COVID-19 Group Testing Method Delivers Results 13 Times Faster than Individual Testing of Each Sample
|
By LabMedica International staff writers Posted on 30 Mar 2021 |

Illustration
A new group method of testing for COVID-19 allows results to be obtained 13 times faster as compared to individual testing of each sample.
The new method developed by researchers from the HSE Laboratory of Algorithms and Technologies for Networks Analysis (Nizhny Novgorod, Russia) and Vilnius University (Vilnius, Lithuania) can be used for asymptomatic populations with seemingly low incidence of coronavirus cases, where it will help detect the infected individuals at a maximum speed with a minimum number of tests, and timely apply the quarantine measures in order to prevent spreading of the disease.
Present COVID-19 testing solutions are based on the extraction of RNA from patients using oropharyngeal and nasopharyngeal swabs, and then testing with real-time PCR for the presence of specific RNA filaments identifying the virus. The speed of this approach is limited by the availability of reactants, trained technicians and laboratories. One way to speed up the testing procedures is group testing, where the swabs of multiple patients are grouped together and tested. The swabs from groups that return a positive result are then tested individually in order to detect specific COVID-19 positive patients. This approach helps decrease the number of tests twofold or more (depending on the spread of the disease) as compared to individual testing of each swab.
For example, suppose 96 samples should be tested and pools of up to 12 samples are possible. In individual testing, 96 tests are necessary. In pool testing, 8 pools of 12 samples are taken and testing is performed. If the result of one pool is positive, then additional 12 individual tests are needed. If two or three groups return a positive result, 24 or 36 additional tests are required, which, together with the first eight tests, will mean a decrease in the number of tests from two to five times as compared to individual testing. The researchers believe that the number of tests can be decreased by optimizing the size of groups that takes into account the total number of swabs and the forecasted number of infected individuals. As the number of infected individuals increases, the possibility of saving swabs decreases but is still about 40% in the event of an incidence of 100 positive samples per 1,000, and 18% for an incidence of 200 per 1,000.
There are ways to optimize group testing, such as choosing the optimal group size based on the total number of swabs and the projected level of disease spreading. Another is the binary splitting method, in which a positive group is split into halves and is tested again, until individual positive swabs are detected. The second method, however, is very time-consuming, which decreases its attractiveness during a pandemic. In addition, to optimize group testing, transposition-based replication is used: after grouping the swabs, researchers form additional control groups from the same swabs and test them together with the main groups. This helps further cut the number of tests, and if the disease levels are low, it also helps to detect positive swabs in one step, which speeds up the testing considerably.
However, this method does not allow for experimenting with group sizes to detect the optimal group size under specific conditions. Researchers from HSE University and Vilnius University suggested OptReplica technology, which uses a more complicated algorithm of swab grouping in key and control groups and helps decrease the number of control groups. In addition, the algorithm helps calculate the optimal group size for the present number of swabs and the forecasted level of disease spreading. The researchers conducted experimental research on samples of 96 and 384 swabs, carrying out 100 randomized tests for each sample size, and compared the effectiveness of transposition-based replication and OptReplica method for different levels of disease incidence. The studies have shown that if the optimal size of groups is chosen, OptReplica is more effective than transposition-based replication. In cases with low incidence, the use of OptReplica, a 13x average reduction of tests can be achieved compared to individual testing without time delay.
“Our simulations are actually proving that using this optimization replication strategy is always advantageous and, even in case of high spread of the disease (10% or 20% of positives in the population), we are still competitive with individual testing strategy,” explained Mario Guarracino, Chief Research Fellow of the Laboratory of Algorithms and Technologies for Networks Analysis.
Related Links:
HSE Laboratory of Algorithms and Technologies for Networks Analysis
Vilnius University
The new method developed by researchers from the HSE Laboratory of Algorithms and Technologies for Networks Analysis (Nizhny Novgorod, Russia) and Vilnius University (Vilnius, Lithuania) can be used for asymptomatic populations with seemingly low incidence of coronavirus cases, where it will help detect the infected individuals at a maximum speed with a minimum number of tests, and timely apply the quarantine measures in order to prevent spreading of the disease.
Present COVID-19 testing solutions are based on the extraction of RNA from patients using oropharyngeal and nasopharyngeal swabs, and then testing with real-time PCR for the presence of specific RNA filaments identifying the virus. The speed of this approach is limited by the availability of reactants, trained technicians and laboratories. One way to speed up the testing procedures is group testing, where the swabs of multiple patients are grouped together and tested. The swabs from groups that return a positive result are then tested individually in order to detect specific COVID-19 positive patients. This approach helps decrease the number of tests twofold or more (depending on the spread of the disease) as compared to individual testing of each swab.
For example, suppose 96 samples should be tested and pools of up to 12 samples are possible. In individual testing, 96 tests are necessary. In pool testing, 8 pools of 12 samples are taken and testing is performed. If the result of one pool is positive, then additional 12 individual tests are needed. If two or three groups return a positive result, 24 or 36 additional tests are required, which, together with the first eight tests, will mean a decrease in the number of tests from two to five times as compared to individual testing. The researchers believe that the number of tests can be decreased by optimizing the size of groups that takes into account the total number of swabs and the forecasted number of infected individuals. As the number of infected individuals increases, the possibility of saving swabs decreases but is still about 40% in the event of an incidence of 100 positive samples per 1,000, and 18% for an incidence of 200 per 1,000.
There are ways to optimize group testing, such as choosing the optimal group size based on the total number of swabs and the projected level of disease spreading. Another is the binary splitting method, in which a positive group is split into halves and is tested again, until individual positive swabs are detected. The second method, however, is very time-consuming, which decreases its attractiveness during a pandemic. In addition, to optimize group testing, transposition-based replication is used: after grouping the swabs, researchers form additional control groups from the same swabs and test them together with the main groups. This helps further cut the number of tests, and if the disease levels are low, it also helps to detect positive swabs in one step, which speeds up the testing considerably.
However, this method does not allow for experimenting with group sizes to detect the optimal group size under specific conditions. Researchers from HSE University and Vilnius University suggested OptReplica technology, which uses a more complicated algorithm of swab grouping in key and control groups and helps decrease the number of control groups. In addition, the algorithm helps calculate the optimal group size for the present number of swabs and the forecasted level of disease spreading. The researchers conducted experimental research on samples of 96 and 384 swabs, carrying out 100 randomized tests for each sample size, and compared the effectiveness of transposition-based replication and OptReplica method for different levels of disease incidence. The studies have shown that if the optimal size of groups is chosen, OptReplica is more effective than transposition-based replication. In cases with low incidence, the use of OptReplica, a 13x average reduction of tests can be achieved compared to individual testing without time delay.
“Our simulations are actually proving that using this optimization replication strategy is always advantageous and, even in case of high spread of the disease (10% or 20% of positives in the population), we are still competitive with individual testing strategy,” explained Mario Guarracino, Chief Research Fellow of the Laboratory of Algorithms and Technologies for Networks Analysis.
Related Links:
HSE Laboratory of Algorithms and Technologies for Networks Analysis
Vilnius University
Latest COVID-19 News
- New Immunosensor Paves Way to Rapid POC Testing for COVID-19 and Emerging Infectious Diseases
- Long COVID Etiologies Found in Acute Infection Blood Samples
- Novel Device Detects COVID-19 Antibodies in Five Minutes
- CRISPR-Powered COVID-19 Test Detects SARS-CoV-2 in 30 Minutes Using Gene Scissors
- Gut Microbiome Dysbiosis Linked to COVID-19
- Novel SARS CoV-2 Rapid Antigen Test Validated for Diagnostic Accuracy
- New COVID + Flu + R.S.V. Test to Help Prepare for `Tripledemic`
- AI Takes Guesswork Out Of Lateral Flow Testing
- Fastest Ever SARS-CoV-2 Antigen Test Designed for Non-Invasive COVID-19 Testing in Any Setting
- Rapid Antigen Tests Detect Omicron, Delta SARS-CoV-2 Variants
- Health Care Professionals Showed Increased Interest in POC Technologies During Pandemic, Finds Study
- Set Up Reserve Lab Capacity Now for Faster Response to Next Pandemic, Say Researchers
- Blood Test Performed During Initial Infection Predicts Long COVID Risk
- Low-Cost COVID-19 Testing Platform Combines Sensitivity of PCR and Speed of Antigen Tests
- Finger-Prick Blood Test Identifies Immunity to COVID-19
- Quick Test Kit Determines Immunity Against COVID-19 and Its Variants
Channels
Clinical Chemistry
view channel
New PSA-Based Prognostic Model Improves Prostate Cancer Risk Assessment
Prostate cancer is the second-leading cause of cancer death among American men, and about one in eight will be diagnosed in their lifetime. Screening relies on blood levels of prostate-specific antigen... Read more
Extracellular Vesicles Linked to Heart Failure Risk in CKD Patients
Chronic kidney disease (CKD) affects more than 1 in 7 Americans and is strongly associated with cardiovascular complications, which account for more than half of deaths among people with CKD.... Read moreMolecular Diagnostics
view channel
Diagnostic Device Predicts Treatment Response for Brain Tumors Via Blood Test
Glioblastoma is one of the deadliest forms of brain cancer, largely because doctors have no reliable way to determine whether treatments are working in real time. Assessing therapeutic response currently... Read more
Blood Test Detects Early-Stage Cancers by Measuring Epigenetic Instability
Early-stage cancers are notoriously difficult to detect because molecular changes are subtle and often missed by existing screening tools. Many liquid biopsies rely on measuring absolute DNA methylation... Read more
“Lab-On-A-Disc” Device Paves Way for More Automated Liquid Biopsies
Extracellular vesicles (EVs) are tiny particles released by cells into the bloodstream that carry molecular information about a cell’s condition, including whether it is cancerous. However, EVs are highly... Read more
Blood Test Identifies Inflammatory Breast Cancer Patients at Increased Risk of Brain Metastasis
Brain metastasis is a frequent and devastating complication in patients with inflammatory breast cancer, an aggressive subtype with limited treatment options. Despite its high incidence, the biological... Read moreHematology
view channel
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read more
Fast and Easy Test Could Revolutionize Blood Transfusions
Blood transfusions are a cornerstone of modern medicine, yet red blood cells can deteriorate quietly while sitting in cold storage for weeks. Although blood units have a fixed expiration date, cells from... Read more
Automated Hemostasis System Helps Labs of All Sizes Optimize Workflow
High-volume hemostasis sections must sustain rapid turnaround while managing reruns and reflex testing. Manual tube handling and preanalytical checks can strain staff time and increase opportunities for error.... Read more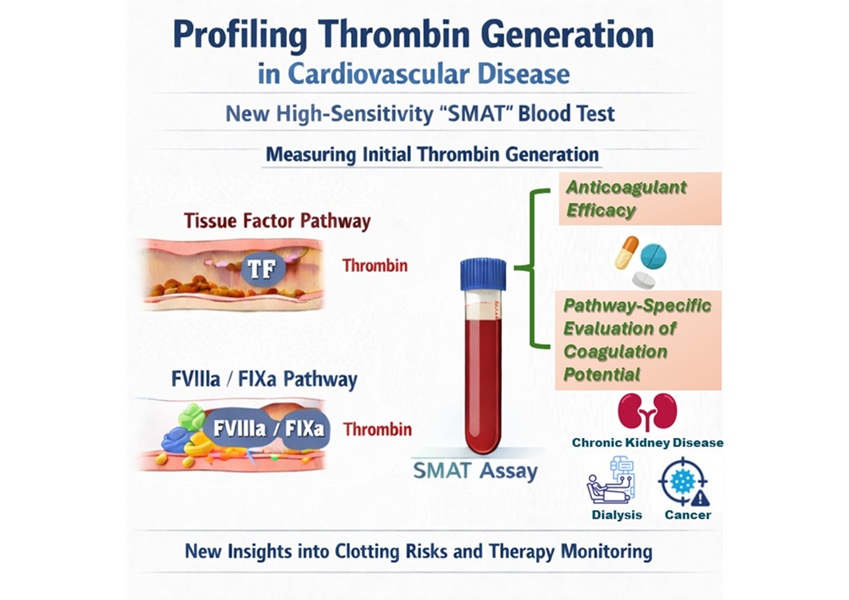
High-Sensitivity Blood Test Improves Assessment of Clotting Risk in Heart Disease Patients
Blood clotting is essential for preventing bleeding, but even small imbalances can lead to serious conditions such as thrombosis or dangerous hemorrhage. In cardiovascular disease, clinicians often struggle... Read moreImmunology
view channelBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read more
Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
Immunotherapy has transformed cancer treatment, but only a small proportion of patients experience lasting benefit, with response rates often remaining between 10% and 20%. Clinicians currently lack reliable... Read moreMicrobiology
view channel
Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
Alzheimer’s disease affects approximately 6.7 million people in the United States and nearly 50 million worldwide, yet early cognitive decline remains difficult to characterize. Increasing evidence suggests... Read moreAI-Powered Platform Enables Rapid Detection of Drug-Resistant C. Auris Pathogens
Infections caused by the pathogenic yeast Candida auris pose a significant threat to hospitalized patients, particularly those with weakened immune systems or those who have invasive medical devices.... Read morePathology
view channel
Engineered Yeast Cells Enable Rapid Testing of Cancer Immunotherapy
Developing new cancer immunotherapies is a slow, costly, and high-risk process, particularly for CAR T cell treatments that must precisely recognize cancer-specific antigens. Small differences in tumor... Read more
First-Of-Its-Kind Test Identifies Autism Risk at Birth
Autism spectrum disorder is treatable, and extensive research shows that early intervention can significantly improve cognitive, social, and behavioral outcomes. Yet in the United States, the average age... Read moreTechnology
view channel
Robotic Technology Unveiled for Automated Diagnostic Blood Draws
Routine diagnostic blood collection is a high‑volume task that can strain staffing and introduce human‑dependent variability, with downstream implications for sample quality and patient experience.... Read more
ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
Clinical laboratories generate billions of test results each year, creating a treasure trove of data with the potential to support more personalized testing, improve operational efficiency, and enhance patient care.... Read moreAptamer Biosensor Technology to Transform Virus Detection
Rapid and reliable virus detection is essential for controlling outbreaks, from seasonal influenza to global pandemics such as COVID-19. Conventional diagnostic methods, including cell culture, antigen... Read more
AI Models Could Predict Pre-Eclampsia and Anemia Earlier Using Routine Blood Tests
Pre-eclampsia and anemia are major contributors to maternal and child mortality worldwide, together accounting for more than half a million deaths each year and leaving millions with long-term health complications.... Read moreIndustry
view channelNew Collaboration Brings Automated Mass Spectrometry to Routine Laboratory Testing
Mass spectrometry is a powerful analytical technique that identifies and quantifies molecules based on their mass and electrical charge. Its high selectivity, sensitivity, and accuracy make it indispensable... Read more
AI-Powered Cervical Cancer Test Set for Major Rollout in Latin America
Noul Co., a Korean company specializing in AI-based blood and cancer diagnostics, announced it will supply its intelligence (AI)-based miLab CER cervical cancer diagnostic solution to Mexico under a multi‑year... Read more
Diasorin and Fisher Scientific Enter into US Distribution Agreement for Molecular POC Platform
Diasorin (Saluggia, Italy) has entered into an exclusive distribution agreement with Fisher Scientific, part of Thermo Fisher Scientific (Waltham, MA, USA), for the LIAISON NES molecular point-of-care... Read more