Sperm DNA Fragmentation – The New Frontier of Fertility Testing
|
By Whitney J. Palmer Posted on 29 Jul 2019 |

(Photo courtesy of AACC)
Worldwide male fertility has followed a disconcerting trend over the last 40 years. Since the 1970s, research shows sperm counts have plummeted by more than 50% in the United States, Europe, Australia, and New Zealand. Because the downward trajectory shows no sign of slowing or rebounding, being able to accurately assess male fertility and its impact on achieving a successful pregnancy has become more critical.
Overall, infertility affects between 10% and 15% of men in prime reproductive age. However, in as many as 15% of cases, conventional semen analysis, based on parameters established by the World Health Organization (WHO), does not identify sperm abnormalities that could cause decreased fertility (Box, below). While the WHO parameters, set in 2010, test volume, sperm count, and motility, they only provide information about sperm presence—not how effectively the sperm will fertilize an oocyte and foster a viable pregnancy.
That means men who fall within normal WHO ranges can still have significant sperm DNA damage. Consequently, there is a need for a technique that provides more detailed information about sperm quality. In the last decade, sperm DNA fragmentation (SDF) has emerged as a possible tool to highlight the level of molecular damage present in a man’s sperm. Several SDF tests are currently available, and the results can guide treatment option selections and fertility services. But reservations remain about how widely applicable and accepted SDF should be.
TESTING OPTIONS
SDF differs from raw semen analysis by examining the number of nicks and breaks present in the sperm’s DNA. Four main tests exist to identify a man’s DNA Fragmentation Index—the proportion of normal-to-damaged sperm—and each strategy is unique.
Sperm chromatin structure assay uses a chemical dye to stain broken sperm red and normal sperm green. Sperm chromatin dispersion treats sperm with acid denaturation after which normal sperm produce halos. Terminal deoxynucleotidyl transferase 2′-deoxyuridine 5′-triphosphates (dUTP) nick end labeling employs fluorescent dUTP to label single- and -double-strand breaks. And, SpermComet uses single-cell gel electrophoresis in which only -fragmented sperm travel through the gel.
Although the mechanisms are varied, these tests are valuable to couples who have not been able to identify the root of their infertility, said James Hotaling, MD, assistant professor of surgery and co-director of the Fertility Integrated Practice Unit at the University of Utah School of Medicine in Salt Lake City.
“SDF is the only test that allows us to look at anything other than bulk semen parameters,” he explained. “It lets us look at that quality of the DNA packaging critical for early embryo development.”
A PROMISING APPROACH
Every man has sperm DNA imperfections, said Mary Samplaski, MD, an assistant professor of urology at the University of Southern California Keck School of Medicine in Los Angeles, but levels are higher among sub-fertile and infertile men. High SDF, loosely defined as more than 30%, correlates with all reproductive outcomes, including lower success rates in natural pregnancy, intrauterine insemination, and in vitro fertilization (IVF), as well as higher miscarriage occurrences.
Several factors lead to this damage, said Ashok Agarwal, PhD, director of the Cleveland Clinic Clinical Andrology Lab and Sperm Bank. Oxidative stress, abortive apoptosis, and environmental factors, such as ultraviolet light and cellphone radiation, all can negatively impact DNA. Lifestyle factors, including obesity, diabetes, and sedentary occupations, also pose damage to sperm. Additionally, varicoceles—enlarged testicular veins that cause overheating and injure sperm—are present in approximately 40% of men with infertility.
With SDF test results in hand, reproductive specialists can recommend necessary lifestyle changes and guide patients toward the fertility treatment options that offer the best opportunities for success, he said.
“Rather than having a patient undergo and play Russian roulette with expensive technologies like IVF or [intracytoplasmic sperm injection] that can cost $10,000 to $15,000 per attempt with less than a 30% success rate,” he said, “we can avoid pricey and unnecessary treatments for couples with male factor infertility having repeated IVF failure or recurrent pregnancy loss by using SDF outcomes to reduce the DNA damage before undergoing assisted reproduction treatment.”
Samplaski agreed, noting that SDF offers vital information, pointing couples struggling with infertility down the right path as early as possible during their best reproductive years. That includes, she added, suggesting men take an antioxidant to counteract any oxidative stress damage.
SDF also supports clinical procedures that reduce DNA damage, according to Sheena Lewis, PhD, FRSB, emeritus professor at Queen’s University Belfast School of Medicine, Dentistry, and Biomedical Sciences in Northern Ireland. Removing sperm via testicular biopsy, before it picks up oxidative stress damage traveling along the epididymis (which she called the “war zone”), can yield healthier sperm for fertility procedures. Varicocele repair also offers similar improvement, she said. In fact, research shows men can experience a 3.4% damage reduction within 3 months via SDF retesting (Int Urol Nephrol 2015;47:1471–7).
WHAT IS HOLDING SDF BACK?
Despite providing a greater degree of actionable information, SDF still lags in the quest for widespread implementation. To a large degree, ease of access is a stumbling block, according to Amin S. Herati, MD, assistant -professor of urology and director of male infertility at the Brady Urological Institute at the Johns Hopkins School of Medicine in Baltimore. “For these tests, access for patients and providers is a big issue,” he said. “Only select labs offer it. Not everyone does it.”
Agarwal agreed, but he did not recommend every lab offer these tests as an in-house service. Instead, he said, they should identify a specialty lab, such as his own, already equipped with properly trained personnel, lab space, and equipment to process SDF tests to meet their needs.
Consistency and translatability have also been obstacles. Not only does each SDF test assess DNA fragmentation differently, each also has its own cut point to diagnose sperm quality levels. To make tests more easily accepted, procedures and results reporting must be standardized, Hotaling emphasized.
“There’s a lot of variability in how the test is run,” he said. “It’s not the same from one place to another, so it’s hard to compare results between labs.” Samplaski concurred, saying the level of existing differentiation makes reproductive specialists reticent to order SDF tests more frequently.
As with all other tests, though, until SDF methods are analyzed in larger clinical trials and submit reliable, reproducible results, providers will remain hesitant about suggesting the test for a wider patient population. Even as an initial SDF advocate, Herati acknowledged that the data to support the methods’ robust use has not appeared so far. However, these functional tests provide actionable information for a certain group of men struggling with infertility.
“I still use sperm DNA fragmentation, but its main role in my mind is for someone with normal semen parameters whose partner might have recurrent pregnancy loss,” Herati said. “We can decide where the sperm should come from for fertility services and what we can do to optimize that choice. That’s really where the utility of DNA fragmentation lies.”
Still, Agarwal said, SDF is one of the most important male fertility advancements in the last 60 years. Although it’s still in the early adoption phase, it offers hope for a successful pregnancy in cases when male-factor infertility was previously undiagnosed.
“Infertility is complicated, and sperm DNA fragmentation is an important part of testing in male patients, but it isn’t a silver bullet,” he emphasized. “It’s one way to examine, look for, and find hidden problems that aren’t told by semen analysis, and that’s a big thing. But, it’s not for every patient who has a problem with infertility.”
Sheena Lewis is the founder of Examen, producer of the SpermCOMET test and managing director of Lewis Fertility Testing, Ltd., a spin-out company of Queen’s University Belfast.
Whitney J. Palmer is a freelance journalist in Holly Springs, North Carolina. Email: whitneyljhowell@gmail.com
At the 71st AACC Annual Scientific Meeting & Clinical Lab Expo, scientific sessions cover a wide array of dynamic areas of clinical laboratory medicine. For sessions related to this and other cutting-edge laboratory methods visit https://2019aacc.org/conference-program.
Overall, infertility affects between 10% and 15% of men in prime reproductive age. However, in as many as 15% of cases, conventional semen analysis, based on parameters established by the World Health Organization (WHO), does not identify sperm abnormalities that could cause decreased fertility (Box, below). While the WHO parameters, set in 2010, test volume, sperm count, and motility, they only provide information about sperm presence—not how effectively the sperm will fertilize an oocyte and foster a viable pregnancy.
That means men who fall within normal WHO ranges can still have significant sperm DNA damage. Consequently, there is a need for a technique that provides more detailed information about sperm quality. In the last decade, sperm DNA fragmentation (SDF) has emerged as a possible tool to highlight the level of molecular damage present in a man’s sperm. Several SDF tests are currently available, and the results can guide treatment option selections and fertility services. But reservations remain about how widely applicable and accepted SDF should be.
TESTING OPTIONS
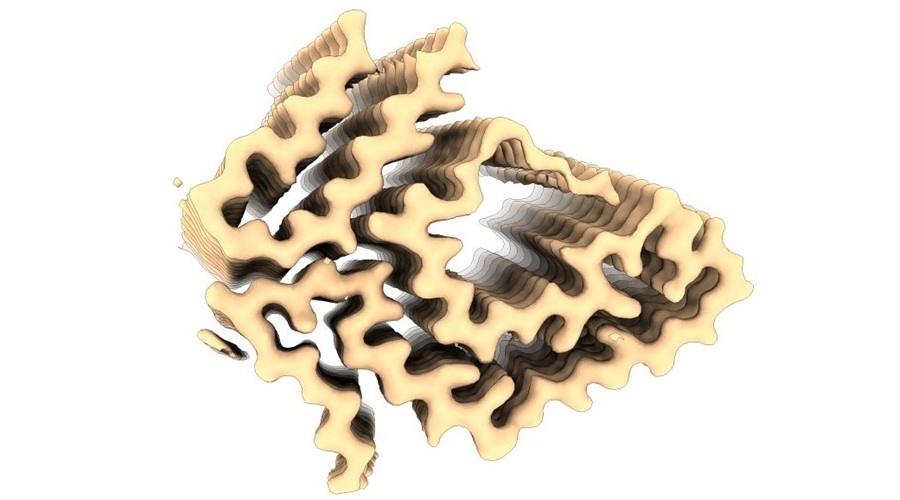
SDF differs from raw semen analysis by examining the number of nicks and breaks present in the sperm’s DNA. Four main tests exist to identify a man’s DNA Fragmentation Index—the proportion of normal-to-damaged sperm—and each strategy is unique.
Sperm chromatin structure assay uses a chemical dye to stain broken sperm red and normal sperm green. Sperm chromatin dispersion treats sperm with acid denaturation after which normal sperm produce halos. Terminal deoxynucleotidyl transferase 2′-deoxyuridine 5′-triphosphates (dUTP) nick end labeling employs fluorescent dUTP to label single- and -double-strand breaks. And, SpermComet uses single-cell gel electrophoresis in which only -fragmented sperm travel through the gel.
Although the mechanisms are varied, these tests are valuable to couples who have not been able to identify the root of their infertility, said James Hotaling, MD, assistant professor of surgery and co-director of the Fertility Integrated Practice Unit at the University of Utah School of Medicine in Salt Lake City.
“SDF is the only test that allows us to look at anything other than bulk semen parameters,” he explained. “It lets us look at that quality of the DNA packaging critical for early embryo development.”
A PROMISING APPROACH
Every man has sperm DNA imperfections, said Mary Samplaski, MD, an assistant professor of urology at the University of Southern California Keck School of Medicine in Los Angeles, but levels are higher among sub-fertile and infertile men. High SDF, loosely defined as more than 30%, correlates with all reproductive outcomes, including lower success rates in natural pregnancy, intrauterine insemination, and in vitro fertilization (IVF), as well as higher miscarriage occurrences.
Several factors lead to this damage, said Ashok Agarwal, PhD, director of the Cleveland Clinic Clinical Andrology Lab and Sperm Bank. Oxidative stress, abortive apoptosis, and environmental factors, such as ultraviolet light and cellphone radiation, all can negatively impact DNA. Lifestyle factors, including obesity, diabetes, and sedentary occupations, also pose damage to sperm. Additionally, varicoceles—enlarged testicular veins that cause overheating and injure sperm—are present in approximately 40% of men with infertility.
With SDF test results in hand, reproductive specialists can recommend necessary lifestyle changes and guide patients toward the fertility treatment options that offer the best opportunities for success, he said.
“Rather than having a patient undergo and play Russian roulette with expensive technologies like IVF or [intracytoplasmic sperm injection] that can cost $10,000 to $15,000 per attempt with less than a 30% success rate,” he said, “we can avoid pricey and unnecessary treatments for couples with male factor infertility having repeated IVF failure or recurrent pregnancy loss by using SDF outcomes to reduce the DNA damage before undergoing assisted reproduction treatment.”
Samplaski agreed, noting that SDF offers vital information, pointing couples struggling with infertility down the right path as early as possible during their best reproductive years. That includes, she added, suggesting men take an antioxidant to counteract any oxidative stress damage.
SDF also supports clinical procedures that reduce DNA damage, according to Sheena Lewis, PhD, FRSB, emeritus professor at Queen’s University Belfast School of Medicine, Dentistry, and Biomedical Sciences in Northern Ireland. Removing sperm via testicular biopsy, before it picks up oxidative stress damage traveling along the epididymis (which she called the “war zone”), can yield healthier sperm for fertility procedures. Varicocele repair also offers similar improvement, she said. In fact, research shows men can experience a 3.4% damage reduction within 3 months via SDF retesting (Int Urol Nephrol 2015;47:1471–7).
WHAT IS HOLDING SDF BACK?
Despite providing a greater degree of actionable information, SDF still lags in the quest for widespread implementation. To a large degree, ease of access is a stumbling block, according to Amin S. Herati, MD, assistant -professor of urology and director of male infertility at the Brady Urological Institute at the Johns Hopkins School of Medicine in Baltimore. “For these tests, access for patients and providers is a big issue,” he said. “Only select labs offer it. Not everyone does it.”
Agarwal agreed, but he did not recommend every lab offer these tests as an in-house service. Instead, he said, they should identify a specialty lab, such as his own, already equipped with properly trained personnel, lab space, and equipment to process SDF tests to meet their needs.
Consistency and translatability have also been obstacles. Not only does each SDF test assess DNA fragmentation differently, each also has its own cut point to diagnose sperm quality levels. To make tests more easily accepted, procedures and results reporting must be standardized, Hotaling emphasized.
“There’s a lot of variability in how the test is run,” he said. “It’s not the same from one place to another, so it’s hard to compare results between labs.” Samplaski concurred, saying the level of existing differentiation makes reproductive specialists reticent to order SDF tests more frequently.
As with all other tests, though, until SDF methods are analyzed in larger clinical trials and submit reliable, reproducible results, providers will remain hesitant about suggesting the test for a wider patient population. Even as an initial SDF advocate, Herati acknowledged that the data to support the methods’ robust use has not appeared so far. However, these functional tests provide actionable information for a certain group of men struggling with infertility.
“I still use sperm DNA fragmentation, but its main role in my mind is for someone with normal semen parameters whose partner might have recurrent pregnancy loss,” Herati said. “We can decide where the sperm should come from for fertility services and what we can do to optimize that choice. That’s really where the utility of DNA fragmentation lies.”
Still, Agarwal said, SDF is one of the most important male fertility advancements in the last 60 years. Although it’s still in the early adoption phase, it offers hope for a successful pregnancy in cases when male-factor infertility was previously undiagnosed.
“Infertility is complicated, and sperm DNA fragmentation is an important part of testing in male patients, but it isn’t a silver bullet,” he emphasized. “It’s one way to examine, look for, and find hidden problems that aren’t told by semen analysis, and that’s a big thing. But, it’s not for every patient who has a problem with infertility.”
Sheena Lewis is the founder of Examen, producer of the SpermCOMET test and managing director of Lewis Fertility Testing, Ltd., a spin-out company of Queen’s University Belfast.
Whitney J. Palmer is a freelance journalist in Holly Springs, North Carolina. Email: whitneyljhowell@gmail.com
At the 71st AACC Annual Scientific Meeting & Clinical Lab Expo, scientific sessions cover a wide array of dynamic areas of clinical laboratory medicine. For sessions related to this and other cutting-edge laboratory methods visit https://2019aacc.org/conference-program.
Latest AACC 2019 News
- Instrumentation Laboratory Presents New IVD Testing System
- Quidel Welcomes Newest Member of Triage Family
- ERBA Mannheim Unveils Next-Generation Automation
- Roche Demonstrates How Health Networks Are Driving Change in Labs and Beyond
- BioMérieux Spotlights Diagnostic Solutions in Use of Antibiotics
- Thermo Shows New Clinical Innovations
- Randox Launches New Innovations
- Streck Introduces Three New Antibiotic Resistance Detection Kits
- EKF Diagnostics Highlights Assay for Diabetes Patient Monitoring
- Sysmex America Exhibits New Products, Automation and Quality Solutions
- BBI Solutions Showcases Mobile Solutions Capabilities at AACC 2019
- MedTest Dx Releases New Product Line for Drugs of Abuse Testing
- Mesa Biotech Launches Molecular Test System at AACC 2019
- Ortho Clinical Diagnostics Highlights Groundbreaking Lab Technology
- Abbott Diagnostics Exhibits POC Diagnostics Solutions at AACC
- Beckman Coulter Demonstrates Latest Innovations in Lab Medicine
Channels
Clinical Chemistry
view channel
New PSA-Based Prognostic Model Improves Prostate Cancer Risk Assessment
Prostate cancer is the second-leading cause of cancer death among American men, and about one in eight will be diagnosed in their lifetime. Screening relies on blood levels of prostate-specific antigen... Read more
Extracellular Vesicles Linked to Heart Failure Risk in CKD Patients
Chronic kidney disease (CKD) affects more than 1 in 7 Americans and is strongly associated with cardiovascular complications, which account for more than half of deaths among people with CKD.... Read moreMolecular Diagnostics
view channel
Diagnostic Device Predicts Treatment Response for Brain Tumors Via Blood Test
Glioblastoma is one of the deadliest forms of brain cancer, largely because doctors have no reliable way to determine whether treatments are working in real time. Assessing therapeutic response currently... Read more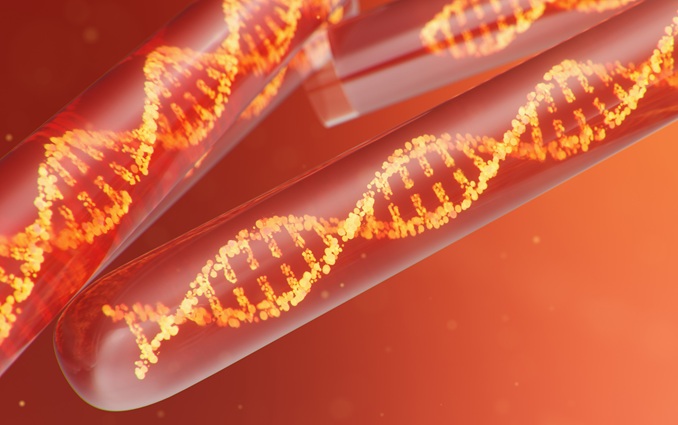
Blood Test Detects Early-Stage Cancers by Measuring Epigenetic Instability
Early-stage cancers are notoriously difficult to detect because molecular changes are subtle and often missed by existing screening tools. Many liquid biopsies rely on measuring absolute DNA methylation... Read more
“Lab-On-A-Disc” Device Paves Way for More Automated Liquid Biopsies
Extracellular vesicles (EVs) are tiny particles released by cells into the bloodstream that carry molecular information about a cell’s condition, including whether it is cancerous. However, EVs are highly... Read more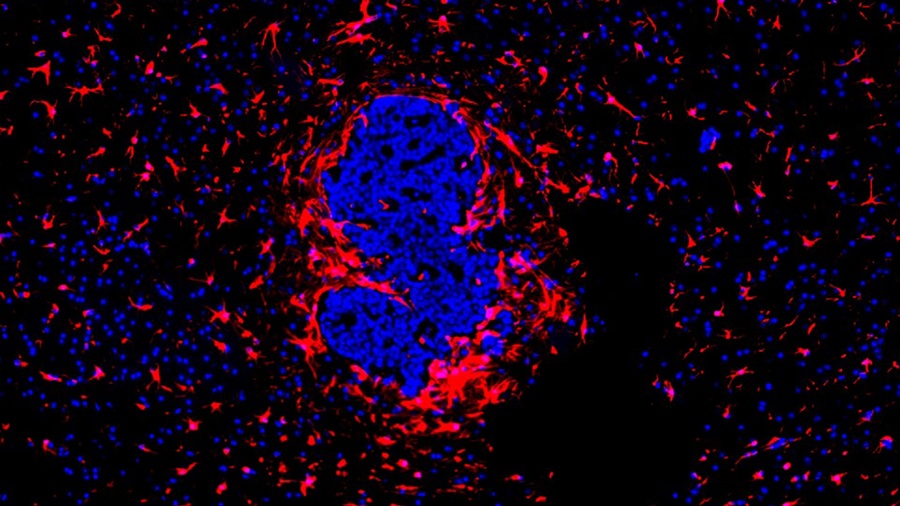
Blood Test Identifies Inflammatory Breast Cancer Patients at Increased Risk of Brain Metastasis
Brain metastasis is a frequent and devastating complication in patients with inflammatory breast cancer, an aggressive subtype with limited treatment options. Despite its high incidence, the biological... Read moreHematology
view channel
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read more
Fast and Easy Test Could Revolutionize Blood Transfusions
Blood transfusions are a cornerstone of modern medicine, yet red blood cells can deteriorate quietly while sitting in cold storage for weeks. Although blood units have a fixed expiration date, cells from... Read more
Automated Hemostasis System Helps Labs of All Sizes Optimize Workflow
High-volume hemostasis sections must sustain rapid turnaround while managing reruns and reflex testing. Manual tube handling and preanalytical checks can strain staff time and increase opportunities for error.... Read more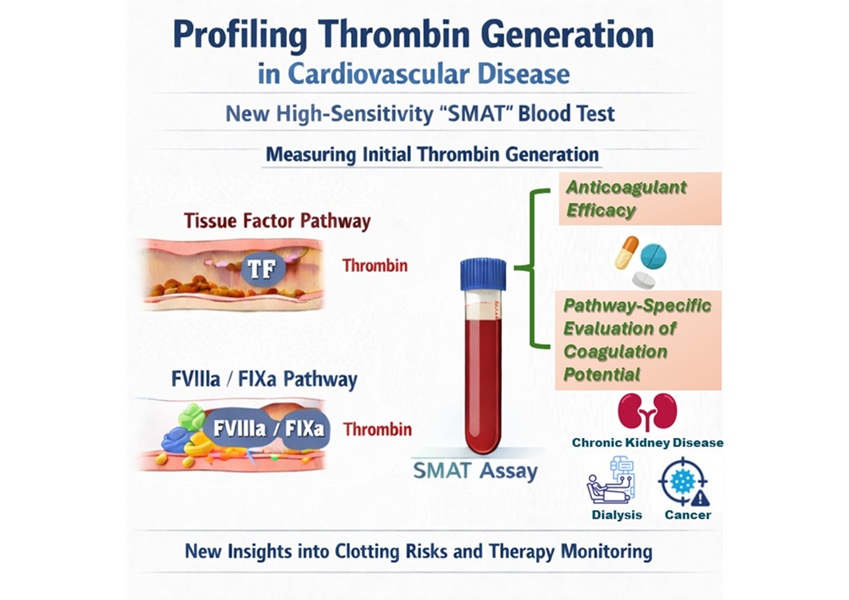
High-Sensitivity Blood Test Improves Assessment of Clotting Risk in Heart Disease Patients
Blood clotting is essential for preventing bleeding, but even small imbalances can lead to serious conditions such as thrombosis or dangerous hemorrhage. In cardiovascular disease, clinicians often struggle... Read moreImmunology
view channelBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read more
Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
Immunotherapy has transformed cancer treatment, but only a small proportion of patients experience lasting benefit, with response rates often remaining between 10% and 20%. Clinicians currently lack reliable... Read moreMicrobiology
view channel
Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
Alzheimer’s disease affects approximately 6.7 million people in the United States and nearly 50 million worldwide, yet early cognitive decline remains difficult to characterize. Increasing evidence suggests... Read moreAI-Powered Platform Enables Rapid Detection of Drug-Resistant C. Auris Pathogens
Infections caused by the pathogenic yeast Candida auris pose a significant threat to hospitalized patients, particularly those with weakened immune systems or those who have invasive medical devices.... Read morePathology
view channel
Engineered Yeast Cells Enable Rapid Testing of Cancer Immunotherapy
Developing new cancer immunotherapies is a slow, costly, and high-risk process, particularly for CAR T cell treatments that must precisely recognize cancer-specific antigens. Small differences in tumor... Read more
First-Of-Its-Kind Test Identifies Autism Risk at Birth
Autism spectrum disorder is treatable, and extensive research shows that early intervention can significantly improve cognitive, social, and behavioral outcomes. Yet in the United States, the average age... Read moreTechnology
view channel
Robotic Technology Unveiled for Automated Diagnostic Blood Draws
Routine diagnostic blood collection is a high‑volume task that can strain staffing and introduce human‑dependent variability, with downstream implications for sample quality and patient experience.... Read more
ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
Clinical laboratories generate billions of test results each year, creating a treasure trove of data with the potential to support more personalized testing, improve operational efficiency, and enhance patient care.... Read moreAptamer Biosensor Technology to Transform Virus Detection
Rapid and reliable virus detection is essential for controlling outbreaks, from seasonal influenza to global pandemics such as COVID-19. Conventional diagnostic methods, including cell culture, antigen... Read more
AI Models Could Predict Pre-Eclampsia and Anemia Earlier Using Routine Blood Tests
Pre-eclampsia and anemia are major contributors to maternal and child mortality worldwide, together accounting for more than half a million deaths each year and leaving millions with long-term health complications.... Read moreIndustry
view channelNew Collaboration Brings Automated Mass Spectrometry to Routine Laboratory Testing
Mass spectrometry is a powerful analytical technique that identifies and quantifies molecules based on their mass and electrical charge. Its high selectivity, sensitivity, and accuracy make it indispensable... Read more
AI-Powered Cervical Cancer Test Set for Major Rollout in Latin America
Noul Co., a Korean company specializing in AI-based blood and cancer diagnostics, announced it will supply its intelligence (AI)-based miLab CER cervical cancer diagnostic solution to Mexico under a multi‑year... Read more
Diasorin and Fisher Scientific Enter into US Distribution Agreement for Molecular POC Platform
Diasorin (Saluggia, Italy) has entered into an exclusive distribution agreement with Fisher Scientific, part of Thermo Fisher Scientific (Waltham, MA, USA), for the LIAISON NES molecular point-of-care... Read more