Combined Gene and Immunotherapy Shows Potential for Aggressive Brain Tumors
|
By LabMedica International staff writers Posted on 17 Jan 2017 |
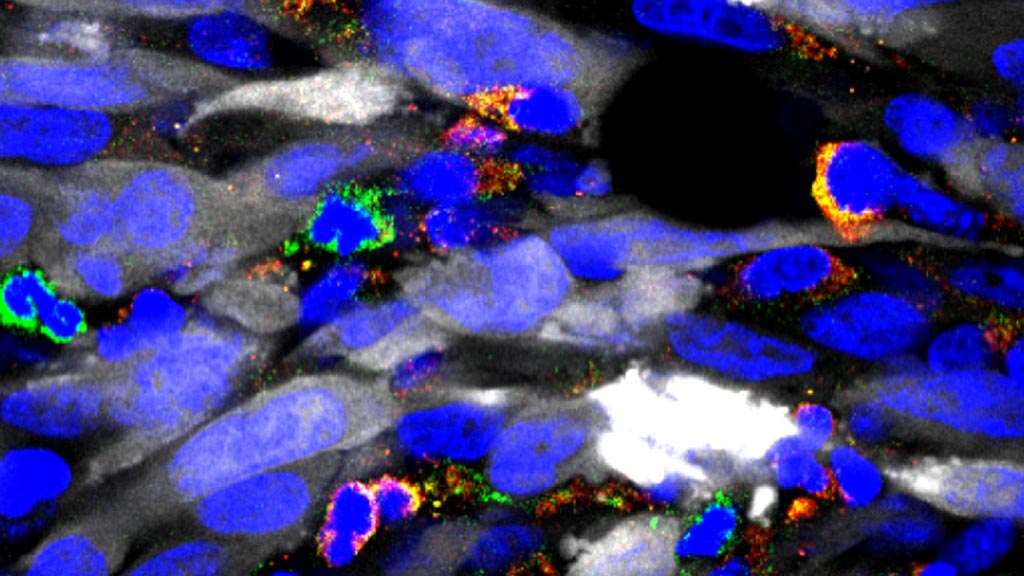
Image: A photomicrograph showing numerous immune suppressive cells in green and yellow, infiltrating the tumor mass (tumor cells in white). By depleting these immune suppressive cells, immunotherapy becomes much more effective (Photo courtesy of the University of Michigan).
A novel approach that combined gene and immunotherapy demonstrated considerable potential in a mouse model as a method for treating the aggressive brain tumor glioblastoma multiforme (GBM).
GBM is the most common primary tumor of the central nervous system and is almost always fatal. The aggressive invasion of GBM cells into the surrounding normal brain makes complete surgical removal impossible, significantly increases resistance to the standard therapy regimen, and virtually assures tumor recurrence. Median survival for newly diagnosed GBM is 14.6 months and declines to eight months for patients with recurrent GBM.
While immunotherapeutic approaches that harness the cytotoxic and memory potential of the host immune system have shown great benefit in other types of cancer. GBMs have developed multiple strategies, including the accumulation of myeloid-derived suppressor cells (MDSCs) to induce immunosuppression. MDSCs contribute to an immunosuppressive network that protects tumors by disabling T-cell adaptive immunity.
As it is imperative to develop multipronged approaches when aiming to generate a robust anti-tumor immune response, end investigators at the University of Michigan tested whether combining MDSC depletion or checkpoint blockade would increase the efficacy of immune-stimulatory herpes simplex type-I thymidine kinase (TK) plus Fms-like tyrosine kinase ligand (Flt3L)-mediated immune stimulatory gene therapy. The method used by the investigators on a mouse GBM model required injecting adenovirus vectors carrying herpes simplex 1 thymidine kinase into the tumor, followed by an antiviral, to elicit tumor cell death. This treatment was used in combination with another adenovirus vector carrying an immune stimulatory cytokine to recruit immune cells into the tumor.
Results published in the January 4, 2017, online edition of the journal Molecular Therapy revealed that MDSCs constituted more than 40% of the tumor-infiltrating immune cells. These cells expressed IL-4Ralpha, inducible nitric oxide synthase (iNOS), arginase, programmed death ligand 1 (PDL1), and CD80, molecules that are critically involved in antigen-specific T-cell suppression.
Depletion of MDSCs strongly enhanced the TK/Flt3L gene therapy-induced tumor-specific CD8 T-cell response, which led to an increased median survival and percentage of long-term survivors. Also, combining PDL1 or CTLA-4 immune checkpoint blockade greatly improved the efficacy of TK/Flt3L gene therapy.
"For the first time, we proved that a type of immunosuppressive cells within the tumor environment play a major role in determining the impact of immunotherapies," said senior author Dr. Maria Castro, professor of neurosurgery and cell and developmental biology at the University of Michigan. "We hope the implementation of our gene therapy strategy for gliomas, used in combination with immune checkpoint blockade, will eventually provide successful treatment for patients with this devastating brain cancer."
GBM is the most common primary tumor of the central nervous system and is almost always fatal. The aggressive invasion of GBM cells into the surrounding normal brain makes complete surgical removal impossible, significantly increases resistance to the standard therapy regimen, and virtually assures tumor recurrence. Median survival for newly diagnosed GBM is 14.6 months and declines to eight months for patients with recurrent GBM.
While immunotherapeutic approaches that harness the cytotoxic and memory potential of the host immune system have shown great benefit in other types of cancer. GBMs have developed multiple strategies, including the accumulation of myeloid-derived suppressor cells (MDSCs) to induce immunosuppression. MDSCs contribute to an immunosuppressive network that protects tumors by disabling T-cell adaptive immunity.
As it is imperative to develop multipronged approaches when aiming to generate a robust anti-tumor immune response, end investigators at the University of Michigan tested whether combining MDSC depletion or checkpoint blockade would increase the efficacy of immune-stimulatory herpes simplex type-I thymidine kinase (TK) plus Fms-like tyrosine kinase ligand (Flt3L)-mediated immune stimulatory gene therapy. The method used by the investigators on a mouse GBM model required injecting adenovirus vectors carrying herpes simplex 1 thymidine kinase into the tumor, followed by an antiviral, to elicit tumor cell death. This treatment was used in combination with another adenovirus vector carrying an immune stimulatory cytokine to recruit immune cells into the tumor.
Results published in the January 4, 2017, online edition of the journal Molecular Therapy revealed that MDSCs constituted more than 40% of the tumor-infiltrating immune cells. These cells expressed IL-4Ralpha, inducible nitric oxide synthase (iNOS), arginase, programmed death ligand 1 (PDL1), and CD80, molecules that are critically involved in antigen-specific T-cell suppression.
Depletion of MDSCs strongly enhanced the TK/Flt3L gene therapy-induced tumor-specific CD8 T-cell response, which led to an increased median survival and percentage of long-term survivors. Also, combining PDL1 or CTLA-4 immune checkpoint blockade greatly improved the efficacy of TK/Flt3L gene therapy.
"For the first time, we proved that a type of immunosuppressive cells within the tumor environment play a major role in determining the impact of immunotherapies," said senior author Dr. Maria Castro, professor of neurosurgery and cell and developmental biology at the University of Michigan. "We hope the implementation of our gene therapy strategy for gliomas, used in combination with immune checkpoint blockade, will eventually provide successful treatment for patients with this devastating brain cancer."
Latest BioResearch News
- Barcoded DNA Sheds Light on Hidden Complexities in Breast Cancer Detection
- CRISPR-Based Platform Pinpoints Drivers of Acute Myeloid Leukemia in Patient Cells
- Protective Brain Protein Emerges as Biomarker Target in Alzheimer’s Disease
- Genome Analysis Predicts Likelihood of Neurodisability in Oxygen-Deprived Newborns
- Gene Panel Predicts Disease Progession for Patients with B-cell Lymphoma
- New Method Simplifies Preparation of Tumor Genomic DNA Libraries
- New Tool Developed for Diagnosis of Chronic HBV Infection
- Panel of Genetic Loci Accurately Predicts Risk of Developing Gout
- Disrupted TGFB Signaling Linked to Increased Cancer-Related Bacteria
- Gene Fusion Protein Proposed as Prostate Cancer Biomarker
- NIV Test to Diagnose and Monitor Vascular Complications in Diabetes
- Semen Exosome MicroRNA Proves Biomarker for Prostate Cancer
- Genetic Loci Link Plasma Lipid Levels to CVD Risk
- Newly Identified Gene Network Aids in Early Diagnosis of Autism Spectrum Disorder
- Link Confirmed between Living in Poverty and Developing Diseases
- Genomic Study Identifies Kidney Disease Loci in Type I Diabetes Patients
Channels
Clinical Chemistry
view channelNew Blood Test Index Offers Earlier Detection of Liver Scarring
Metabolic fatty liver disease is highly prevalent and often silent, yet it can progress to fibrosis, cirrhosis, and liver failure. Current first-line blood test scores frequently return indeterminate results,... Read more
Electronic Nose Smells Early Signs of Ovarian Cancer in Blood
Ovarian cancer is often diagnosed at a late stage because its symptoms are vague and resemble those of more common conditions. Unlike breast cancer, there is currently no reliable screening method, and... Read moreMolecular Diagnostics
view channel
New Test Detects Alzheimer’s by Analyzing Altered Protein Shapes in Blood
Alzheimer’s disease begins developing years before memory loss or other symptoms become visible. Misfolded proteins gradually accumulate in the brain, disrupting normal cellular processes.... Read more
New Diagnostic Markers for Multiple Sclerosis Discovered in Cerebrospinal Fluid
Multiple sclerosis (MS) affects nearly three million people worldwide and can cause symptoms such as numbness, visual disturbances, fatigue, and neurological disability. Diagnosing the disease can be challenging... Read moreHematology
view channel
Rapid Cartridge-Based Test Aims to Expand Access to Hemoglobin Disorder Diagnosis
Sickle cell disease and beta thalassemia are hemoglobin disorders that often require referral to specialized laboratories for definitive diagnosis, delaying results for patients and clinicians.... Read more
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read moreImmunology
view channel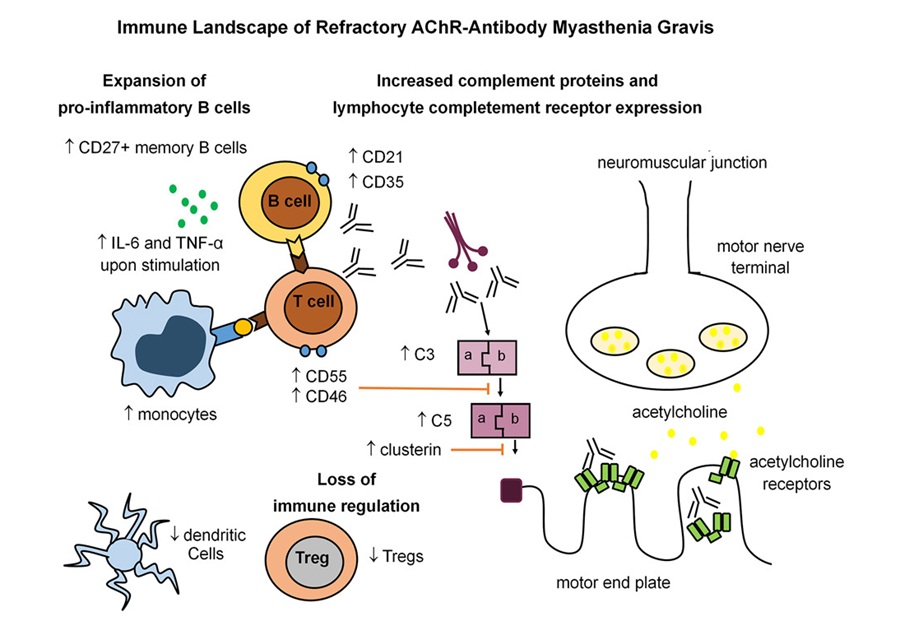
Immune Signature Identified in Treatment-Resistant Myasthenia Gravis
Myasthenia gravis is a rare autoimmune disorder in which immune attack at the neuromuscular junction causes fluctuating weakness that can impair vision, movement, speech, swallowing, and breathing.... Read more
New Biomarker Predicts Chemotherapy Response in Triple-Negative Breast Cancer
Triple-negative breast cancer is an aggressive form of breast cancer in which patients often show widely varying responses to chemotherapy. Predicting who will benefit from treatment remains challenging,... Read moreBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read moreMicrobiology
view channel
Blood-Based Viral Signature Identified in Crohn’s Disease
Crohn’s disease is a chronic inflammatory intestinal disorder affecting approximately 0.4% of the European population, with symptoms and progression that vary widely. Although viral components of the microbiome... Read more
Hidden Gut Viruses Linked to Colorectal Cancer Risk
Colorectal cancer (CRC) remains a leading cause of cancer mortality in many Western countries, and existing risk-stratification approaches leave substantial room for improvement. Although age, diet, and... Read morePathology
view channel
Molecular Imaging to Reduce Need for Melanoma Biopsies
Melanoma is the deadliest form of skin cancer and accounts for the vast majority of skin cancer-related deaths. Because early melanomas can closely resemble benign moles, clinicians often rely on visual... Read more
Urine Specimen Collection System Improves Diagnostic Accuracy and Efficiency
Urine testing is a critical, non-invasive diagnostic tool used to detect conditions such as pregnancy, urinary tract infections, metabolic disorders, cancer, and kidney disease. However, contaminated or... Read moreTechnology
view channel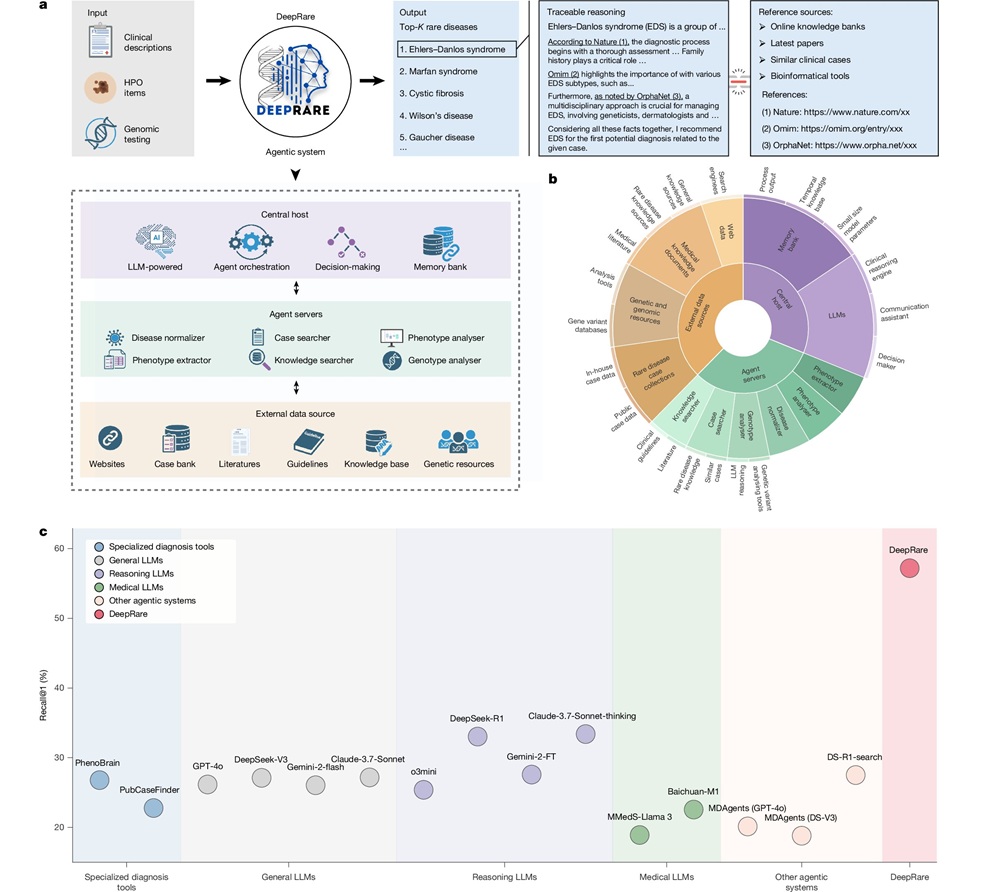
AI Model Outperforms Clinicians in Rare Disease Detection
Rare diseases affect an estimated 300 million people worldwide, yet diagnosis is often protracted and error-prone. Many conditions present with heterogeneous signs that overlap with common disorders, leading... Read more
AI-Driven Diagnostic Demonstrates High Accuracy in Detecting Periprosthetic Joint Infection
Periprosthetic joint infection (PJI) is a rare but serious complication affecting 1% to 2% of primary joint replacement surgeries. The condition occurs when bacteria or fungi infect tissues around an implanted... Read moreIndustry
view channel
Cepheid Joins CDC Initiative to Strengthen U.S. Pandemic Testing Preparednesss
Cepheid (Sunnyvale, CA, USA) has been selected by the U.S. Centers for Disease Control and Prevention (CDC) as one of four national collaborators in a federal initiative to speed rapid diagnostic technologies... Read more
QuidelOrtho Collaborates with Lifotronic to Expand Global Immunoassay Portfolio
QuidelOrtho (San Diego, CA, USA) has entered a long-term strategic supply agreement with Lifotronic Technology (Shenzhen, China) to expand its global immunoassay portfolio and accelerate customer access... Read more








 (3) (1).png)