Combined Gene and Immunotherapy Shows Potential for Aggressive Brain Tumors
|
By LabMedica International staff writers Posted on 17 Jan 2017 |
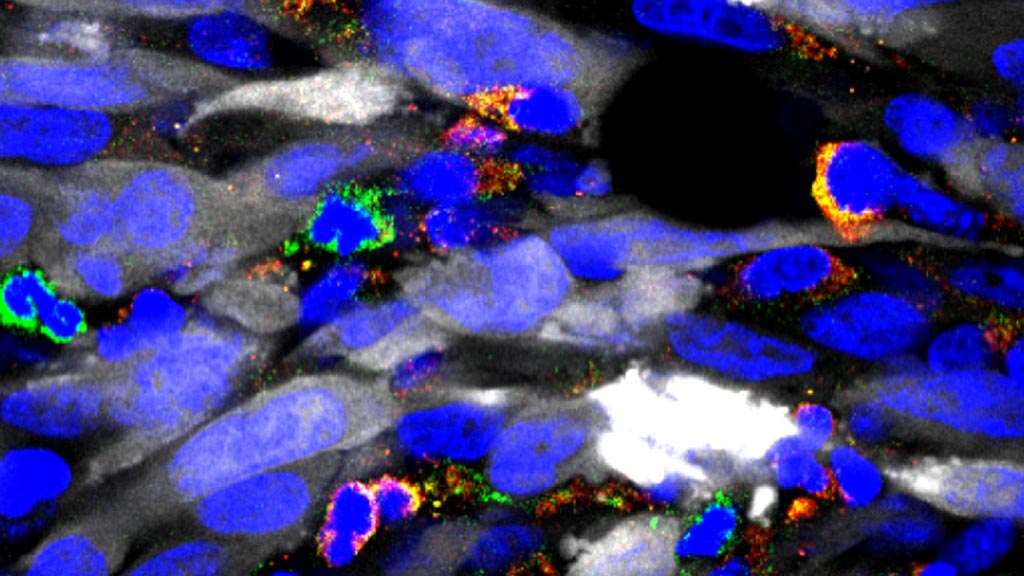
Image: A photomicrograph showing numerous immune suppressive cells in green and yellow, infiltrating the tumor mass (tumor cells in white). By depleting these immune suppressive cells, immunotherapy becomes much more effective (Photo courtesy of the University of Michigan).
A novel approach that combined gene and immunotherapy demonstrated considerable potential in a mouse model as a method for treating the aggressive brain tumor glioblastoma multiforme (GBM).
GBM is the most common primary tumor of the central nervous system and is almost always fatal. The aggressive invasion of GBM cells into the surrounding normal brain makes complete surgical removal impossible, significantly increases resistance to the standard therapy regimen, and virtually assures tumor recurrence. Median survival for newly diagnosed GBM is 14.6 months and declines to eight months for patients with recurrent GBM.
While immunotherapeutic approaches that harness the cytotoxic and memory potential of the host immune system have shown great benefit in other types of cancer. GBMs have developed multiple strategies, including the accumulation of myeloid-derived suppressor cells (MDSCs) to induce immunosuppression. MDSCs contribute to an immunosuppressive network that protects tumors by disabling T-cell adaptive immunity.
As it is imperative to develop multipronged approaches when aiming to generate a robust anti-tumor immune response, end investigators at the University of Michigan tested whether combining MDSC depletion or checkpoint blockade would increase the efficacy of immune-stimulatory herpes simplex type-I thymidine kinase (TK) plus Fms-like tyrosine kinase ligand (Flt3L)-mediated immune stimulatory gene therapy. The method used by the investigators on a mouse GBM model required injecting adenovirus vectors carrying herpes simplex 1 thymidine kinase into the tumor, followed by an antiviral, to elicit tumor cell death. This treatment was used in combination with another adenovirus vector carrying an immune stimulatory cytokine to recruit immune cells into the tumor.
Results published in the January 4, 2017, online edition of the journal Molecular Therapy revealed that MDSCs constituted more than 40% of the tumor-infiltrating immune cells. These cells expressed IL-4Ralpha, inducible nitric oxide synthase (iNOS), arginase, programmed death ligand 1 (PDL1), and CD80, molecules that are critically involved in antigen-specific T-cell suppression.
Depletion of MDSCs strongly enhanced the TK/Flt3L gene therapy-induced tumor-specific CD8 T-cell response, which led to an increased median survival and percentage of long-term survivors. Also, combining PDL1 or CTLA-4 immune checkpoint blockade greatly improved the efficacy of TK/Flt3L gene therapy.
"For the first time, we proved that a type of immunosuppressive cells within the tumor environment play a major role in determining the impact of immunotherapies," said senior author Dr. Maria Castro, professor of neurosurgery and cell and developmental biology at the University of Michigan. "We hope the implementation of our gene therapy strategy for gliomas, used in combination with immune checkpoint blockade, will eventually provide successful treatment for patients with this devastating brain cancer."
GBM is the most common primary tumor of the central nervous system and is almost always fatal. The aggressive invasion of GBM cells into the surrounding normal brain makes complete surgical removal impossible, significantly increases resistance to the standard therapy regimen, and virtually assures tumor recurrence. Median survival for newly diagnosed GBM is 14.6 months and declines to eight months for patients with recurrent GBM.
While immunotherapeutic approaches that harness the cytotoxic and memory potential of the host immune system have shown great benefit in other types of cancer. GBMs have developed multiple strategies, including the accumulation of myeloid-derived suppressor cells (MDSCs) to induce immunosuppression. MDSCs contribute to an immunosuppressive network that protects tumors by disabling T-cell adaptive immunity.
As it is imperative to develop multipronged approaches when aiming to generate a robust anti-tumor immune response, end investigators at the University of Michigan tested whether combining MDSC depletion or checkpoint blockade would increase the efficacy of immune-stimulatory herpes simplex type-I thymidine kinase (TK) plus Fms-like tyrosine kinase ligand (Flt3L)-mediated immune stimulatory gene therapy. The method used by the investigators on a mouse GBM model required injecting adenovirus vectors carrying herpes simplex 1 thymidine kinase into the tumor, followed by an antiviral, to elicit tumor cell death. This treatment was used in combination with another adenovirus vector carrying an immune stimulatory cytokine to recruit immune cells into the tumor.
Results published in the January 4, 2017, online edition of the journal Molecular Therapy revealed that MDSCs constituted more than 40% of the tumor-infiltrating immune cells. These cells expressed IL-4Ralpha, inducible nitric oxide synthase (iNOS), arginase, programmed death ligand 1 (PDL1), and CD80, molecules that are critically involved in antigen-specific T-cell suppression.
Depletion of MDSCs strongly enhanced the TK/Flt3L gene therapy-induced tumor-specific CD8 T-cell response, which led to an increased median survival and percentage of long-term survivors. Also, combining PDL1 or CTLA-4 immune checkpoint blockade greatly improved the efficacy of TK/Flt3L gene therapy.
"For the first time, we proved that a type of immunosuppressive cells within the tumor environment play a major role in determining the impact of immunotherapies," said senior author Dr. Maria Castro, professor of neurosurgery and cell and developmental biology at the University of Michigan. "We hope the implementation of our gene therapy strategy for gliomas, used in combination with immune checkpoint blockade, will eventually provide successful treatment for patients with this devastating brain cancer."
Latest BioResearch News
- Mass Spectrometry Technique Detects Protein and Sugar Changes in Neurodegeneration
- Barcoded DNA Sheds Light on Hidden Complexities in Breast Cancer Detection
- CRISPR-Based Platform Pinpoints Drivers of Acute Myeloid Leukemia in Patient Cells
- Protective Brain Protein Emerges as Biomarker Target in Alzheimer’s Disease
- Genome Analysis Predicts Likelihood of Neurodisability in Oxygen-Deprived Newborns
- Gene Panel Predicts Disease Progession for Patients with B-cell Lymphoma
- New Method Simplifies Preparation of Tumor Genomic DNA Libraries
- New Tool Developed for Diagnosis of Chronic HBV Infection
- Panel of Genetic Loci Accurately Predicts Risk of Developing Gout
- Disrupted TGFB Signaling Linked to Increased Cancer-Related Bacteria
- Gene Fusion Protein Proposed as Prostate Cancer Biomarker
- NIV Test to Diagnose and Monitor Vascular Complications in Diabetes
- Semen Exosome MicroRNA Proves Biomarker for Prostate Cancer
- Genetic Loci Link Plasma Lipid Levels to CVD Risk
- Newly Identified Gene Network Aids in Early Diagnosis of Autism Spectrum Disorder
- Link Confirmed between Living in Poverty and Developing Diseases
Channels
Clinical Chemistry
view channel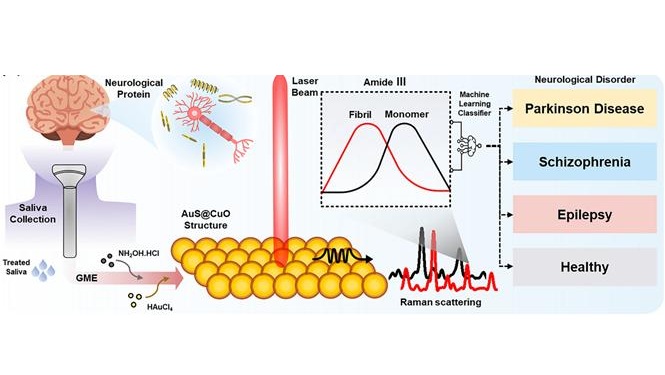
AI Sensor Detects Neurological Disorders Using Single Saliva Drop
Neurological disorders such as Parkinson’s disease and Alzheimer’s disease often develop gradually and present subtle symptoms in their early stages. Because early signs are frequently vague or atypical,... Read moreNew Blood Test Index Offers Earlier Detection of Liver Scarring
Metabolic fatty liver disease is highly prevalent and often silent, yet it can progress to fibrosis, cirrhosis, and liver failure. Current first-line blood test scores frequently return indeterminate results,... Read moreMolecular Diagnostics
view channel
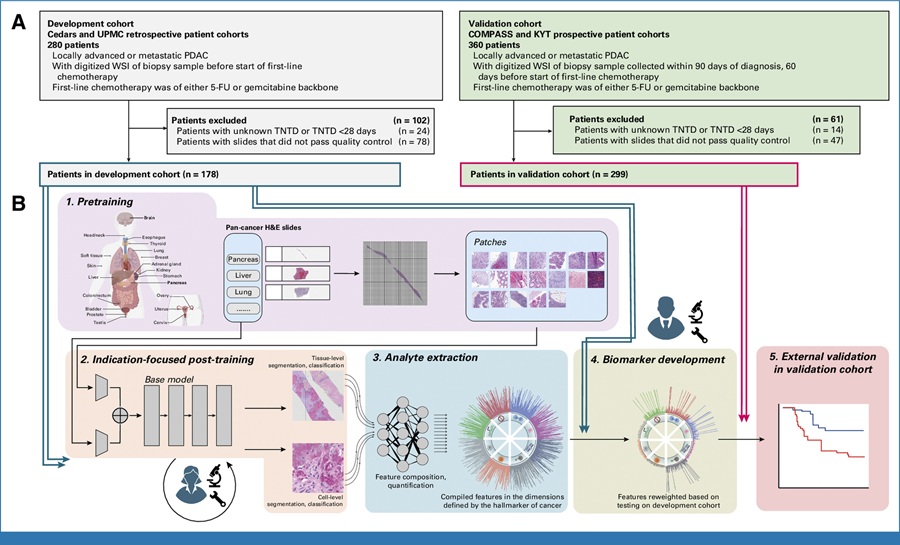
AI-Powered Blood Test Detects Early Pancreatic Cancer with More Than 90% Accuracy
Pancreatic cancer is one of the most lethal cancers, often referred to as the “King of Cancers” because symptoms usually appear only at advanced stages. As a result, most patients are diagnosed late, and... Read more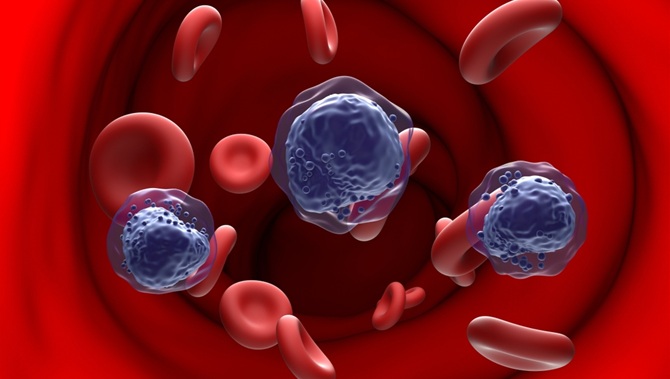
AI-Powered Blood Test Flags Relapse Risk Earlier After Transplant
Relapse after allogeneic hematopoietic cell transplant is a major cause of mortality in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), and standard monitoring can miss early warning signals.... Read more
World’s First Portable POC Test Simultaneously Detects Four Common STIs in One Hour
Sexually transmitted infections (STIs) often present with similar symptoms, making accurate diagnosis challenging without laboratory testing. Delays in identifying the exact infection can lead to inappropriate... Read moreHematology
view channel
Rapid Cartridge-Based Test Aims to Expand Access to Hemoglobin Disorder Diagnosis
Sickle cell disease and beta thalassemia are hemoglobin disorders that often require referral to specialized laboratories for definitive diagnosis, delaying results for patients and clinicians.... Read more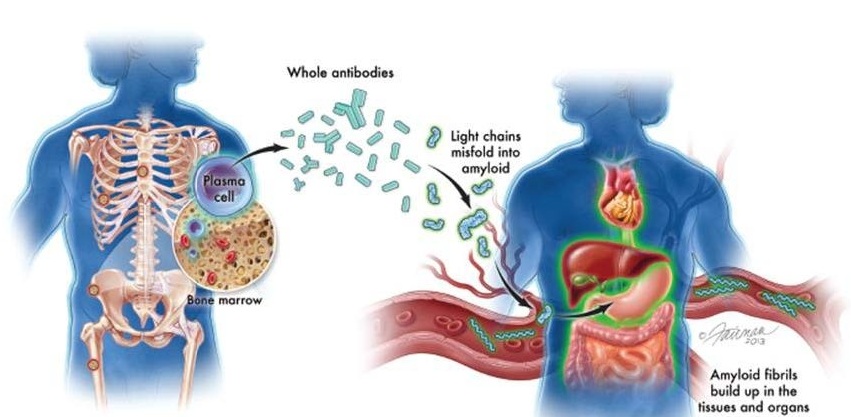
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read moreImmunology
view channel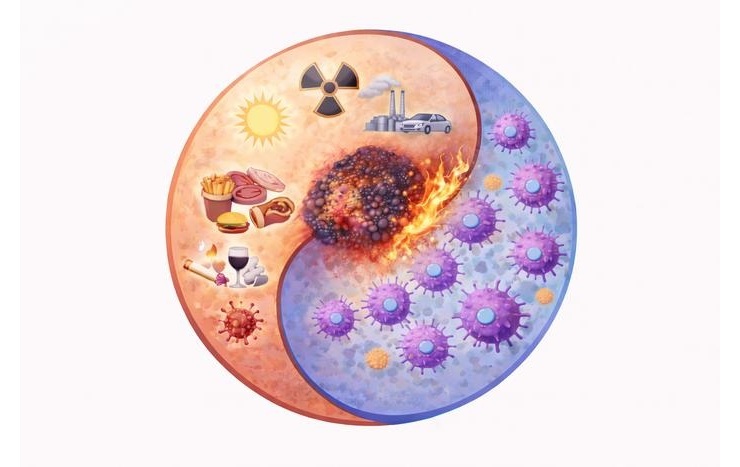
Cancer Mutation ‘Fingerprints’ to Improve Prediction of Immunotherapy Response
Cancer cells accumulate thousands of genetic mutations, but not all mutations affect tumors in the same way. Some make cancer cells more visible to the immune system, while others allow tumors to evade... Read more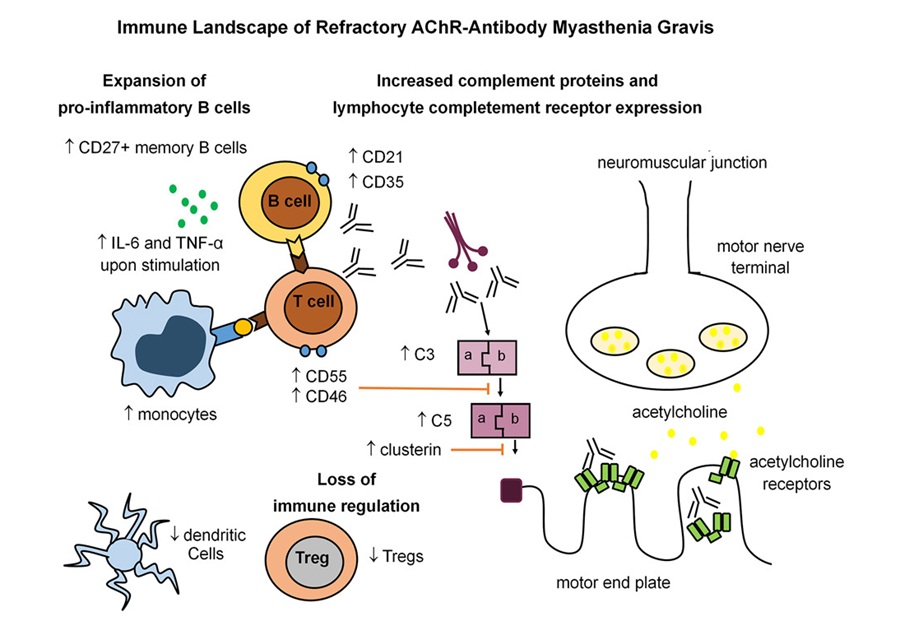
Immune Signature Identified in Treatment-Resistant Myasthenia Gravis
Myasthenia gravis is a rare autoimmune disorder in which immune attack at the neuromuscular junction causes fluctuating weakness that can impair vision, movement, speech, swallowing, and breathing.... Read more
New Biomarker Predicts Chemotherapy Response in Triple-Negative Breast Cancer
Triple-negative breast cancer is an aggressive form of breast cancer in which patients often show widely varying responses to chemotherapy. Predicting who will benefit from treatment remains challenging,... Read moreBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read moreMicrobiology
view channel
WHO Recommends Near POC Tests, Tongue Swabs and Sputum Pooling for TB Diagnosis
Tuberculosis (TB) remains one of the world’s leading infectious disease killers, yet millions of cases go undiagnosed or are detected too late. Barriers such as reliance on sputum samples, limited laboratory... Read more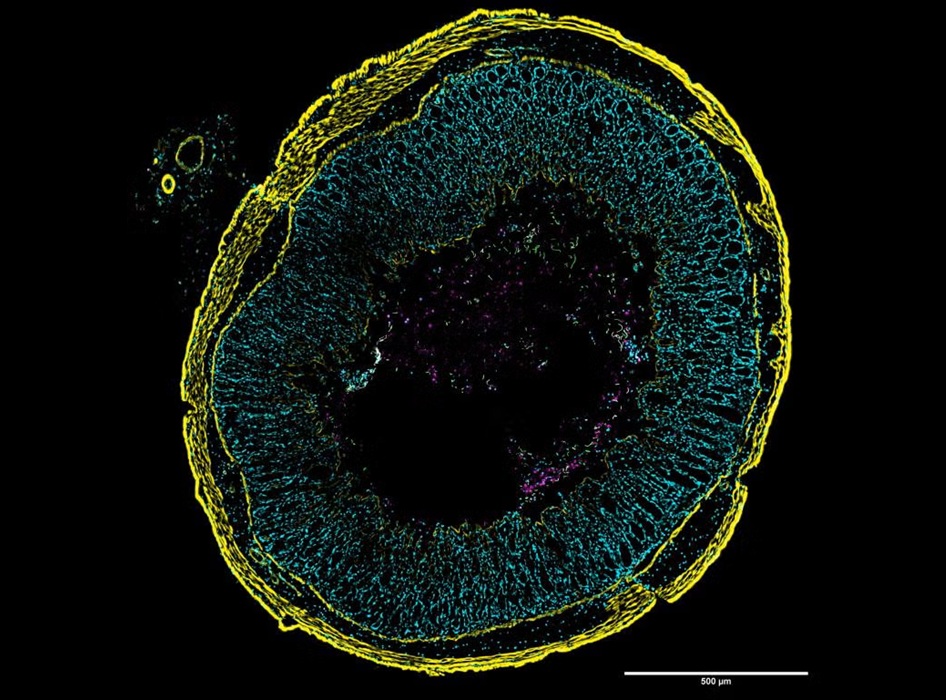
New Imaging Approach Could Help Predict Dangerous Gut Infection
Clostridioides difficile infections affect roughly half a million people in the United States each year and are a leading cause of infectious diarrhea in healthcare settings. The bacterium can trigger... Read morePathology
view channel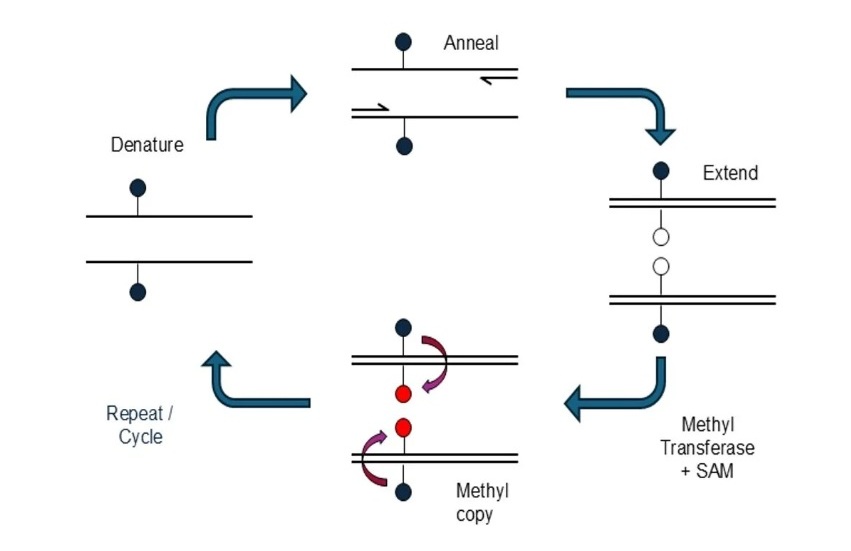
Novel mcPCR Technology to Transform Testing of Clinical Samples
DNA methylation is an important biological marker used in the diagnosis and monitoring of many diseases, including cancer. These chemical modifications to DNA influence gene activity and can reveal early... Read more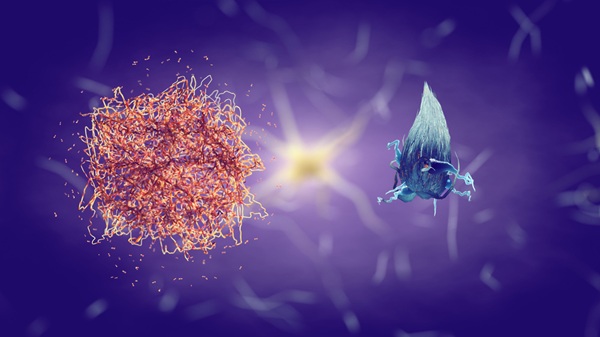
Sex Differences in Alzheimer’s Biomarkers Linked to Faster Cognitive Decline
Sex differences in Alzheimer’s disease present ongoing diagnostic challenges, with women often experiencing a disproportionate disease burden even when preclinical amyloid-beta levels are similar to men.... Read moreTechnology
view channel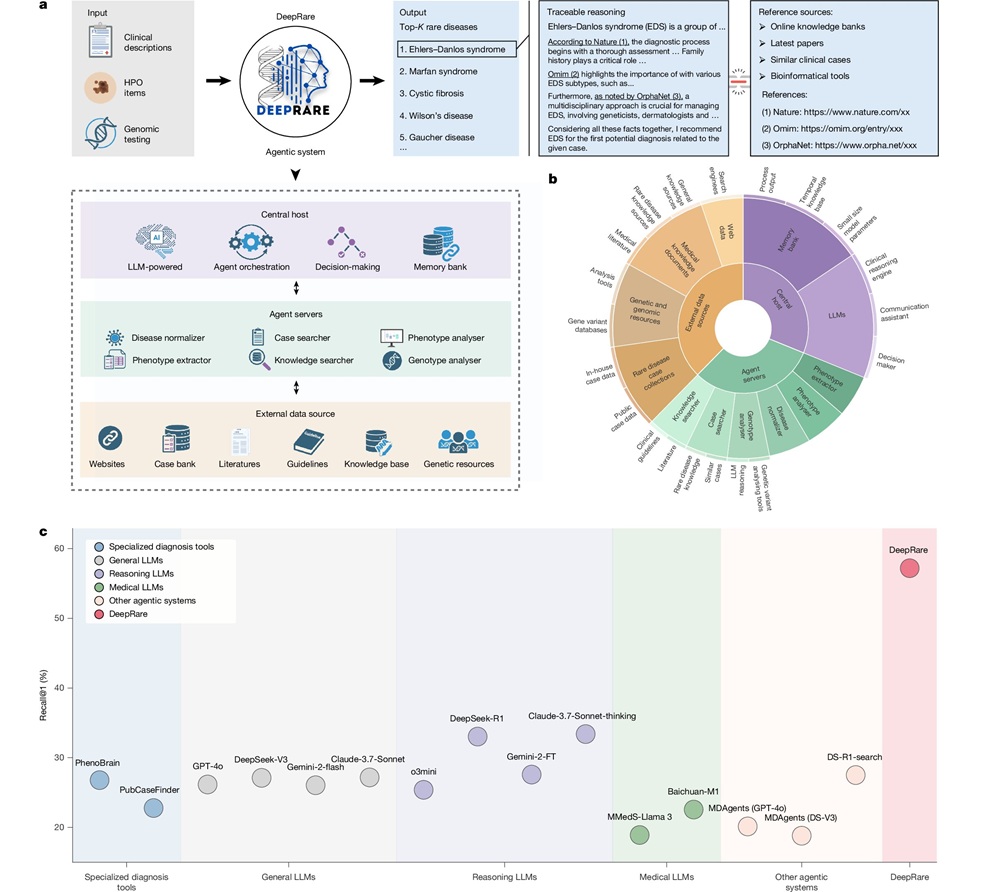
AI Model Outperforms Clinicians in Rare Disease Detection
Rare diseases affect an estimated 300 million people worldwide, yet diagnosis is often protracted and error-prone. Many conditions present with heterogeneous signs that overlap with common disorders, leading... Read more
AI-Driven Diagnostic Demonstrates High Accuracy in Detecting Periprosthetic Joint Infection
Periprosthetic joint infection (PJI) is a rare but serious complication affecting 1% to 2% of primary joint replacement surgeries. The condition occurs when bacteria or fungi infect tissues around an implanted... Read moreIndustry
view channel
Agilent Technologies Acquires Pathology Diagnostics Company Biocare Medical
Agilent Technologies (Santa Clara, CA, USA) has entered into a definitive agreement to acquire Biocare Medical (Pacheco, CA, USA), expanding its pathology portfolio through the addition of highly complementary... Read more
Cepheid Joins CDC Initiative to Strengthen U.S. Pandemic Testing Preparednesss
Cepheid (Sunnyvale, CA, USA) has been selected by the U.S. Centers for Disease Control and Prevention (CDC) as one of four national collaborators in a federal initiative to speed rapid diagnostic technologies... Read more
QuidelOrtho Collaborates with Lifotronic to Expand Global Immunoassay Portfolio
QuidelOrtho (San Diego, CA, USA) has entered a long-term strategic supply agreement with Lifotronic Technology (Shenzhen, China) to expand its global immunoassay portfolio and accelerate customer access... Read more