Serum Magnesium Levels Associated with CAP Mortality
|
By LabMedica International staff writers Posted on 07 Jan 2019 |

Image: The Dimension EXL 200 integrated chemistry system (Photo courtesy of Siemens Healthcare).
Community acquired pneumonia (CAP) is a common illness affecting hundreds of millions worldwide, with increasing hospital admissions throughout the years mainly due to the aging population. It is a major cause of mortality and morbidity in all age groups, especially the elderly.
Magnesium deficiency has been associated with a number of clinical manifestations such as arrhythmias, cardiac insufficiency, sudden death, muscle weakness, bronchospasm, tetany, seizures, as well as hypokalemia, hypocalcaemia, hyponatremia, and hypophosphatemia. Hypermagnesemia may cause severe symptomatic hypotension, bradycardia and ECG changes like wide QRS.
Scientists at the Rambam Health Care Campus (Haifa, Israel) and their colleagues retrospectively reviewed between January 1, 2010, and December 31, 2016, the data of 4,708 patients diagnosed with CAP at discharge; 3,851 patients had magnesium levels within 48 hours, and 55% were males and the median age was 72 years old. Participants were analyzed retrospectively in order to identify the risk factors for a primary endpoint of 30-day mortality.
The Charlson’s comorbidity score was calculated based on data collected; laboratory values (first values within 48 hours): Hemoglobin (Hb), White blood cell count (WBC), red blood cell distribution width (RDW), pH, partial pressure of carbon dioxide (pCO2), serum glucose, serum creatinine, sodium, calcium, phosphorus, magnesium, blood urea nitrogen (BUN), and serum albumin. Hematological values were measured using the Advia 120 Hematology Analyzer. Serum glucose, serum creatinine, sodium, calcium, phosphorus, magnesium, blood urea nitrogen (BUN), and serum albumin were measured on admission using Siemens’ Dimension Integrated Chemistry System; PH, bicarbonate, partial pressure of CO2 and lactate were measured using GEM premier 3500.
The team reported that blood urea nitrogen (BUN) > 20 mg/dL, hypoalbuminemia, and abnormal levels of magnesium were all associated with increased risk of 30-day mortality. Normal magnesium levels were associated with the lowest mortality rate (14.7%). Notably, within the normal levels, high normal magnesium levels (2.0 to 2.4 mg/dL) were correlated with higher mortality rates (30.3%) as compared to levels that ranged between 1.35 to 2 mg/dL (12.9%). Hypomagnesemia and hypermagnesemia were both associated with excess of 30-day mortality, 18.4 and 50%, respectively. Normal levels of magnesium levels in their laboratory vary between 1.35 and 2.4 mg/dL.
The authors concluded that hypomagnesemia and hypermagnesemia on admission were associated with an increased rate of 30-day mortality among adult patients hospitalized with CAP. Interestingly, magnesium levels within the upper normal limits were associated with higher mortality. The study was published on December 27, 2018, in the journal BMC Infectious Diseases.
Related Links:
Rambam Health Care Campus
Magnesium deficiency has been associated with a number of clinical manifestations such as arrhythmias, cardiac insufficiency, sudden death, muscle weakness, bronchospasm, tetany, seizures, as well as hypokalemia, hypocalcaemia, hyponatremia, and hypophosphatemia. Hypermagnesemia may cause severe symptomatic hypotension, bradycardia and ECG changes like wide QRS.
Scientists at the Rambam Health Care Campus (Haifa, Israel) and their colleagues retrospectively reviewed between January 1, 2010, and December 31, 2016, the data of 4,708 patients diagnosed with CAP at discharge; 3,851 patients had magnesium levels within 48 hours, and 55% were males and the median age was 72 years old. Participants were analyzed retrospectively in order to identify the risk factors for a primary endpoint of 30-day mortality.
The Charlson’s comorbidity score was calculated based on data collected; laboratory values (first values within 48 hours): Hemoglobin (Hb), White blood cell count (WBC), red blood cell distribution width (RDW), pH, partial pressure of carbon dioxide (pCO2), serum glucose, serum creatinine, sodium, calcium, phosphorus, magnesium, blood urea nitrogen (BUN), and serum albumin. Hematological values were measured using the Advia 120 Hematology Analyzer. Serum glucose, serum creatinine, sodium, calcium, phosphorus, magnesium, blood urea nitrogen (BUN), and serum albumin were measured on admission using Siemens’ Dimension Integrated Chemistry System; PH, bicarbonate, partial pressure of CO2 and lactate were measured using GEM premier 3500.
The team reported that blood urea nitrogen (BUN) > 20 mg/dL, hypoalbuminemia, and abnormal levels of magnesium were all associated with increased risk of 30-day mortality. Normal magnesium levels were associated with the lowest mortality rate (14.7%). Notably, within the normal levels, high normal magnesium levels (2.0 to 2.4 mg/dL) were correlated with higher mortality rates (30.3%) as compared to levels that ranged between 1.35 to 2 mg/dL (12.9%). Hypomagnesemia and hypermagnesemia were both associated with excess of 30-day mortality, 18.4 and 50%, respectively. Normal levels of magnesium levels in their laboratory vary between 1.35 and 2.4 mg/dL.
The authors concluded that hypomagnesemia and hypermagnesemia on admission were associated with an increased rate of 30-day mortality among adult patients hospitalized with CAP. Interestingly, magnesium levels within the upper normal limits were associated with higher mortality. The study was published on December 27, 2018, in the journal BMC Infectious Diseases.
Related Links:
Rambam Health Care Campus
Latest Microbiology News
- Rapid Sequencing Could Transform Tuberculosis Care
- Blood-Based Viral Signature Identified in Crohn’s Disease
- Hidden Gut Viruses Linked to Colorectal Cancer Risk
- Three-Test Panel Launched for Detection of Liver Fluke Infections
- Rapid Test Promises Faster Answers for Drug-Resistant Infections
- CRISPR-Based Technology Neutralizes Antibiotic-Resistant Bacteria
- Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
- AI-Powered Platform Enables Rapid Detection of Drug-Resistant C. Auris Pathogens
- New Test Measures How Effectively Antibiotics Kill Bacteria
- New Antimicrobial Stewardship Standards for TB Care to Optimize Diagnostics
- New UTI Diagnosis Method Delivers Antibiotic Resistance Results 24 Hours Earlier
- Breakthroughs in Microbial Analysis to Enhance Disease Prediction
- Blood-Based Diagnostic Method Could Identify Pediatric LRTIs
- Rapid Diagnostic Test Matches Gold Standard for Sepsis Detection
- Rapid POC Tuberculosis Test Provides Results Within 15 Minutes
- Rapid Assay Identifies Bloodstream Infection Pathogens Directly from Patient Samples
Channels
Molecular Diagnostics
view channel
Blood Test Could Spot Common Post-Surgery Condition Early
Heterotopic ossification (HO), the abnormal formation of bone in soft tissue, is a common complication following hip replacement surgery. The condition affects nearly one in three patients and can lead... Read more
New Blood Test Can Help Predict Testicular Cancer Recurrence
Stage 1 testicular germ cell tumor is typically treated with surgery followed by active surveillance. Although most patients experience strong long-term outcomes, about one in four will see their cancer... Read more
New Test Detects Alzheimer’s by Analyzing Altered Protein Shapes in Blood
Alzheimer’s disease begins developing years before memory loss or other symptoms become visible. Misfolded proteins gradually accumulate in the brain, disrupting normal cellular processes.... Read more
New Diagnostic Markers for Multiple Sclerosis Discovered in Cerebrospinal Fluid
Multiple sclerosis (MS) affects nearly three million people worldwide and can cause symptoms such as numbness, visual disturbances, fatigue, and neurological disability. Diagnosing the disease can be challenging... Read moreHematology
view channel
Rapid Cartridge-Based Test Aims to Expand Access to Hemoglobin Disorder Diagnosis
Sickle cell disease and beta thalassemia are hemoglobin disorders that often require referral to specialized laboratories for definitive diagnosis, delaying results for patients and clinicians.... Read more
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read moreImmunology
view channel
Cancer Mutation ‘Fingerprints’ to Improve Prediction of Immunotherapy Response
Cancer cells accumulate thousands of genetic mutations, but not all mutations affect tumors in the same way. Some make cancer cells more visible to the immune system, while others allow tumors to evade... Read more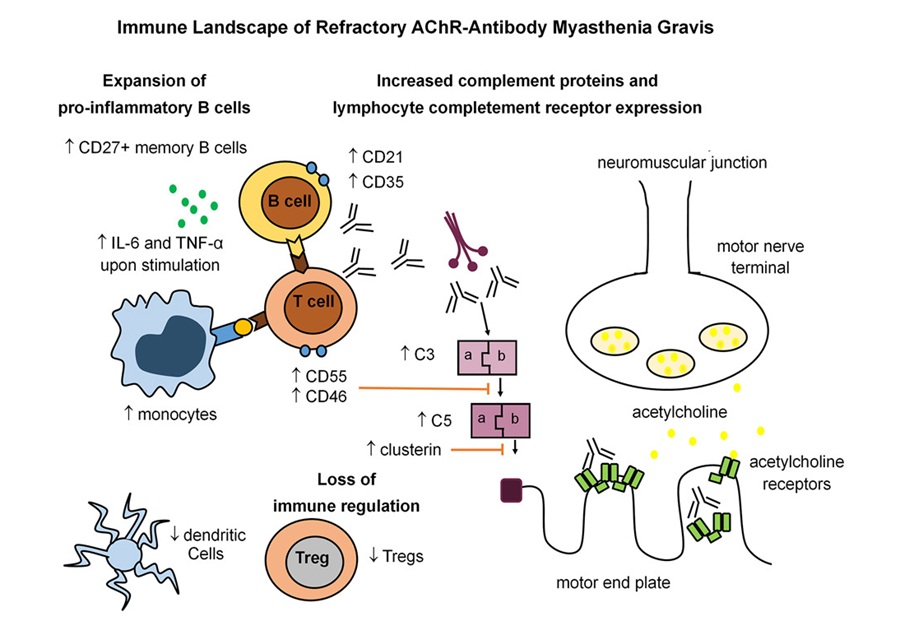
Immune Signature Identified in Treatment-Resistant Myasthenia Gravis
Myasthenia gravis is a rare autoimmune disorder in which immune attack at the neuromuscular junction causes fluctuating weakness that can impair vision, movement, speech, swallowing, and breathing.... Read more
New Biomarker Predicts Chemotherapy Response in Triple-Negative Breast Cancer
Triple-negative breast cancer is an aggressive form of breast cancer in which patients often show widely varying responses to chemotherapy. Predicting who will benefit from treatment remains challenging,... Read moreBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read moreMicrobiology
view channel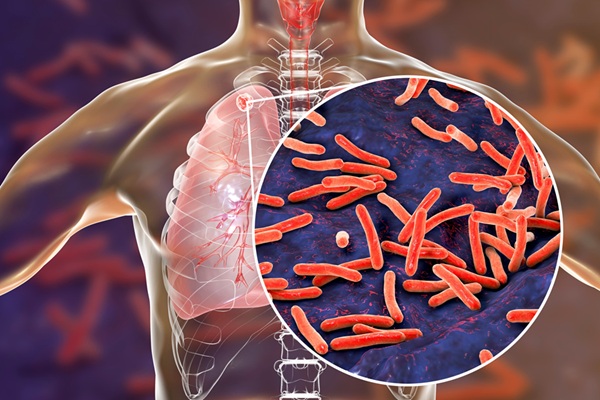
Rapid Sequencing Could Transform Tuberculosis Care
Tuberculosis remains the world’s leading cause of death from a single infectious agent, responsible for more than one million deaths each year. Diagnosing and monitoring the disease can be slow because... Read more
Blood-Based Viral Signature Identified in Crohn’s Disease
Crohn’s disease is a chronic inflammatory intestinal disorder affecting approximately 0.4% of the European population, with symptoms and progression that vary widely. Although viral components of the microbiome... Read morePathology
view channel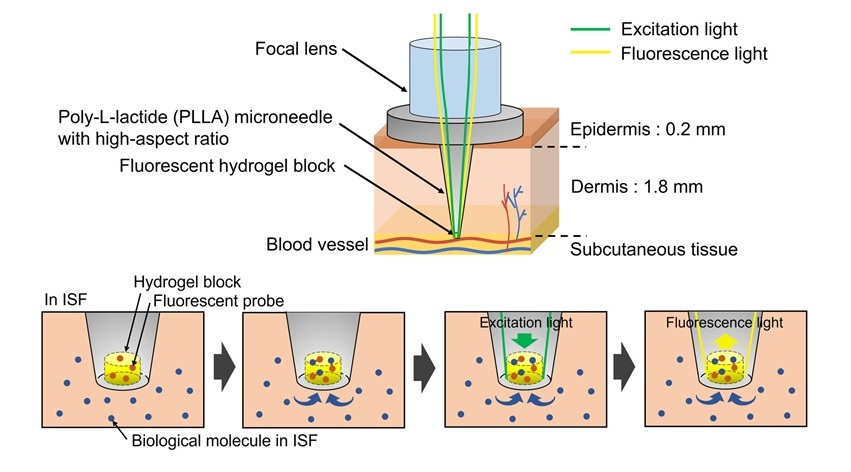
World’s First Optical Microneedle Device to Enable Blood-Sampling-Free Clinical Testing
Blood sampling is one of the most common clinical procedures, but it can be difficult or uncomfortable for many patients, especially older adults or individuals with certain medical conditions.... Read more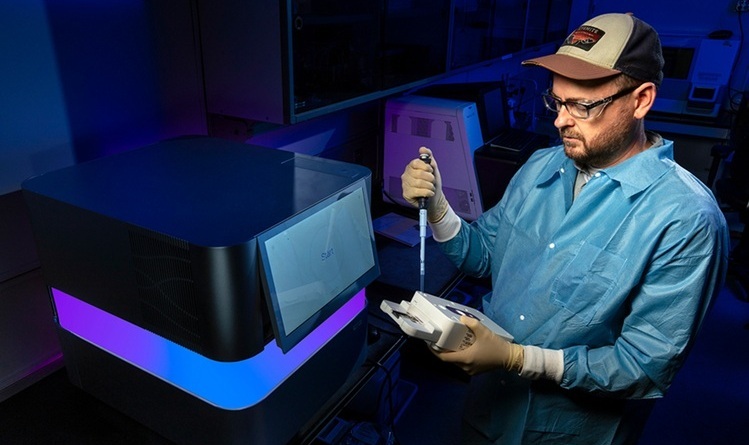
Pathogen-Agnostic Testing Reveals Hidden Respiratory Threats in Negative Samples
Polymerase Chain Reaction (PCR) testing became widely recognized during the COVID-19 pandemic as a powerful method for detecting viruses such as SARS-CoV-2. PCR belongs to a group of diagnostic methods... Read moreTechnology
view channel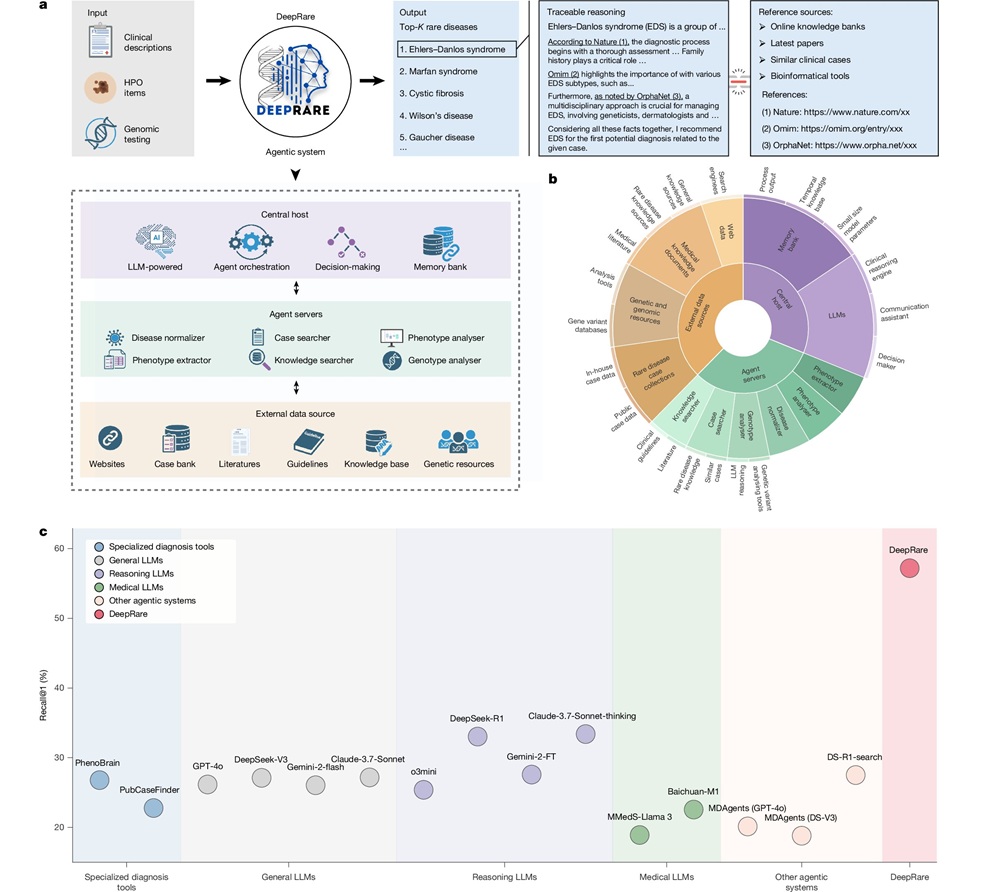
AI Model Outperforms Clinicians in Rare Disease Detection
Rare diseases affect an estimated 300 million people worldwide, yet diagnosis is often protracted and error-prone. Many conditions present with heterogeneous signs that overlap with common disorders, leading... Read more
AI-Driven Diagnostic Demonstrates High Accuracy in Detecting Periprosthetic Joint Infection
Periprosthetic joint infection (PJI) is a rare but serious complication affecting 1% to 2% of primary joint replacement surgeries. The condition occurs when bacteria or fungi infect tissues around an implanted... Read moreIndustry
view channel
Cepheid Joins CDC Initiative to Strengthen U.S. Pandemic Testing Preparednesss
Cepheid (Sunnyvale, CA, USA) has been selected by the U.S. Centers for Disease Control and Prevention (CDC) as one of four national collaborators in a federal initiative to speed rapid diagnostic technologies... Read more
QuidelOrtho Collaborates with Lifotronic to Expand Global Immunoassay Portfolio
QuidelOrtho (San Diego, CA, USA) has entered a long-term strategic supply agreement with Lifotronic Technology (Shenzhen, China) to expand its global immunoassay portfolio and accelerate customer access... Read more


















