Chronic Anemia Cured by Gene Therapy Using Genetically Engineered Blood Vessels
|
By LabMedica International staff writers Posted on 29 Nov 2011 |
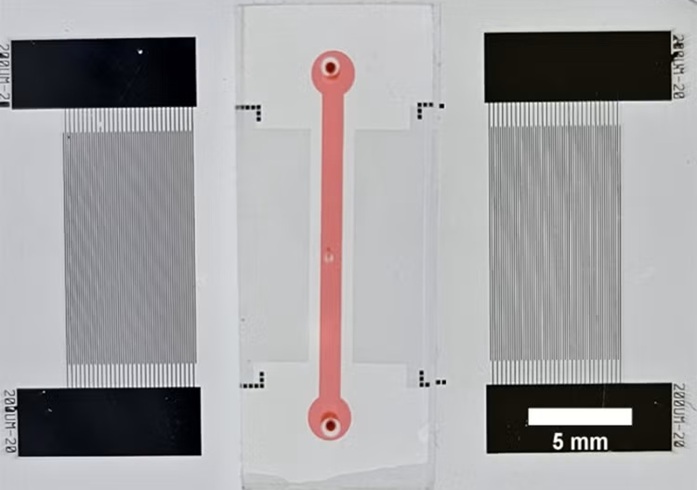
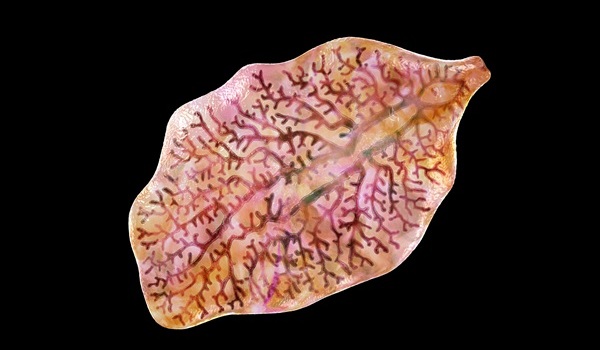
A novel gene therapeutic method employing genetically engineered blood vessels to deliver erythropoietin (EPO) to anemic mice was described in a proof-of-concept study.
Investigators at Harvard Medical School (Boston, MA, USA) created a new type of blood vessel by isolating endothelial colony-forming cells from human blood and then inserting into these cells the gene that encodes EPO. The gene that was inserted was part of a complex that included an “off/on switch” activated by the drug doxycycline.
The genetically engineered colony-forming cells were injected under the skin of immunodeficient mice that had been rendered anemic by radiation treatment (as often occurs in cancer patients) or through loss of kidney tissue (modeling chronic kidney failure).
Results published in the November 17, 2011, issue of the journal Blood revealed that the transplanted cells spontaneously formed networks of blood vessels that became integrated into the animals' own circulatory system. EPO produced by the genetically engineered cells was then released directly into the bloodstream. EPO production could be controlled by administrating or withholding doxycycline.
“Blood-vessel implants are an ideal platform technology for gene therapy applications whose goal is systemic drug delivery,” said senior author Dr. Juan M. Melero-Martin, assistant professor of surgery at Harvard Medical School. “Blood vessels are one of the few tissues where we have good control over engraftment. Endothelial cells are easily isolated from blood, are good at assembling themselves into blood vessels, and are ideal for releasing compounds into the bloodstream, since they line the blood vessels.”
“Such drugs are currently made in bioreactors by engineered cells, and are very expensive to make in large amounts. The paradigm shift here is, why we do not instruct your own cells to be the factory?” said Dr. Melero-Martin.
If this approach can be applied in humans, it would relieve patients from having to receive frequent EPO injections, thus reducing the medical costs associated with the management of anemia.
Related Links:
Harvard Medical School
Investigators at Harvard Medical School (Boston, MA, USA) created a new type of blood vessel by isolating endothelial colony-forming cells from human blood and then inserting into these cells the gene that encodes EPO. The gene that was inserted was part of a complex that included an “off/on switch” activated by the drug doxycycline.
The genetically engineered colony-forming cells were injected under the skin of immunodeficient mice that had been rendered anemic by radiation treatment (as often occurs in cancer patients) or through loss of kidney tissue (modeling chronic kidney failure).
Results published in the November 17, 2011, issue of the journal Blood revealed that the transplanted cells spontaneously formed networks of blood vessels that became integrated into the animals' own circulatory system. EPO produced by the genetically engineered cells was then released directly into the bloodstream. EPO production could be controlled by administrating or withholding doxycycline.
“Blood-vessel implants are an ideal platform technology for gene therapy applications whose goal is systemic drug delivery,” said senior author Dr. Juan M. Melero-Martin, assistant professor of surgery at Harvard Medical School. “Blood vessels are one of the few tissues where we have good control over engraftment. Endothelial cells are easily isolated from blood, are good at assembling themselves into blood vessels, and are ideal for releasing compounds into the bloodstream, since they line the blood vessels.”
“Such drugs are currently made in bioreactors by engineered cells, and are very expensive to make in large amounts. The paradigm shift here is, why we do not instruct your own cells to be the factory?” said Dr. Melero-Martin.
If this approach can be applied in humans, it would relieve patients from having to receive frequent EPO injections, thus reducing the medical costs associated with the management of anemia.
Related Links:
Harvard Medical School
Latest BioResearch News
- Barcoded DNA Sheds Light on Hidden Complexities in Breast Cancer Detection
- CRISPR-Based Platform Pinpoints Drivers of Acute Myeloid Leukemia in Patient Cells
- Protective Brain Protein Emerges as Biomarker Target in Alzheimer’s Disease
- Genome Analysis Predicts Likelihood of Neurodisability in Oxygen-Deprived Newborns
- Gene Panel Predicts Disease Progession for Patients with B-cell Lymphoma
- New Method Simplifies Preparation of Tumor Genomic DNA Libraries
- New Tool Developed for Diagnosis of Chronic HBV Infection
- Panel of Genetic Loci Accurately Predicts Risk of Developing Gout
- Disrupted TGFB Signaling Linked to Increased Cancer-Related Bacteria
- Gene Fusion Protein Proposed as Prostate Cancer Biomarker
- NIV Test to Diagnose and Monitor Vascular Complications in Diabetes
- Semen Exosome MicroRNA Proves Biomarker for Prostate Cancer
- Genetic Loci Link Plasma Lipid Levels to CVD Risk
- Newly Identified Gene Network Aids in Early Diagnosis of Autism Spectrum Disorder
- Link Confirmed between Living in Poverty and Developing Diseases
- Genomic Study Identifies Kidney Disease Loci in Type I Diabetes Patients
Channels
Clinical Chemistry
view channelNew Blood Test Index Offers Earlier Detection of Liver Scarring
Metabolic fatty liver disease is highly prevalent and often silent, yet it can progress to fibrosis, cirrhosis, and liver failure. Current first-line blood test scores frequently return indeterminate results,... Read more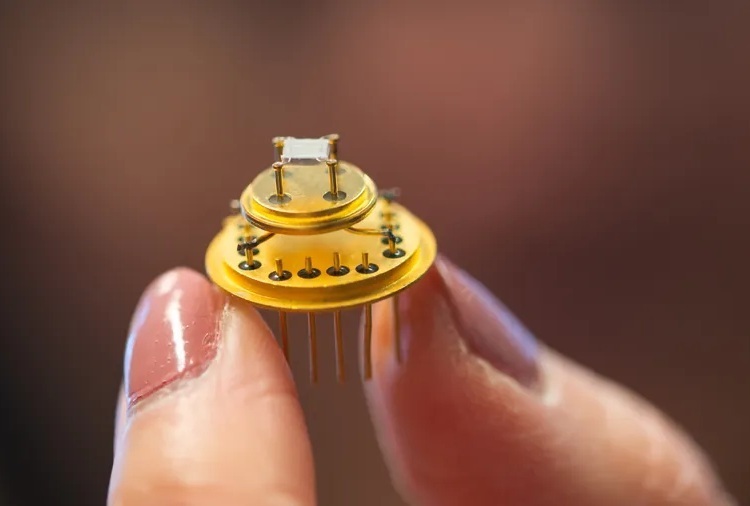
Electronic Nose Smells Early Signs of Ovarian Cancer in Blood
Ovarian cancer is often diagnosed at a late stage because its symptoms are vague and resemble those of more common conditions. Unlike breast cancer, there is currently no reliable screening method, and... Read moreMolecular Diagnostics
view channel
Simple One-Hour Saliva Test Detects Common Cancers
Early detection is critical for improving cancer outcomes, yet many diagnostic tests rely on invasive procedures such as blood draws or biopsies. Researchers are exploring simpler approaches that could... Read more
Blood Test Could Help Guide Treatment Decisions in Germ Cell Tumors
Chemotherapy is often highly effective for germ cell tumors, but in a subset of patients, the disease does not respond well to standard treatment. For these individuals, doctors may consider high-dose... Read moreHematology
view channel
Rapid Cartridge-Based Test Aims to Expand Access to Hemoglobin Disorder Diagnosis
Sickle cell disease and beta thalassemia are hemoglobin disorders that often require referral to specialized laboratories for definitive diagnosis, delaying results for patients and clinicians.... Read more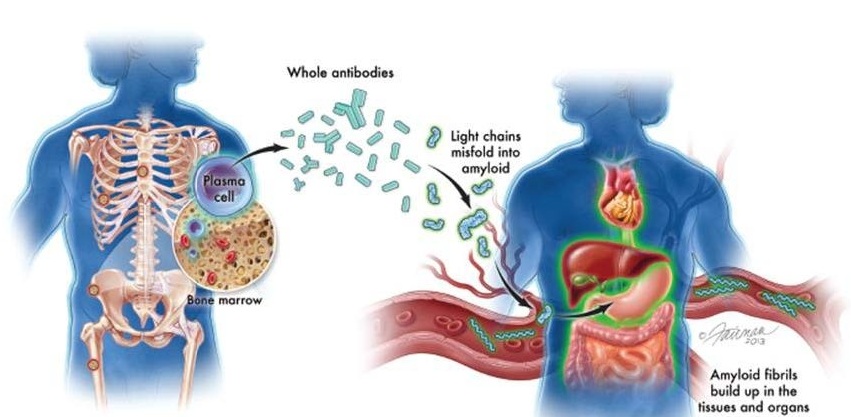
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read moreImmunology
view channel
Cancer Mutation ‘Fingerprints’ to Improve Prediction of Immunotherapy Response
Cancer cells accumulate thousands of genetic mutations, but not all mutations affect tumors in the same way. Some make cancer cells more visible to the immune system, while others allow tumors to evade... Read more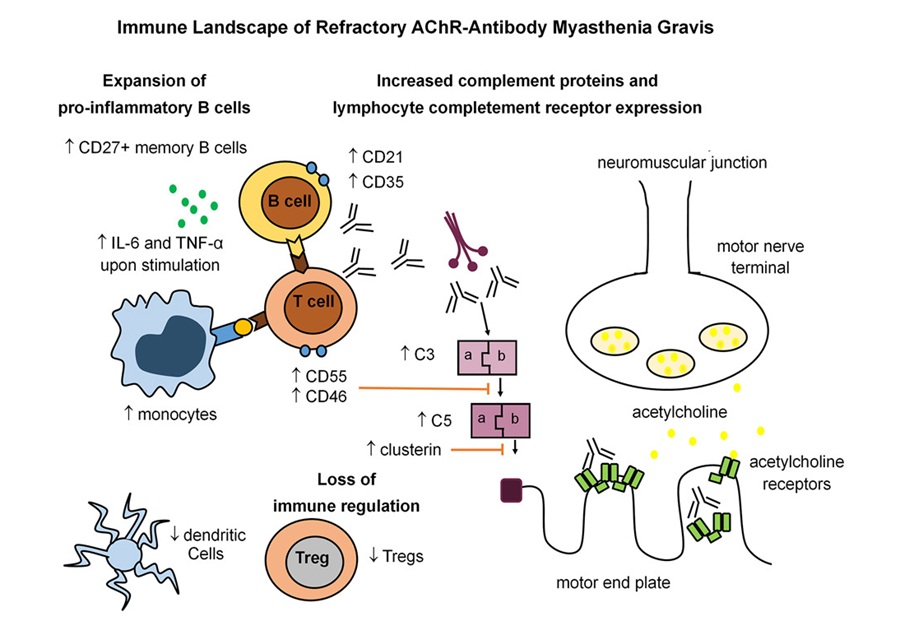
Immune Signature Identified in Treatment-Resistant Myasthenia Gravis
Myasthenia gravis is a rare autoimmune disorder in which immune attack at the neuromuscular junction causes fluctuating weakness that can impair vision, movement, speech, swallowing, and breathing.... Read more
New Biomarker Predicts Chemotherapy Response in Triple-Negative Breast Cancer
Triple-negative breast cancer is an aggressive form of breast cancer in which patients often show widely varying responses to chemotherapy. Predicting who will benefit from treatment remains challenging,... Read moreBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read moreMicrobiology
view channel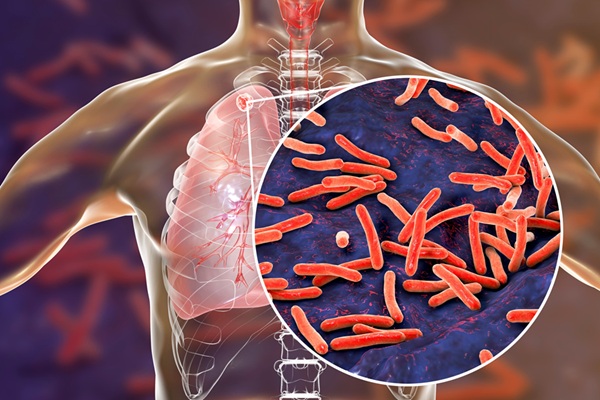
Rapid Sequencing Could Transform Tuberculosis Care
Tuberculosis remains the world’s leading cause of death from a single infectious agent, responsible for more than one million deaths each year. Diagnosing and monitoring the disease can be slow because... Read more
Blood-Based Viral Signature Identified in Crohn’s Disease
Crohn’s disease is a chronic inflammatory intestinal disorder affecting approximately 0.4% of the European population, with symptoms and progression that vary widely. Although viral components of the microbiome... Read morePathology
view channel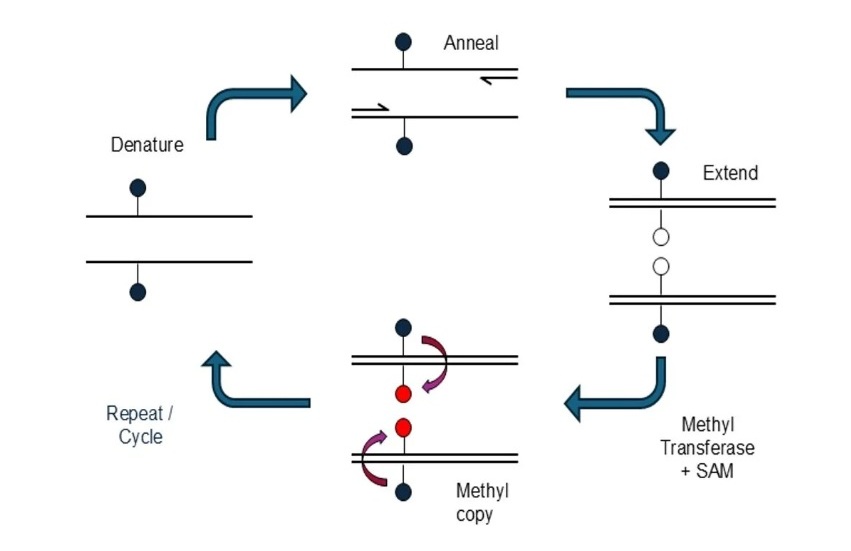
Novel mcPCR Technology to Transform Testing of Clinical Samples
DNA methylation is an important biological marker used in the diagnosis and monitoring of many diseases, including cancer. These chemical modifications to DNA influence gene activity and can reveal early... Read more
Sex Differences in Alzheimer’s Biomarkers Linked to Faster Cognitive Decline
Sex differences in Alzheimer’s disease present ongoing diagnostic challenges, with women often experiencing a disproportionate disease burden even when preclinical amyloid-beta levels are similar to men.... Read moreTechnology
view channel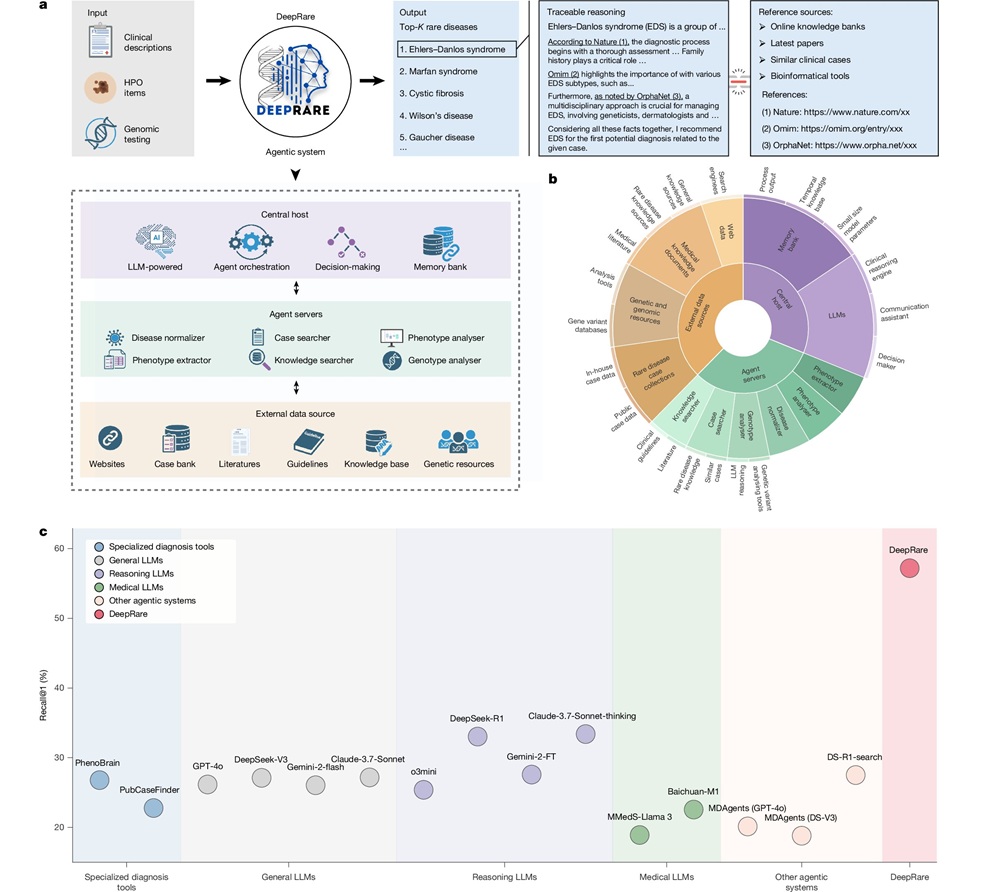
AI Model Outperforms Clinicians in Rare Disease Detection
Rare diseases affect an estimated 300 million people worldwide, yet diagnosis is often protracted and error-prone. Many conditions present with heterogeneous signs that overlap with common disorders, leading... Read more
AI-Driven Diagnostic Demonstrates High Accuracy in Detecting Periprosthetic Joint Infection
Periprosthetic joint infection (PJI) is a rare but serious complication affecting 1% to 2% of primary joint replacement surgeries. The condition occurs when bacteria or fungi infect tissues around an implanted... Read moreIndustry
view channel
Cepheid Joins CDC Initiative to Strengthen U.S. Pandemic Testing Preparednesss
Cepheid (Sunnyvale, CA, USA) has been selected by the U.S. Centers for Disease Control and Prevention (CDC) as one of four national collaborators in a federal initiative to speed rapid diagnostic technologies... Read more
QuidelOrtho Collaborates with Lifotronic to Expand Global Immunoassay Portfolio
QuidelOrtho (San Diego, CA, USA) has entered a long-term strategic supply agreement with Lifotronic Technology (Shenzhen, China) to expand its global immunoassay portfolio and accelerate customer access... Read more








 Analyzer.jpg)