Stem Cell Test Predicts Treatment Outcome for Patients with Platinum-Resistant Ovarian Cancer
Posted on 09 Apr 2025
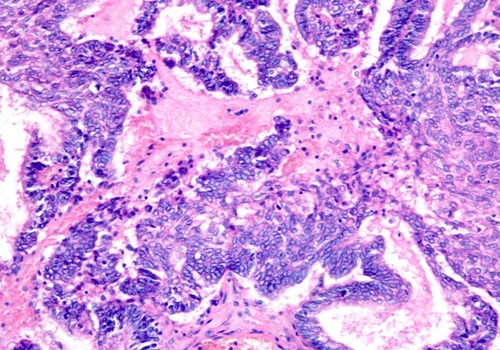
Epithelial ovarian cancer frequently responds to chemotherapy initially, but eventually, the tumor develops resistance to the therapy, leading to regrowth. This resistance is partially due to the activation and selection of cancer stem cells (CSCs) that repair and rebuild the tumor after chemotherapy damage. New findings from a Phase 3 trial, published in the journal npj Precision Oncology, reveal that a test for cancer stem cells can help identify more effective treatments and improve outcomes for patients with platinum-resistant ovarian cancer (those who experience recurrence within six months after receiving platinum-based chemotherapy).
The ChemoID platform, developed by researchers at the University of Cincinnati (Cincinnati, OH, USA), works by testing cancer stem cells found in individual patients' tumors against specific anticancer drugs to determine the most effective treatment options. The platform operates under the premise that by evaluating both tumor cells and cancer stem cells for chemosensitivity, one can target and eliminate CSCs that could otherwise repopulate the tumor. In the trial, 81 patients with platinum-resistant ovarian cancer were randomly assigned to have their chemotherapy treatment chosen using the ChemoID platform or based on the physician's standard methods. Physicians typically select treatments based on approved therapies, their previous experiences, past treatments the patient has undergone, and the side effects or toxicity that the patient has previously experienced.
The primary outcome measured was the patients’ objective response rate (ORR), which refers to the percentage of patients in each group who achieved either a partial or complete response to the treatment within a designated period. In addition, progression-free survival (PFS)—the duration of time a patient lives without the cancer worsening during and after treatment—and the duration of the response were measured. Results showed that patients who were treated using the ChemoID assay had significantly better clinical and statistical outcomes compared to those who received the physician’s choice of therapy. The ORR for patients in the ChemoID group was 50%, while only 5% of patients in the physician-choice group responded positively.
Median PFS for patients in the ChemoID group was 11 months, compared to only three months in the physician-choice group. Furthermore, patients in the ChemoID group had a median duration of response of eight months, whereas those in the physician-choice group experienced just five-and-a-half months. These improved response rates could potentially reduce healthcare costs associated with ineffective therapies and unnecessary toxicity, according to researchers.
The findings from this study suggest that using assay-guided treatment approaches could reduce financial toxicity for ovarian cancer patients, particularly those with platinum-resistant disease who often struggle with treatment decisions. Future studies are needed to further validate the ChemoID platform and explore how it works with different molecular subgroups, such as patients with BRCA mutations. Additionally, the testing of emerging biologic therapies will help refine the best uses for this test.