar, a Research Assistant at the MIT Media Lab and in the Collins Lab. “The device costs about $15, but mass production would bring the housing costs down to about $3. Assays for new targets can be created in about two weeks, enabling the rapid development of tests for new variants of SARS-CoV-2 as well as for other infectious diseases.”
“miSHERLOCK eliminates the need to transport patient samples to a centralized testing location and greatly simplifies the sample preparation steps, giving patients and doctors a faster, more accurate picture of individual and community health, which is critical during an evolving pandemic,” said co-first author Helena de Puig, Ph.D., a Postdoctoral Fellow at the Wyss Institute and MIT.
Related Links:
Wyss Institute for Biologically Inspired Engineering at Harvard University
Massachusetts Institute of Technology
The diagnostic device, called Minimally Instrumented SHERLOCK (miSHERLOCK), has been developed by researchers at the Wyss Institute for Biologically Inspired Engineering at Harvard University (Boston, MA, USA) and the Massachusetts Institute of Technology (MIT; Cambridge, MA, USA). It is easy to use and provides results that can be read and verified by an accompanying smartphone app within one hour. It successfully distinguished between three different variants of SARS-CoV-2 in experiments, and can be rapidly reconfigured to detect additional variants like Delta. The device can be assembled using a 3D printer and commonly available components for about USD 15, and re-using the hardware brings the cost of individual assays down to USD 6 each.
For the SARS-CoV-2 detection piece of their diagnostic, the researchers turned to a CRISPR-based technology created in the lab of Wyss Core Faculty member and senior paper author Jim Collins, Ph.D. called “specific high sensitivity enzymatic reporter unlocking” (SHERLOCK). SHERLOCK makes use of CRISPR’s “molecular scissors” to snip DNA or RNA at specific locations, with an added bonus: upon recognizing its target sequence, this specific type of scissors also cuts other pieces of DNA in the surrounding area, allowing it to be engineered to produce a signal indicating that the target has been successfully cut.
The researchers created a SHERLOCK reaction designed to cut SARS-CoV-2 RNA at a specific region of a gene called Nucleoprotein that is conserved across multiple variants of the virus. When the molecular scissors – an enzyme called Cas12a – successfully binds to and cuts the Nucleoprotein gene, single-stranded DNA probes are also cut, producing a fluorescent signal. They also created additional SHERLOCK assays designed to target a panel of viral mutations in Spike protein sequences that represent three SARS-CoV-2 genetic variants: Alpha, Beta, and Gamma.
Armed with assays that could reliably detect viral RNA within the accepted concentration range for FDA-authorized diagnostic tests, the team next focused their efforts on solving what is arguably the most difficult challenge in diagnostics: sample preparation. The team chose to use saliva rather than nasopharyngeal swab samples as their diagnostic source material, because it’s easier for users to collect saliva and studies have shown that SARS-CoV-2 is detectable in saliva for a greater number of days post-infection. But unprocessed saliva presents challenges of its own: it contains enzymes that degrade various molecules, producing a high rate of false positives.
The researchers developed a novel technique to solve that problem. First, they added two chemicals called DTT and EGTA to saliva and heated the sample to 95°C for three minutes, deactivated the enzymes producing the false positive signal from the untreated saliva and sliced open any viral particles. They then incorporated a porous membrane that was engineered to trap RNA on its surface, which could finally be added directly to the SHERLOCK reaction to generate a result.
To integrate the saliva sample preparation and the SHERLOCK reaction into one diagnostic, the team designed a simple battery-powered device with two chambers: a heated sample preparation chamber, and an unheated reaction chamber. A user spits into the sample preparation chamber, turns on the heat, and waits three to six minutes for the saliva to be wicked into the filter. The user removes the filter and transfers it to the reaction chamber column, then pushes a plunger that deposits the filter into the chamber and punctures a water reservoir to activate the SHERLOCK reaction. 55 minutes later, the user looks through the tinted transilluminator window into the reaction chamber and confirms the presence of a fluorescent signal. They can also use an accompanying smartphone app that analyzes the pixels being registered by the smartphone’s camera to provide a clear positive or negative diagnosis.
The researchers tested their diagnostic device using clinical saliva samples from 27 COVID-19 patients and 21 healthy patients, and found that miSHERLOCK correctly identified COVID-19-positive patients 96% of the time and patients without the disease 95% of the time. They also tested its performance against the Alpha, Beta, and Gamma SARS-CoV-2 variants by spiking healthy human saliva with full-length synthetic viral RNA containing mutations representing each variant, and found that the device was effective across a range of viral RNA concentrations.
“One of the great things about miSHERLOCK is that it’s entirely modular. The device itself is separate from the assays, so you can plug in different assays for the specific sequence of RNA or DNA you’re trying to detect,” said co-first author Devora Najjar, a Research Assistant at the MIT Media Lab and in the Collins Lab. “The device costs about $15, but mass production would bring the housing costs down to about $3. Assays for new targets can be created in about two weeks, enabling the rapid development of tests for new variants of SARS-CoV-2 as well as for other infectious diseases.”
“miSHERLOCK eliminates the need to transport patient samples to a centralized testing location and greatly simplifies the sample preparation steps, giving patients and doctors a faster, more accurate picture of individual and community health, which is critical during an evolving pandemic,” said co-first author Helena de Puig, Ph.D., a Postdoctoral Fellow at the Wyss Institute and MIT.
Related Links:
Wyss Institute for Biologically Inspired Engineering at Harvard University
Massachusetts Institute of Technology
Latest COVID-19 News
- New Immunosensor Paves Way to Rapid POC Testing for COVID-19 and Emerging Infectious Diseases
- Long COVID Etiologies Found in Acute Infection Blood Samples
- Novel Device Detects COVID-19 Antibodies in Five Minutes
- CRISPR-Powered COVID-19 Test Detects SARS-CoV-2 in 30 Minutes Using Gene Scissors
- Gut Microbiome Dysbiosis Linked to COVID-19
- Novel SARS CoV-2 Rapid Antigen Test Validated for Diagnostic Accuracy
- New COVID + Flu + R.S.V. Test to Help Prepare for `Tripledemic`
- AI Takes Guesswork Out Of Lateral Flow Testing
- Fastest Ever SARS-CoV-2 Antigen Test Designed for Non-Invasive COVID-19 Testing in Any Setting
- Rapid Antigen Tests Detect Omicron, Delta SARS-CoV-2 Variants
- Health Care Professionals Showed Increased Interest in POC Technologies During Pandemic, Finds Study
- Set Up Reserve Lab Capacity Now for Faster Response to Next Pandemic, Say Researchers
- Blood Test Performed During Initial Infection Predicts Long COVID Risk
- Low-Cost COVID-19 Testing Platform Combines Sensitivity of PCR and Speed of Antigen Tests
- Finger-Prick Blood Test Identifies Immunity to COVID-19
- Quick Test Kit Determines Immunity Against COVID-19 and Its Variants
Channels
Clinical Chemistry
view channel
New PSA-Based Prognostic Model Improves Prostate Cancer Risk Assessment
Prostate cancer is the second-leading cause of cancer death among American men, and about one in eight will be diagnosed in their lifetime. Screening relies on blood levels of prostate-specific antigen... Read more
Extracellular Vesicles Linked to Heart Failure Risk in CKD Patients
Chronic kidney disease (CKD) affects more than 1 in 7 Americans and is strongly associated with cardiovascular complications, which account for more than half of deaths among people with CKD.... Read moreMolecular Diagnostics
view channel
Diagnostic Device Predicts Treatment Response for Brain Tumors Via Blood Test
Glioblastoma is one of the deadliest forms of brain cancer, largely because doctors have no reliable way to determine whether treatments are working in real time. Assessing therapeutic response currently... Read more
Blood Test Detects Early-Stage Cancers by Measuring Epigenetic Instability
Early-stage cancers are notoriously difficult to detect because molecular changes are subtle and often missed by existing screening tools. Many liquid biopsies rely on measuring absolute DNA methylation... Read more
“Lab-On-A-Disc” Device Paves Way for More Automated Liquid Biopsies
Extracellular vesicles (EVs) are tiny particles released by cells into the bloodstream that carry molecular information about a cell’s condition, including whether it is cancerous. However, EVs are highly... Read more
Blood Test Identifies Inflammatory Breast Cancer Patients at Increased Risk of Brain Metastasis
Brain metastasis is a frequent and devastating complication in patients with inflammatory breast cancer, an aggressive subtype with limited treatment options. Despite its high incidence, the biological... Read moreHematology
view channel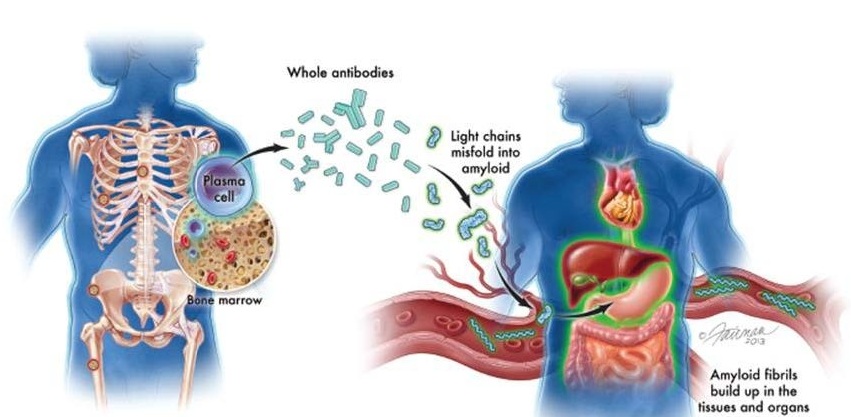
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read more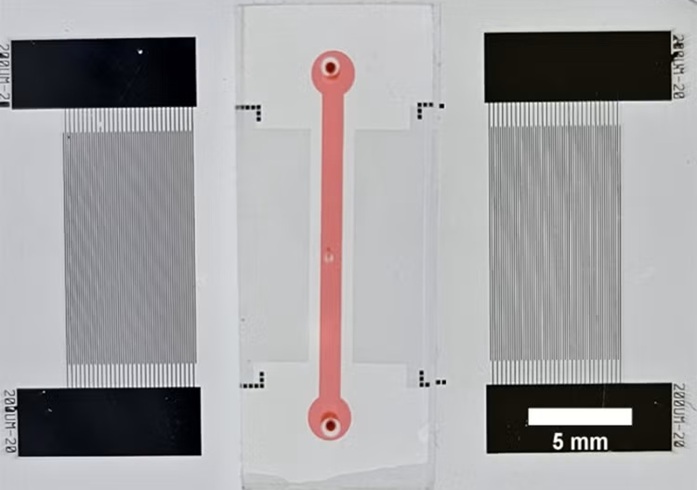
Fast and Easy Test Could Revolutionize Blood Transfusions
Blood transfusions are a cornerstone of modern medicine, yet red blood cells can deteriorate quietly while sitting in cold storage for weeks. Although blood units have a fixed expiration date, cells from... Read more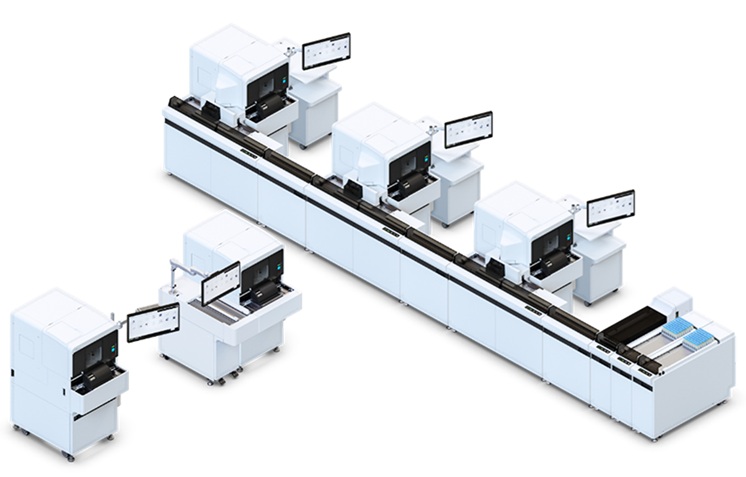
Automated Hemostasis System Helps Labs of All Sizes Optimize Workflow
High-volume hemostasis sections must sustain rapid turnaround while managing reruns and reflex testing. Manual tube handling and preanalytical checks can strain staff time and increase opportunities for error.... Read more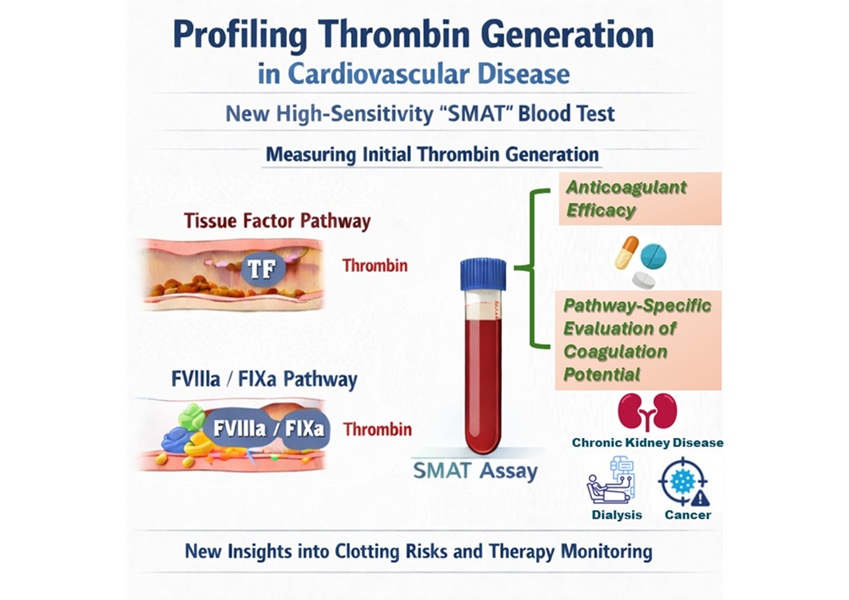
High-Sensitivity Blood Test Improves Assessment of Clotting Risk in Heart Disease Patients
Blood clotting is essential for preventing bleeding, but even small imbalances can lead to serious conditions such as thrombosis or dangerous hemorrhage. In cardiovascular disease, clinicians often struggle... Read moreImmunology
view channelBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read more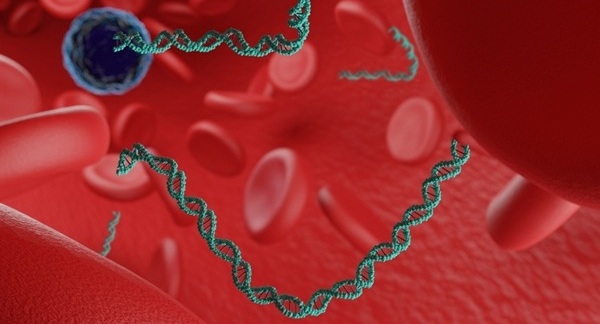
Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
Immunotherapy has transformed cancer treatment, but only a small proportion of patients experience lasting benefit, with response rates often remaining between 10% and 20%. Clinicians currently lack reliable... Read moreMicrobiology
view channel
Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
Alzheimer’s disease affects approximately 6.7 million people in the United States and nearly 50 million worldwide, yet early cognitive decline remains difficult to characterize. Increasing evidence suggests... Read moreAI-Powered Platform Enables Rapid Detection of Drug-Resistant C. Auris Pathogens
Infections caused by the pathogenic yeast Candida auris pose a significant threat to hospitalized patients, particularly those with weakened immune systems or those who have invasive medical devices.... Read morePathology
view channel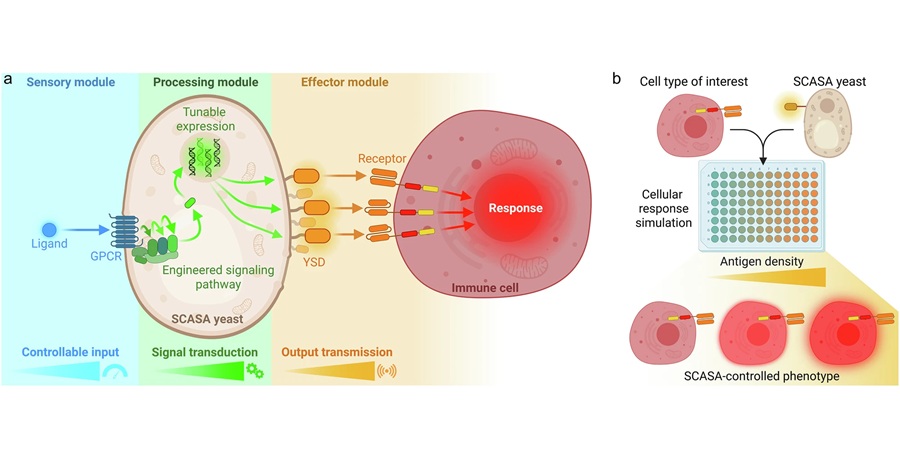
Engineered Yeast Cells Enable Rapid Testing of Cancer Immunotherapy
Developing new cancer immunotherapies is a slow, costly, and high-risk process, particularly for CAR T cell treatments that must precisely recognize cancer-specific antigens. Small differences in tumor... Read more
First-Of-Its-Kind Test Identifies Autism Risk at Birth
Autism spectrum disorder is treatable, and extensive research shows that early intervention can significantly improve cognitive, social, and behavioral outcomes. Yet in the United States, the average age... Read moreTechnology
view channel
Robotic Technology Unveiled for Automated Diagnostic Blood Draws
Routine diagnostic blood collection is a high‑volume task that can strain staffing and introduce human‑dependent variability, with downstream implications for sample quality and patient experience.... Read more
ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
Clinical laboratories generate billions of test results each year, creating a treasure trove of data with the potential to support more personalized testing, improve operational efficiency, and enhance patient care.... Read moreAptamer Biosensor Technology to Transform Virus Detection
Rapid and reliable virus detection is essential for controlling outbreaks, from seasonal influenza to global pandemics such as COVID-19. Conventional diagnostic methods, including cell culture, antigen... Read more
AI Models Could Predict Pre-Eclampsia and Anemia Earlier Using Routine Blood Tests
Pre-eclampsia and anemia are major contributors to maternal and child mortality worldwide, together accounting for more than half a million deaths each year and leaving millions with long-term health complications.... Read moreIndustry
view channelNew Collaboration Brings Automated Mass Spectrometry to Routine Laboratory Testing
Mass spectrometry is a powerful analytical technique that identifies and quantifies molecules based on their mass and electrical charge. Its high selectivity, sensitivity, and accuracy make it indispensable... Read more
AI-Powered Cervical Cancer Test Set for Major Rollout in Latin America
Noul Co., a Korean company specializing in AI-based blood and cancer diagnostics, announced it will supply its intelligence (AI)-based miLab CER cervical cancer diagnostic solution to Mexico under a multi‑year... Read more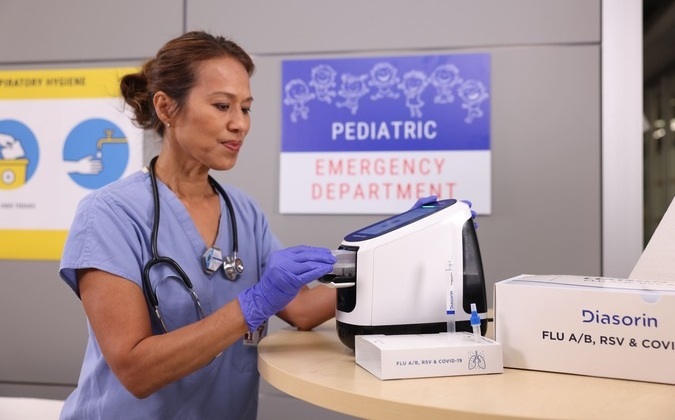
Diasorin and Fisher Scientific Enter into US Distribution Agreement for Molecular POC Platform
Diasorin (Saluggia, Italy) has entered into an exclusive distribution agreement with Fisher Scientific, part of Thermo Fisher Scientific (Waltham, MA, USA), for the LIAISON NES molecular point-of-care... Read more