Rapid Sepsis Diagnostic Device to Enable Personalized Critical Care for ICU Patients
Posted on 24 Sep 2025
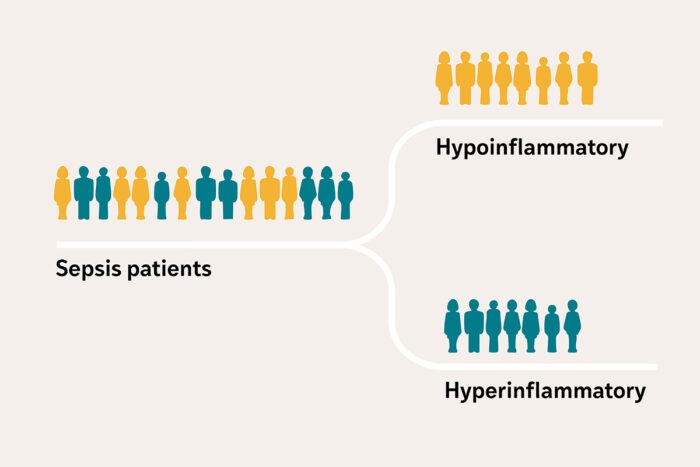
Sepsis is a life-threatening condition that occurs when the body’s response to infection spirals out of control, damaging organs and leading to critical illness. Patients often arrive at intensive care units (ICUs) with similar symptoms such as fever, low blood pressure, and kidney failure, yet their biological responses can differ significantly. Some experience a severe hyperinflammatory profile with higher mortality, while others have a less severe hypoinflammatory profile. Researchers have now developed a sepsis diagnostic device to quickly identify these subgroups and guide treatment decisions.
Researchers at Washington University School of Medicine (St. Louis, MO, USA) are developing a clinical test and handheld device for sepsis diagnostics. The device will classify patients into high-risk or low-risk groups based on two biomarkers, interleukin-8 (IL-8) and soluble tumor necrosis factor receptor 1 (sTNFR-1). The system uses a lateral flow assay, similar to a rapid COVID-19 test, enhanced with fluorescent nanoparticles for highly sensitive detection and quantification.
Previous research, including a study of 3,000 critically ill patients published in The Lancet Respiratory Medicine, showed IL-8 and sTNFR-1 as reliable indicators of inflammatory response. An analysis of past clinical trial data demonstrated that treatments previously deemed ineffective showed benefit in specific subgroups. This confirmed that distinguishing between hyperinflammatory and hypoinflammatory profiles could unlock new treatment strategies and repurpose earlier therapies.
The planned device will use a few drops of plasma applied to a test strip containing plasmonic fluors, which glow when binding to the biomarkers. A handheld camera detects the glow, and computer modeling quantifies biomarker levels to categorize patients in real time. Using a grant of USD 5 million awarded by the U.S. Department of Defense, physicians at WashU Medicine are developing this rapid, portable, and affordable tool for deployment in military zones, rural hospitals, and intensive care units, offering personalized care when every minute matters.
“This tool has the potential to reach patients at the bedside, offering personalized care based on each individual’s specific biological responses,” said Pratik Sinha, MBChB, PhD, assistant professor in the Department of Anesthesiology at Washington University School of Medicine. “We hope to fill a need in critical care that will help bring more effective treatments to more patients.”
Related Links:
WashU Medicine












