First Molecule Created to Suppress Major Component of Cancer Gene On-Off Switch
|
By LabMedica International staff writers Posted on 21 Oct 2010 |
In the endeavor to block the growth and spread of tumors, there have been many attempts to get cancer genes to ignore their internal regulatory instructions. In a new study, a team of scientists has created the first molecule able to prevent cancer genes from "hearing” those instructions, inhibiting the cancer process at its foundation.
The study, published online in late September 2010 by the journal Nature, demonstrated that proteins delivering stop and start instructions to a cancer gene--known as epigenetic "reader” proteins--can be targeted for future cancer therapies. The research is particularly pertinent to a rare but destructive cancer of children and young adults known as NUT midline carcinoma (NMC)--a disease so inflexible that no potential therapy for it has ever reached the stage of being evaluated in a clinical trial.
"In recent years, it has become clear that being able to control gene activity in cancer-- manipulating which genes are ‘on' or ‘off''--can be a high-impact approach to the disease,” said the study's senior author, James Bradner, M.D., of Dana-Farber Cancer Institute (Boston, MA, USA). "If you can switch off a cancer cell's growth genes, the cell will die. Alternatively, switching on a tissue gene can cause a cancer cell to become a more normal tissue cell.”
In this study, Dr. Bradner's lab synthesized a molecule that has both effects: by blocking a specific abnormal protein in NUT midline carcinoma cells, it stops them from dividing so prolifically and makes them ‘forget' they are cancer cells and start appearing more like normal cells. The assembled molecule affects the cell's multilayered machinery for controlling gene activity--the set of structures collectively known as the epigenome. Large portions of each gene play a regulatory role, dictating whether the gene is active, industriously sending orders for new proteins, or inactive, and temporarily at rest.
The gene's DNA is packaged in a substance called chromatin, which is the slate on which instructions to begin or cease activity are inscribed. The instructions themselves take the form of "bookmarks,” material placed on the chromatin by so-called epigenetic "writer” proteins. Another group of epigenetic proteins, known as "erasers,” is able to remove the bookmarks. Both types of proteins have effectively been disabled by researchers, using molecules generated in the laboratory or taken from nature. Their success has triggered intense interest in the development of anticancer therapies that work by blocking such proteins.
A third kind of epigenetic proteins--potentially the most appealing as therapeutic targets, because they switch genes on or off by "reading” the bookmarks--has received scant scientific attention. Dr. Bradner and his colleagues looked to this little-studied area of biology by focusing on NMC cells.
The disease is caused by a chromosomal translocation, in which two genes from different chromosomes become connected and give rise to an abnormal, fused protein known as BRD4-NUT. A review of the scientific literature suggested that some members of the benzodiazepine family of drugs, which includes Valium, Xanax, and Ativan, are active against "bromodomain” proteins such as BRD4. With that as a clue, Dr. Bradner and his Dana-Farber colleague Jun Qi, Ph.D., created an array of molecules to see if any inhibited a "reader” protein of the BRD4-NUT gene. One did, quite persuasively--a hybrid molecule, which researchers named JQ1, for Qi.
The investigators worked with researchers in the United States and overseas to learn more about the properties of JQ1 and how it works in cells. Stefan Knapp, Ph.D., of Oxford University (U.K.), provided crystal-clear images of the molecule bound to a protein; Olaf Wiest, Ph.D., of the University of Notre Dame (West Bend, IN, USA), showed that the molecule is less flexible in the presence of a protein, clarifying why it so effectively blocks the protein; and Andrew Kung, M.D., Ph.D., of Dana-Farber, modified animal models in which the molecule could be tested against NMC tumors.
The animal studies were especially promising. Investigators transplanted NMC cells from patients into laboratory mice, which were then given the JQ1 molecule. "The activity of the molecule was remarkable,” noted Dr. Bradner. "All the mice that received JQ1 lived; all that did not, died.”
For now, JQ1's primary utility is as a probe for better understanding the biology underlying NUT midline carcinoma. Drs. Bradner, Qi and their colleagues are customizing the molecule to maximize its effectiveness as a BRD4-NUT stopper. Ultimately, it, or a similar molecule, could be the basis for the first effective therapy against NMC.
"The disease tends to arise in the chest, head, or neck, along the vertical centerline of the body, with aggressive tumor growth and metastasis,” Dr. Bradner explained. "Patients may have a brief response to chemotherapy, but they eventually succumb to the spread of the disease.”
Unlike most cancers, NMC's tissue of origin is not known. It is a disease defined entirely by its genetic signature--the presence of the translocated gene BRD4-NUT. Prior to its genetic identification by Christopher French, M.D., of Brigham and Women's Hospital (Boston, MA, USA) and a study coauthor, NMC was not recognized as a definitive disease.
"This research further illustrates the promise of personalized medicine,” Dr. Bradner remarked, "which is the ability to deliver selected molecules to cancer-causing proteins to stop the cancer process while producing a minimum of residual side effects. The development of JQ1 or similar molecule into a drug may produce the first therapy specifically designed for patients with NMC.”
Related Links:
Dana-Farber Cancer Institute
Brigham and Women's Hospital
The study, published online in late September 2010 by the journal Nature, demonstrated that proteins delivering stop and start instructions to a cancer gene--known as epigenetic "reader” proteins--can be targeted for future cancer therapies. The research is particularly pertinent to a rare but destructive cancer of children and young adults known as NUT midline carcinoma (NMC)--a disease so inflexible that no potential therapy for it has ever reached the stage of being evaluated in a clinical trial.
"In recent years, it has become clear that being able to control gene activity in cancer-- manipulating which genes are ‘on' or ‘off''--can be a high-impact approach to the disease,” said the study's senior author, James Bradner, M.D., of Dana-Farber Cancer Institute (Boston, MA, USA). "If you can switch off a cancer cell's growth genes, the cell will die. Alternatively, switching on a tissue gene can cause a cancer cell to become a more normal tissue cell.”
In this study, Dr. Bradner's lab synthesized a molecule that has both effects: by blocking a specific abnormal protein in NUT midline carcinoma cells, it stops them from dividing so prolifically and makes them ‘forget' they are cancer cells and start appearing more like normal cells. The assembled molecule affects the cell's multilayered machinery for controlling gene activity--the set of structures collectively known as the epigenome. Large portions of each gene play a regulatory role, dictating whether the gene is active, industriously sending orders for new proteins, or inactive, and temporarily at rest.
The gene's DNA is packaged in a substance called chromatin, which is the slate on which instructions to begin or cease activity are inscribed. The instructions themselves take the form of "bookmarks,” material placed on the chromatin by so-called epigenetic "writer” proteins. Another group of epigenetic proteins, known as "erasers,” is able to remove the bookmarks. Both types of proteins have effectively been disabled by researchers, using molecules generated in the laboratory or taken from nature. Their success has triggered intense interest in the development of anticancer therapies that work by blocking such proteins.
A third kind of epigenetic proteins--potentially the most appealing as therapeutic targets, because they switch genes on or off by "reading” the bookmarks--has received scant scientific attention. Dr. Bradner and his colleagues looked to this little-studied area of biology by focusing on NMC cells.
The disease is caused by a chromosomal translocation, in which two genes from different chromosomes become connected and give rise to an abnormal, fused protein known as BRD4-NUT. A review of the scientific literature suggested that some members of the benzodiazepine family of drugs, which includes Valium, Xanax, and Ativan, are active against "bromodomain” proteins such as BRD4. With that as a clue, Dr. Bradner and his Dana-Farber colleague Jun Qi, Ph.D., created an array of molecules to see if any inhibited a "reader” protein of the BRD4-NUT gene. One did, quite persuasively--a hybrid molecule, which researchers named JQ1, for Qi.
The investigators worked with researchers in the United States and overseas to learn more about the properties of JQ1 and how it works in cells. Stefan Knapp, Ph.D., of Oxford University (U.K.), provided crystal-clear images of the molecule bound to a protein; Olaf Wiest, Ph.D., of the University of Notre Dame (West Bend, IN, USA), showed that the molecule is less flexible in the presence of a protein, clarifying why it so effectively blocks the protein; and Andrew Kung, M.D., Ph.D., of Dana-Farber, modified animal models in which the molecule could be tested against NMC tumors.
The animal studies were especially promising. Investigators transplanted NMC cells from patients into laboratory mice, which were then given the JQ1 molecule. "The activity of the molecule was remarkable,” noted Dr. Bradner. "All the mice that received JQ1 lived; all that did not, died.”
For now, JQ1's primary utility is as a probe for better understanding the biology underlying NUT midline carcinoma. Drs. Bradner, Qi and their colleagues are customizing the molecule to maximize its effectiveness as a BRD4-NUT stopper. Ultimately, it, or a similar molecule, could be the basis for the first effective therapy against NMC.
"The disease tends to arise in the chest, head, or neck, along the vertical centerline of the body, with aggressive tumor growth and metastasis,” Dr. Bradner explained. "Patients may have a brief response to chemotherapy, but they eventually succumb to the spread of the disease.”
Unlike most cancers, NMC's tissue of origin is not known. It is a disease defined entirely by its genetic signature--the presence of the translocated gene BRD4-NUT. Prior to its genetic identification by Christopher French, M.D., of Brigham and Women's Hospital (Boston, MA, USA) and a study coauthor, NMC was not recognized as a definitive disease.
"This research further illustrates the promise of personalized medicine,” Dr. Bradner remarked, "which is the ability to deliver selected molecules to cancer-causing proteins to stop the cancer process while producing a minimum of residual side effects. The development of JQ1 or similar molecule into a drug may produce the first therapy specifically designed for patients with NMC.”
Related Links:
Dana-Farber Cancer Institute
Brigham and Women's Hospital
Latest BioResearch News
- Barcoded DNA Sheds Light on Hidden Complexities in Breast Cancer Detection
- CRISPR-Based Platform Pinpoints Drivers of Acute Myeloid Leukemia in Patient Cells
- Protective Brain Protein Emerges as Biomarker Target in Alzheimer’s Disease
- Genome Analysis Predicts Likelihood of Neurodisability in Oxygen-Deprived Newborns
- Gene Panel Predicts Disease Progession for Patients with B-cell Lymphoma
- New Method Simplifies Preparation of Tumor Genomic DNA Libraries
- New Tool Developed for Diagnosis of Chronic HBV Infection
- Panel of Genetic Loci Accurately Predicts Risk of Developing Gout
- Disrupted TGFB Signaling Linked to Increased Cancer-Related Bacteria
- Gene Fusion Protein Proposed as Prostate Cancer Biomarker
- NIV Test to Diagnose and Monitor Vascular Complications in Diabetes
- Semen Exosome MicroRNA Proves Biomarker for Prostate Cancer
- Genetic Loci Link Plasma Lipid Levels to CVD Risk
- Newly Identified Gene Network Aids in Early Diagnosis of Autism Spectrum Disorder
- Link Confirmed between Living in Poverty and Developing Diseases
- Genomic Study Identifies Kidney Disease Loci in Type I Diabetes Patients
Channels
Clinical Chemistry
view channelNew Blood Test Index Offers Earlier Detection of Liver Scarring
Metabolic fatty liver disease is highly prevalent and often silent, yet it can progress to fibrosis, cirrhosis, and liver failure. Current first-line blood test scores frequently return indeterminate results,... Read more
Electronic Nose Smells Early Signs of Ovarian Cancer in Blood
Ovarian cancer is often diagnosed at a late stage because its symptoms are vague and resemble those of more common conditions. Unlike breast cancer, there is currently no reliable screening method, and... Read moreMolecular Diagnostics
view channel
New Blood Test Can Help Predict Testicular Cancer Recurrence
Stage 1 testicular germ cell tumor is typically treated with surgery followed by active surveillance. Although most patients experience strong long-term outcomes, about one in four will see their cancer... Read more
New Test Detects Alzheimer’s by Analyzing Altered Protein Shapes in Blood
Alzheimer’s disease begins developing years before memory loss or other symptoms become visible. Misfolded proteins gradually accumulate in the brain, disrupting normal cellular processes.... Read more
New Diagnostic Markers for Multiple Sclerosis Discovered in Cerebrospinal Fluid
Multiple sclerosis (MS) affects nearly three million people worldwide and can cause symptoms such as numbness, visual disturbances, fatigue, and neurological disability. Diagnosing the disease can be challenging... Read moreHematology
view channel
Rapid Cartridge-Based Test Aims to Expand Access to Hemoglobin Disorder Diagnosis
Sickle cell disease and beta thalassemia are hemoglobin disorders that often require referral to specialized laboratories for definitive diagnosis, delaying results for patients and clinicians.... Read more
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read moreImmunology
view channel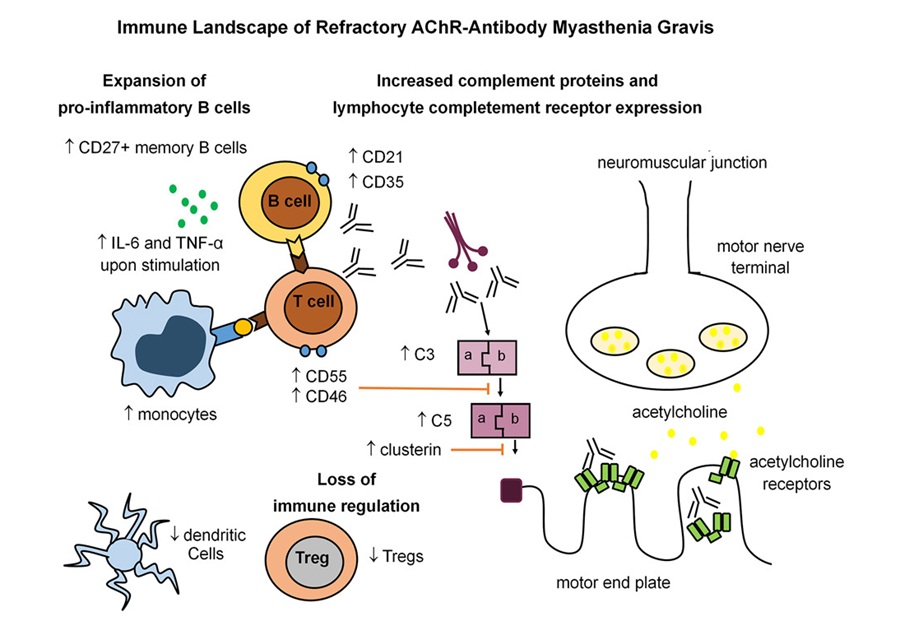
Immune Signature Identified in Treatment-Resistant Myasthenia Gravis
Myasthenia gravis is a rare autoimmune disorder in which immune attack at the neuromuscular junction causes fluctuating weakness that can impair vision, movement, speech, swallowing, and breathing.... Read more
New Biomarker Predicts Chemotherapy Response in Triple-Negative Breast Cancer
Triple-negative breast cancer is an aggressive form of breast cancer in which patients often show widely varying responses to chemotherapy. Predicting who will benefit from treatment remains challenging,... Read moreBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read moreMicrobiology
view channel
Rapid Sequencing Could Transform Tuberculosis Care
Tuberculosis remains the world’s leading cause of death from a single infectious agent, responsible for more than one million deaths each year. Diagnosing and monitoring the disease can be slow because... Read more
Blood-Based Viral Signature Identified in Crohn’s Disease
Crohn’s disease is a chronic inflammatory intestinal disorder affecting approximately 0.4% of the European population, with symptoms and progression that vary widely. Although viral components of the microbiome... Read morePathology
view channel
Pathogen-Agnostic Testing Reveals Hidden Respiratory Threats in Negative Samples
Polymerase Chain Reaction (PCR) testing became widely recognized during the COVID-19 pandemic as a powerful method for detecting viruses such as SARS-CoV-2. PCR belongs to a group of diagnostic methods... Read more
Molecular Imaging to Reduce Need for Melanoma Biopsies
Melanoma is the deadliest form of skin cancer and accounts for the vast majority of skin cancer-related deaths. Because early melanomas can closely resemble benign moles, clinicians often rely on visual... Read moreTechnology
view channel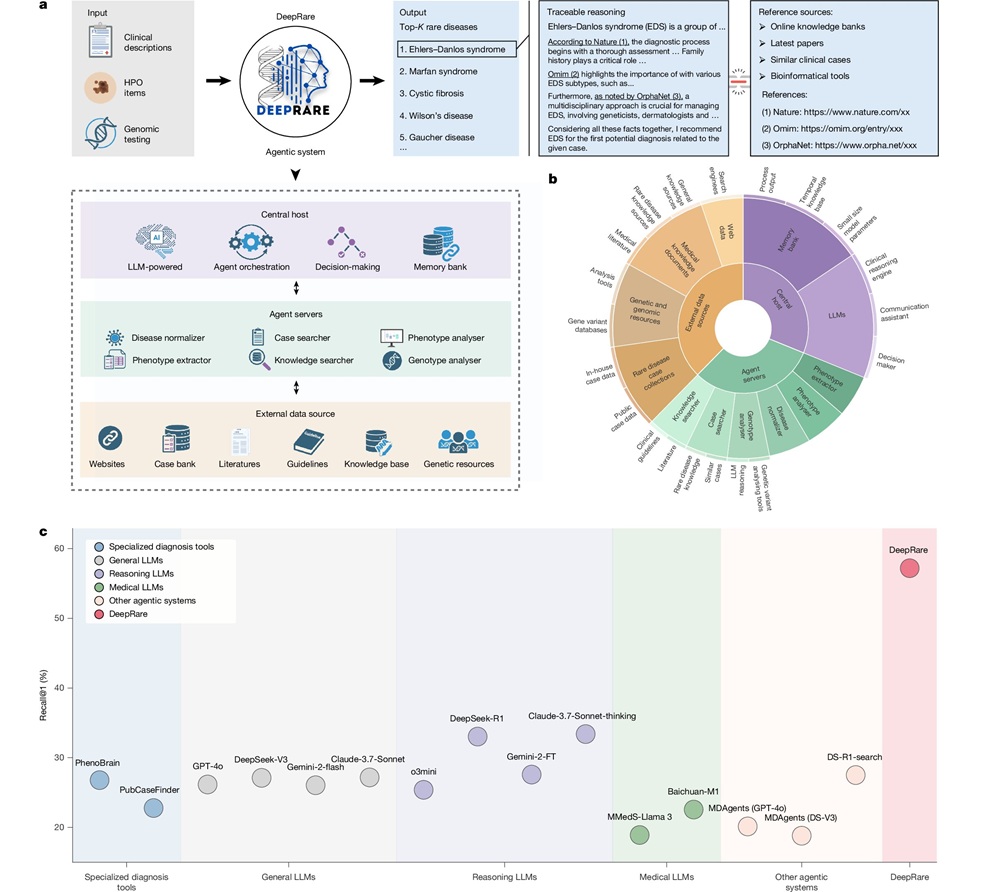
AI Model Outperforms Clinicians in Rare Disease Detection
Rare diseases affect an estimated 300 million people worldwide, yet diagnosis is often protracted and error-prone. Many conditions present with heterogeneous signs that overlap with common disorders, leading... Read more
AI-Driven Diagnostic Demonstrates High Accuracy in Detecting Periprosthetic Joint Infection
Periprosthetic joint infection (PJI) is a rare but serious complication affecting 1% to 2% of primary joint replacement surgeries. The condition occurs when bacteria or fungi infect tissues around an implanted... Read moreIndustry
view channel
Cepheid Joins CDC Initiative to Strengthen U.S. Pandemic Testing Preparednesss
Cepheid (Sunnyvale, CA, USA) has been selected by the U.S. Centers for Disease Control and Prevention (CDC) as one of four national collaborators in a federal initiative to speed rapid diagnostic technologies... Read more
QuidelOrtho Collaborates with Lifotronic to Expand Global Immunoassay Portfolio
QuidelOrtho (San Diego, CA, USA) has entered a long-term strategic supply agreement with Lifotronic Technology (Shenzhen, China) to expand its global immunoassay portfolio and accelerate customer access... Read more





















