New Technology Rapidly Diagnoses Sickle Cell Disease
|
By LabMedica International staff writers Posted on 29 Oct 2020 |
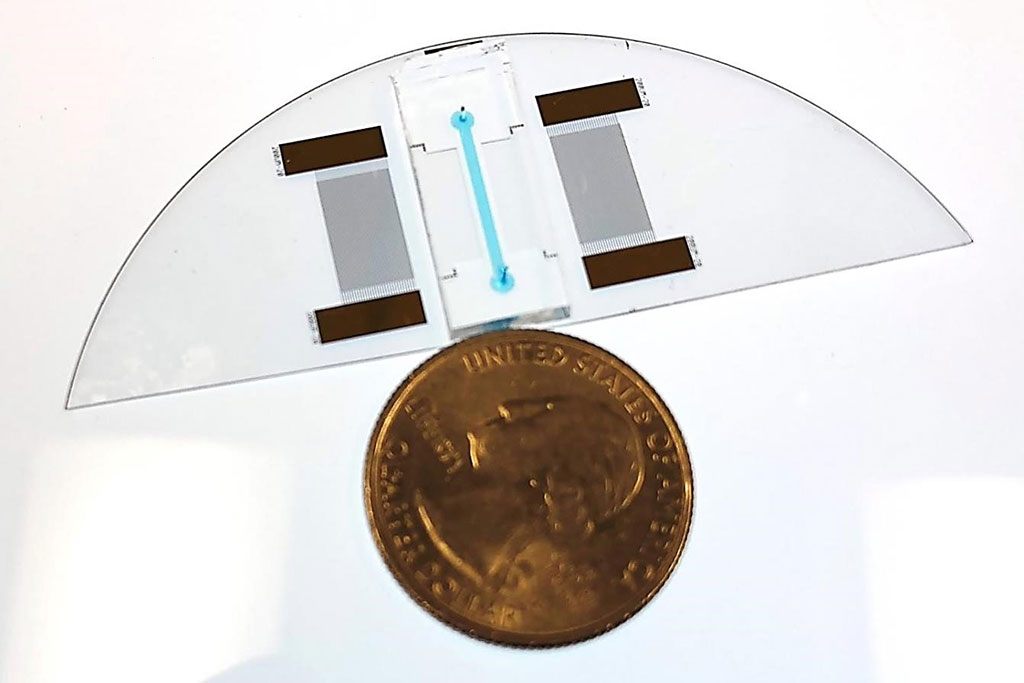
Image: An Acousto Thermal Shift Assay `lab-on-a-chip` device shown next to a US quarter for size comparison. The device can diagnose sickle cell anemia (Photo courtesy of CU Boulder College of Engineering and Applied Science).
Sickle cell disease (SCD) is a group of blood disorders typically inherited from a person's parents. The most common type is known as sickle cell anemia (SCA). It results in an abnormality in the oxygen-carrying protein hemoglobin found in red blood cells.
Sickle cell disease occurs when a person inherits two abnormal copies of the β-globin gene that makes hemoglobin, one from each parent. This gene occurs in chromosome 11. Several subtypes exist, depending on the exact mutation in each hemoglobin gene. An attack can be set off by temperature changes, stress, dehydration, and high altitude.
Molecular, Cellular and Developmental Biologists at the University of Colorado, (Boulder, CO, USA) have developed a new way to diagnose diseases of the blood like sickle cell disease with sensitivity and precision and in only one minute. Their technology is smaller than a quarter and requires only a small droplet of blood to assess protein interactions, dysfunction or mutations. The team used Thermal Shift Assays (TSAs) to assess protein stability under varying conditions. Such tests took about a day to run. Now, with the new technology, an Acousto Thermal Shift Assay (ATSA), they can do the same but faster and with greater sensitivity.
Proteins have a specific solubility at a specific temperature. The solubility changes when one protein bonds to another, or when the protein is mutated, by measuring solubility at different temperatures, scientists can tell whether the protein has been mutating. The ATSA utilizes high-amplitude sound waves, or ultrasound, to heat a protein sample. The tool then measures data continuously, recording how much of the protein has dissolved at every fraction of change in degrees Celsius. The ATSA requires only a power source, a microscope and a camera as simple as the one on a smartphone. Because the protein is concentrated, there is also no need to apply a florescent dye as is sometimes required to highlight protein changes in a traditional TSA.
Yonghui Ding, PhD, a post-doctoral fellow and the first author of the study, said, “The method is seven to 34 times more sensitive. The ATSA can distinguish the sickle cell protein from normal protein, while the traditional TSA method cannot.” The study was published on October 15, 2020 in the journal Small.
Related Links:
University of Colorado
Sickle cell disease occurs when a person inherits two abnormal copies of the β-globin gene that makes hemoglobin, one from each parent. This gene occurs in chromosome 11. Several subtypes exist, depending on the exact mutation in each hemoglobin gene. An attack can be set off by temperature changes, stress, dehydration, and high altitude.
Molecular, Cellular and Developmental Biologists at the University of Colorado, (Boulder, CO, USA) have developed a new way to diagnose diseases of the blood like sickle cell disease with sensitivity and precision and in only one minute. Their technology is smaller than a quarter and requires only a small droplet of blood to assess protein interactions, dysfunction or mutations. The team used Thermal Shift Assays (TSAs) to assess protein stability under varying conditions. Such tests took about a day to run. Now, with the new technology, an Acousto Thermal Shift Assay (ATSA), they can do the same but faster and with greater sensitivity.
Proteins have a specific solubility at a specific temperature. The solubility changes when one protein bonds to another, or when the protein is mutated, by measuring solubility at different temperatures, scientists can tell whether the protein has been mutating. The ATSA utilizes high-amplitude sound waves, or ultrasound, to heat a protein sample. The tool then measures data continuously, recording how much of the protein has dissolved at every fraction of change in degrees Celsius. The ATSA requires only a power source, a microscope and a camera as simple as the one on a smartphone. Because the protein is concentrated, there is also no need to apply a florescent dye as is sometimes required to highlight protein changes in a traditional TSA.
Yonghui Ding, PhD, a post-doctoral fellow and the first author of the study, said, “The method is seven to 34 times more sensitive. The ATSA can distinguish the sickle cell protein from normal protein, while the traditional TSA method cannot.” The study was published on October 15, 2020 in the journal Small.
Related Links:
University of Colorado
Latest Technology News
- Blood Test “Clocks” Predict Start of Alzheimer’s Symptoms
- AI-Powered Biomarker Predicts Liver Cancer Risk
- Robotic Technology Unveiled for Automated Diagnostic Blood Draws
- ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
- Aptamer Biosensor Technology to Transform Virus Detection
- AI Models Could Predict Pre-Eclampsia and Anemia Earlier Using Routine Blood Tests
- AI-Generated Sensors Open New Paths for Early Cancer Detection
- Pioneering Blood Test Detects Lung Cancer Using Infrared Imaging
- AI Predicts Colorectal Cancer Survival Using Clinical and Molecular Features
Channels
Clinical Chemistry
view channel
Existing Hospital Analyzers Can Identify Fake Liquid Medical Products
Counterfeit and substandard medicines remain a serious global health threat, with World Health Organization estimates suggesting that 10.5% of medicines in low- and middle-income countries are either fake... Read more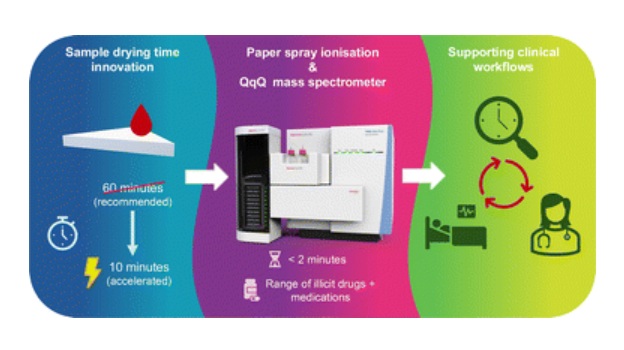
Rapid Blood Testing Method Aids Safer Decision-Making in Drug-Related Emergencies
Acute recreational drug toxicity is a frequent reason for emergency department visits, yet clinicians rarely have access to confirmatory toxicology results in real time. Instead, treatment decisions are... Read moreMolecular Diagnostics
view channel
New Extraction Kit Enables Consistent, Scalable cfDNA Isolation from Multiple Biofluids
Circulating cell-free DNA (cfDNA) found in plasma, serum, urine, and cerebrospinal fluid is typically present at low concentrations and is often highly fragmented, making efficient recovery challenging... Read more
AI-Powered Liquid Biopsy Classifies Pediatric Brain Tumors with High Accuracy
Liquid biopsies offer a noninvasive way to study cancer by analyzing circulating tumor DNA in body fluids. However, in pediatric brain tumors, the small amount of ctDNA in cerebrospinal fluid has limited... Read moreImmunology
view channel
New Biomarker Predicts Chemotherapy Response in Triple-Negative Breast Cancer
Triple-negative breast cancer is an aggressive form of breast cancer in which patients often show widely varying responses to chemotherapy. Predicting who will benefit from treatment remains challenging,... Read moreBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read more
Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
Immunotherapy has transformed cancer treatment, but only a small proportion of patients experience lasting benefit, with response rates often remaining between 10% and 20%. Clinicians currently lack reliable... Read moreMicrobiology
view channel
Rapid Test Promises Faster Answers for Drug-Resistant Infections
Drug-resistant pathogens continue to pose a growing threat in healthcare facilities, where delayed detection can impede outbreak control and increase mortality. Candida auris is notoriously difficult to... Read more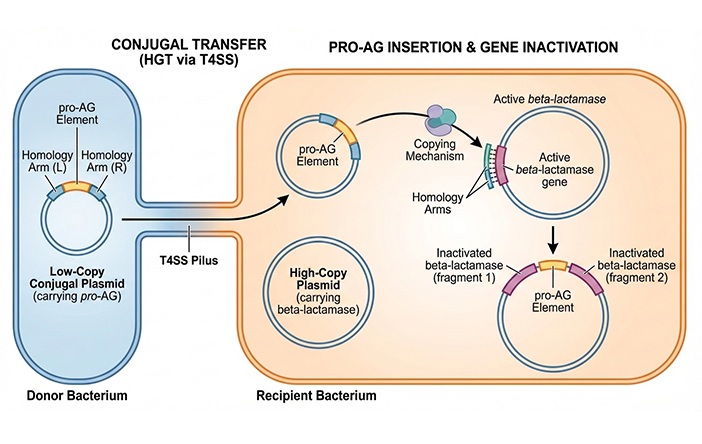
CRISPR-Based Technology Neutralizes Antibiotic-Resistant Bacteria
Antibiotic resistance has accelerated into a global health crisis, with projections estimating more than 10 million deaths per year by 2050 as drug-resistant “superbugs” continue to spread.... Read more
Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
Alzheimer’s disease affects approximately 6.7 million people in the United States and nearly 50 million worldwide, yet early cognitive decline remains difficult to characterize. Increasing evidence suggests... Read morePathology
view channel
Single Sample Classifier Predicts Cancer-Associated Fibroblast Subtypes in Patient Samples
Pancreatic ductal adenocarcinoma (PDAC) remains one of the deadliest cancers, in part because of its dense tumor microenvironment that influences how tumors grow and respond to treatment.... Read more
New AI-Driven Platform Standardizes Tuberculosis Smear Microscopy Workflow
Sputum smear microscopy remains central to tuberculosis treatment monitoring and follow-up, particularly in high‑burden settings where serial testing is routine. Yet consistent, repeatable bacillary assessment... Read more
AI Tool Uses Blood Biomarkers to Predict Transplant Complications Before Symptoms Appear
Stem cell and bone marrow transplants can be lifesaving, but serious complications may arise months after patients leave the hospital. One of the most dangerous is chronic graft-versus-host disease, in... Read moreTechnology
view channel
Blood Test “Clocks” Predict Start of Alzheimer’s Symptoms
More than 7 million Americans live with Alzheimer’s disease, and related health and long-term care costs are projected to reach nearly USD 400 billion in 2025. The disease has no cure, and symptoms often... Read more
AI-Powered Biomarker Predicts Liver Cancer Risk
Liver cancer, or hepatocellular carcinoma, causes more than 800,000 deaths worldwide each year and often goes undetected until late stages. Even after treatment, recurrence rates reach 70% to 80%, contributing... Read more
Robotic Technology Unveiled for Automated Diagnostic Blood Draws
Routine diagnostic blood collection is a high‑volume task that can strain staffing and introduce human‑dependent variability, with downstream implications for sample quality and patient experience.... Read more
ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
Clinical laboratories generate billions of test results each year, creating a treasure trove of data with the potential to support more personalized testing, improve operational efficiency, and enhance patient care.... Read moreIndustry
view channel
QuidelOrtho Collaborates with Lifotronic to Expand Global Immunoassay Portfolio
QuidelOrtho (San Diego, CA, USA) has entered a long-term strategic supply agreement with Lifotronic Technology (Shenzhen, China) to expand its global immunoassay portfolio and accelerate customer access... Read more









 Analyzer.jpg)