Methodology Devised to Improve Stem Cell Reprogramming
|
By LabMedica International staff writers Posted on 27 Jan 2015 |
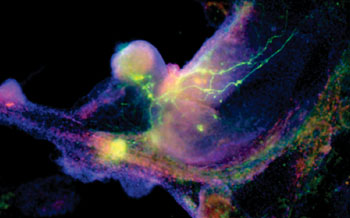
Image: Induced pluripotent stem (iPS) cells, which act very much like embryonic stem cells, are shown growing into heart cells (blue) and nerve cells (green) (Photo courtesy of Gladstone Institutes/Chris Goodfellow).
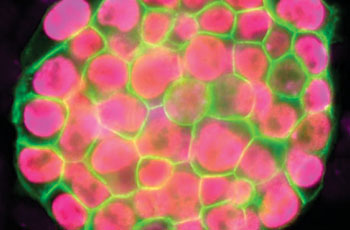
Image: Microscopic view of a colony of induced pluripotent stem cells obtained by reprogramming a specialized cell for two weeks (Photo courtesy of UCLA Broad Stem Cell Research Center/Plath Lab).
In a study that provides scientists with a critical new determination of stem cell development and its role in disease, researchers have established a first-of-its-kind approach that outlines the stages by which specialized cells are reprogrammed into stem cells resembling those found in embryos. The research could have wide ranging, long-term implications in enhancing disease modeling and devising new therapies for patients.
The study, conducted by researchers from the University of California, Los Angeles (UCLA; USA) Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research and led by Dr. Kathrin Plath, a professor of biological chemistry, was published January 2015 in the journal Cell. Induced pluripotent stem cells (iPSCs) are cells that can be generated from adult cells and then, like embryonic stem cells, be directed to become any cell in the human body. Adult cells can also be reprogrammed in the lab to change from a specialized cell back to an iPSC (and thereby becoming a cell similar to that of an embryonic stem cell).
Reprogramming takes one to two weeks and is a mostly inefficient process, with typically less than one percent of the beginning cells effectively becoming an iPSC. The exact stages a cell goes through during the reprogramming process are not well understood. This knowledge is vital, because iPSCs have great potential in the field of regenerative medicine, as they can constantly reproduce and provide a single source of patient-specific cells to replace those lost to injury or disease. They can also be used to create innovative disease models from which new drugs and therapies can be developed.
Vincent Pasque and Jason Tchieu, postdoctoral fellows in Plath’s lab and co-first authors of the study, developed a roadmap of the reprogramming process using detailed time-course analyses. They induced the reprogramming of specialized cells (that could only make more of themselves, and no other cell types), then observed and analyzed on a daily basis or every other day the process of transformation at the single-cell level. The data were gathered and recorded during a time period of up to two weeks.
Dr. Plath’s team found that the changes that happen in cells during reprogramming occur in sequentially, and that notably, the stages of the sequence were the same across the diverse reprogramming systems and different cell types analyzed. “The exact stage of reprogramming of any cell can now be determined,” Dr. Pasque said. “This study signals a big change in thinking, because it provides simple and efficient tools for scientists to study stem cell creation in a stage-by-stage manner. Most studies to date ignore the stages of reprogramming, but we can now seek to better understand the entire process on both a macro and micro level.”
Dr. Plath’s group additionally discovered that the stages of reprogramming to iPSC are different from what was expected. They found that it is not simply the reversed sequence of stages of embryo development. Some steps are reversed in the expected order; others do not actually happen in the exact reverse order and resist a change until late during reprogramming to iPSCs. “This reflects how cells do not like to change from one specialized cell type to another and resist a change in cell identity,” Dr. Pasque said. “Resistance to reprogramming also helps to explain why reprogramming takes place only in a very small proportion of the starting cells.”
With these findings, Dr. Plath’s lab plans future studies to actively isolate specific cell types during specific stages of reprogramming. They also hope the research will encourage further investigation into the characteristics of iPSC development. “This research has broad impact, because by understanding cell reprogramming better we have the potential to improve disease modeling and the generation of better sources of patient-specific specialized cells suitable for replacement therapy,” concluded Dr. Plath. “This can ultimately benefit patients with new and better treatments for a wide range of diseases.”
Related Links:
University of California, Los Angeles’ Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research
The study, conducted by researchers from the University of California, Los Angeles (UCLA; USA) Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research and led by Dr. Kathrin Plath, a professor of biological chemistry, was published January 2015 in the journal Cell. Induced pluripotent stem cells (iPSCs) are cells that can be generated from adult cells and then, like embryonic stem cells, be directed to become any cell in the human body. Adult cells can also be reprogrammed in the lab to change from a specialized cell back to an iPSC (and thereby becoming a cell similar to that of an embryonic stem cell).
Reprogramming takes one to two weeks and is a mostly inefficient process, with typically less than one percent of the beginning cells effectively becoming an iPSC. The exact stages a cell goes through during the reprogramming process are not well understood. This knowledge is vital, because iPSCs have great potential in the field of regenerative medicine, as they can constantly reproduce and provide a single source of patient-specific cells to replace those lost to injury or disease. They can also be used to create innovative disease models from which new drugs and therapies can be developed.
Vincent Pasque and Jason Tchieu, postdoctoral fellows in Plath’s lab and co-first authors of the study, developed a roadmap of the reprogramming process using detailed time-course analyses. They induced the reprogramming of specialized cells (that could only make more of themselves, and no other cell types), then observed and analyzed on a daily basis or every other day the process of transformation at the single-cell level. The data were gathered and recorded during a time period of up to two weeks.
Dr. Plath’s team found that the changes that happen in cells during reprogramming occur in sequentially, and that notably, the stages of the sequence were the same across the diverse reprogramming systems and different cell types analyzed. “The exact stage of reprogramming of any cell can now be determined,” Dr. Pasque said. “This study signals a big change in thinking, because it provides simple and efficient tools for scientists to study stem cell creation in a stage-by-stage manner. Most studies to date ignore the stages of reprogramming, but we can now seek to better understand the entire process on both a macro and micro level.”
Dr. Plath’s group additionally discovered that the stages of reprogramming to iPSC are different from what was expected. They found that it is not simply the reversed sequence of stages of embryo development. Some steps are reversed in the expected order; others do not actually happen in the exact reverse order and resist a change until late during reprogramming to iPSCs. “This reflects how cells do not like to change from one specialized cell type to another and resist a change in cell identity,” Dr. Pasque said. “Resistance to reprogramming also helps to explain why reprogramming takes place only in a very small proportion of the starting cells.”
With these findings, Dr. Plath’s lab plans future studies to actively isolate specific cell types during specific stages of reprogramming. They also hope the research will encourage further investigation into the characteristics of iPSC development. “This research has broad impact, because by understanding cell reprogramming better we have the potential to improve disease modeling and the generation of better sources of patient-specific specialized cells suitable for replacement therapy,” concluded Dr. Plath. “This can ultimately benefit patients with new and better treatments for a wide range of diseases.”
Related Links:
University of California, Los Angeles’ Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research
Latest BioResearch News
- Genome Analysis Predicts Likelihood of Neurodisability in Oxygen-Deprived Newborns
- Gene Panel Predicts Disease Progession for Patients with B-cell Lymphoma
- New Method Simplifies Preparation of Tumor Genomic DNA Libraries
- New Tool Developed for Diagnosis of Chronic HBV Infection
- Panel of Genetic Loci Accurately Predicts Risk of Developing Gout
- Disrupted TGFB Signaling Linked to Increased Cancer-Related Bacteria
- Gene Fusion Protein Proposed as Prostate Cancer Biomarker
- NIV Test to Diagnose and Monitor Vascular Complications in Diabetes
- Semen Exosome MicroRNA Proves Biomarker for Prostate Cancer
- Genetic Loci Link Plasma Lipid Levels to CVD Risk
- Newly Identified Gene Network Aids in Early Diagnosis of Autism Spectrum Disorder
- Link Confirmed between Living in Poverty and Developing Diseases
- Genomic Study Identifies Kidney Disease Loci in Type I Diabetes Patients
- Liquid Biopsy More Effective for Analyzing Tumor Drug Resistance Mutations
- New Liquid Biopsy Assay Reveals Host-Pathogen Interactions
- Method Developed for Enriching Trophoblast Population in Samples
Channels
Clinical Chemistry
view channel
Electronic Nose Smells Early Signs of Ovarian Cancer in Blood
Ovarian cancer is often diagnosed at a late stage because its symptoms are vague and resemble those of more common conditions. Unlike breast cancer, there is currently no reliable screening method, and... Read more
Simple Blood Test Offers New Path to Alzheimer’s Assessment in Primary Care
Timely evaluation of cognitive symptoms in primary care is often limited by restricted access to specialized diagnostics and invasive confirmatory procedures. Clinicians need accessible tools to determine... Read moreMolecular Diagnostics
view channel
Genetic Test Predicts Radiation Therapy Risk for Prostate Cancer Patients
External beam radiation therapy is widely used to treat localized prostate cancer, which has a five-year survival rate exceeding 99%. However, more than 20% of patients develop persistent urinary side... Read more
Genetic Test Aids Early Detection and Improved Treatment for Cancers
Lynch syndrome is a hereditary genetic condition that significantly increases the risk of several cancers, including those of the bowel and urinary tract. Urinary tract cancers—affecting the kidney, bladder,... Read moreHematology
view channel
Rapid Cartridge-Based Test Aims to Expand Access to Hemoglobin Disorder Diagnosis
Sickle cell disease and beta thalassemia are hemoglobin disorders that often require referral to specialized laboratories for definitive diagnosis, delaying results for patients and clinicians.... Read more
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read moreImmunology
view channel
New Biomarker Predicts Chemotherapy Response in Triple-Negative Breast Cancer
Triple-negative breast cancer is an aggressive form of breast cancer in which patients often show widely varying responses to chemotherapy. Predicting who will benefit from treatment remains challenging,... Read moreBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read more
Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
Immunotherapy has transformed cancer treatment, but only a small proportion of patients experience lasting benefit, with response rates often remaining between 10% and 20%. Clinicians currently lack reliable... Read moreMicrobiology
view channel
Three-Test Panel Launched for Detection of Liver Fluke Infections
Parasitic liver fluke infections remain endemic in parts of Asia, where transmission commonly occurs through consumption of raw freshwater fish or aquatic plants. Chronic infection is a well-established... Read more
Rapid Test Promises Faster Answers for Drug-Resistant Infections
Drug-resistant pathogens continue to pose a growing threat in healthcare facilities, where delayed detection can impede outbreak control and increase mortality. Candida auris is notoriously difficult to... Read more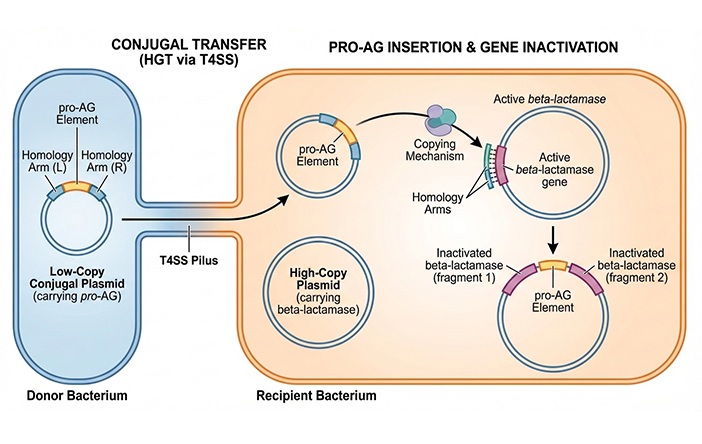
CRISPR-Based Technology Neutralizes Antibiotic-Resistant Bacteria
Antibiotic resistance has accelerated into a global health crisis, with projections estimating more than 10 million deaths per year by 2050 as drug-resistant “superbugs” continue to spread.... Read more
Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
Alzheimer’s disease affects approximately 6.7 million people in the United States and nearly 50 million worldwide, yet early cognitive decline remains difficult to characterize. Increasing evidence suggests... Read morePathology
view channel
Urine Specimen Collection System Improves Diagnostic Accuracy and Efficiency
Urine testing is a critical, non-invasive diagnostic tool used to detect conditions such as pregnancy, urinary tract infections, metabolic disorders, cancer, and kidney disease. However, contaminated or... Read more
AI-Powered 3D Scanning System Speeds Cancer Screening
Cytology remains a cornerstone of cancer detection, requiring specialists to examine bodily fluids and cells under a microscope. This labor-intensive process involves inspecting up to one million cells... Read moreTechnology
view channel
Blood Test “Clocks” Predict Start of Alzheimer’s Symptoms
More than 7 million Americans live with Alzheimer’s disease, and related health and long-term care costs are projected to reach nearly USD 400 billion in 2025. The disease has no cure, and symptoms often... Read more
AI-Powered Biomarker Predicts Liver Cancer Risk
Liver cancer, or hepatocellular carcinoma, causes more than 800,000 deaths worldwide each year and often goes undetected until late stages. Even after treatment, recurrence rates reach 70% to 80%, contributing... Read more
Robotic Technology Unveiled for Automated Diagnostic Blood Draws
Routine diagnostic blood collection is a high‑volume task that can strain staffing and introduce human‑dependent variability, with downstream implications for sample quality and patient experience.... Read more
ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
Clinical laboratories generate billions of test results each year, creating a treasure trove of data with the potential to support more personalized testing, improve operational efficiency, and enhance patient care.... Read moreIndustry
view channel
QuidelOrtho Collaborates with Lifotronic to Expand Global Immunoassay Portfolio
QuidelOrtho (San Diego, CA, USA) has entered a long-term strategic supply agreement with Lifotronic Technology (Shenzhen, China) to expand its global immunoassay portfolio and accelerate customer access... Read more










 (3) (1).png)