Leprosy Neural Impairment Diagnosis Evaluated by Tests
|
By LabMedica International staff writers Posted on 07 Jun 2018 |

Image: The ABI 7300 real-time PCR system (Photo courtesy of Applied Biosystems).
Leprosy is a chronic infectious disease caused by Mycobacterium leprae, an obligate intracellular parasite with a predilection for infecting peripheral nerves and skin. Leprosy is a current and challenging disease, because it still represents a problem for public health in developing countries.
Despite the apparent progress observed in recent years in leprosy control, early identification of cases remains one of the primary objectives of control programs. The long incubation period of leprosy, its insidious symptoms and signs make the diagnosis difficult. The predominance of multibacillary (MB) cases with neural disabilities indicates late diagnosis, reinforcing the ineffective epidemiological control in many countries.
Scientists at the Federal University of Uberlândia (UFU, Uberlândia, Brazil) and their colleagues recruited 175 seropositive and 35 seronegative household contacts from 2014 to 2016, who were subjected to an extensive protocol that included clinical, molecular (peripheral blood quantitative polymerase chain reaction (qPCR), slit-skin smear qPCR, skin biopsy qPCR) and electroneuromyographic evaluations. Enzyme-linked immunosorbent assay (ELISA) was performed on all household contacts. Serum anti-phenolic glycolipid I (PGL-I) IgM antibodies were detected by enzyme-linked immunosorbent assay (ELISA) performed against the purified native PGL-I from the M. leprae cell wall. The quantitative real-time PCR (qPCR) assay targeting M. leprae DNA was performed by targeting the bacillus-specific genomic region (RLEP) in a real-time PCR system.
The investigators found that the positivity of peripheral blood qPCR of seropositive contacts was 40.6% (71/175) whereas only 8.6% (3/35) were qPCR positive in seronegative contacts. For the slit-skin smear, only 4% (7/175) of seropositive contacts presented positive bacilloscopy, whereas the qPCR detected 47.4% (83/175) positivity in this group compared with only 17.1% (6/35) in seronegative contacts. Seropositive contacts presented a 4.04-fold higher chance of neural impairment. The peripheral blood qPCR positivity presented odds of 2.08-fold higher towards neural impairment. Contrarily, the presence of at least one BCG vaccine scar demonstrated 2.44-fold greater protection against neural impairment (OR = 0.41).
The authors concluded that ELISA anti-PGL-I is the most important test in determining the increased chance of neural impairment in asymptomatic leprosy household contacts. The combination of the two assays (ELISA anti-PGL-I and peripheral blood qPCR) and the presence of BCG scar may identify individuals with higher chances of developing leprosy neuropathy corroborating with the early diagnosis and treatment. The study was published on May 21, 2018, in the journal Public Library of Science Neglected Tropical Diseases.
Related Links:
Federal University of Uberlândia
Despite the apparent progress observed in recent years in leprosy control, early identification of cases remains one of the primary objectives of control programs. The long incubation period of leprosy, its insidious symptoms and signs make the diagnosis difficult. The predominance of multibacillary (MB) cases with neural disabilities indicates late diagnosis, reinforcing the ineffective epidemiological control in many countries.
Scientists at the Federal University of Uberlândia (UFU, Uberlândia, Brazil) and their colleagues recruited 175 seropositive and 35 seronegative household contacts from 2014 to 2016, who were subjected to an extensive protocol that included clinical, molecular (peripheral blood quantitative polymerase chain reaction (qPCR), slit-skin smear qPCR, skin biopsy qPCR) and electroneuromyographic evaluations. Enzyme-linked immunosorbent assay (ELISA) was performed on all household contacts. Serum anti-phenolic glycolipid I (PGL-I) IgM antibodies were detected by enzyme-linked immunosorbent assay (ELISA) performed against the purified native PGL-I from the M. leprae cell wall. The quantitative real-time PCR (qPCR) assay targeting M. leprae DNA was performed by targeting the bacillus-specific genomic region (RLEP) in a real-time PCR system.
The investigators found that the positivity of peripheral blood qPCR of seropositive contacts was 40.6% (71/175) whereas only 8.6% (3/35) were qPCR positive in seronegative contacts. For the slit-skin smear, only 4% (7/175) of seropositive contacts presented positive bacilloscopy, whereas the qPCR detected 47.4% (83/175) positivity in this group compared with only 17.1% (6/35) in seronegative contacts. Seropositive contacts presented a 4.04-fold higher chance of neural impairment. The peripheral blood qPCR positivity presented odds of 2.08-fold higher towards neural impairment. Contrarily, the presence of at least one BCG vaccine scar demonstrated 2.44-fold greater protection against neural impairment (OR = 0.41).
The authors concluded that ELISA anti-PGL-I is the most important test in determining the increased chance of neural impairment in asymptomatic leprosy household contacts. The combination of the two assays (ELISA anti-PGL-I and peripheral blood qPCR) and the presence of BCG scar may identify individuals with higher chances of developing leprosy neuropathy corroborating with the early diagnosis and treatment. The study was published on May 21, 2018, in the journal Public Library of Science Neglected Tropical Diseases.
Related Links:
Federal University of Uberlândia
Latest Immunology News
- Immune Signature Identified in Treatment-Resistant Myasthenia Gravis
- New Biomarker Predicts Chemotherapy Response in Triple-Negative Breast Cancer
- Blood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
- Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
- Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
- Blood Test Could Identify Colon Cancer Patients to Benefit from NSAIDs
- Blood Test Could Detect Adverse Immunotherapy Effects
- Routine Blood Test Can Predict Who Benefits Most from CAR T-Cell Therapy
- New Test Distinguishes Vaccine-Induced False Positives from Active HIV Infection
- Gene Signature Test Predicts Response to Key Breast Cancer Treatment
- Chip Captures Cancer Cells from Blood to Help Select Right Breast Cancer Treatment
- Blood-Based Liquid Biopsy Model Analyzes Immunotherapy Effectiveness
- Signature Genes Predict T-Cell Expansion in Cancer Immunotherapy
- Molecular Microscope Diagnostic System Assesses Lung Transplant Rejection
- Blood Test Tracks Treatment Resistance in High-Grade Serous Ovarian Cancer
- Luminescent Probe Measures Immune Cell Activity in Real Time
Channels
Clinical Chemistry
view channelNew Blood Test Index Offers Earlier Detection of Liver Scarring
Metabolic fatty liver disease is highly prevalent and often silent, yet it can progress to fibrosis, cirrhosis, and liver failure. Current first-line blood test scores frequently return indeterminate results,... Read more
Electronic Nose Smells Early Signs of Ovarian Cancer in Blood
Ovarian cancer is often diagnosed at a late stage because its symptoms are vague and resemble those of more common conditions. Unlike breast cancer, there is currently no reliable screening method, and... Read moreMolecular Diagnostics
view channel
New Test Detects Alzheimer’s by Analyzing Altered Protein Shapes in Blood
Alzheimer’s disease begins developing years before memory loss or other symptoms become visible. Misfolded proteins gradually accumulate in the brain, disrupting normal cellular processes.... Read more
New Diagnostic Markers for Multiple Sclerosis Discovered in Cerebrospinal Fluid
Multiple sclerosis (MS) affects nearly three million people worldwide and can cause symptoms such as numbness, visual disturbances, fatigue, and neurological disability. Diagnosing the disease can be challenging... Read moreHematology
view channel
Rapid Cartridge-Based Test Aims to Expand Access to Hemoglobin Disorder Diagnosis
Sickle cell disease and beta thalassemia are hemoglobin disorders that often require referral to specialized laboratories for definitive diagnosis, delaying results for patients and clinicians.... Read more
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read moreImmunology
view channel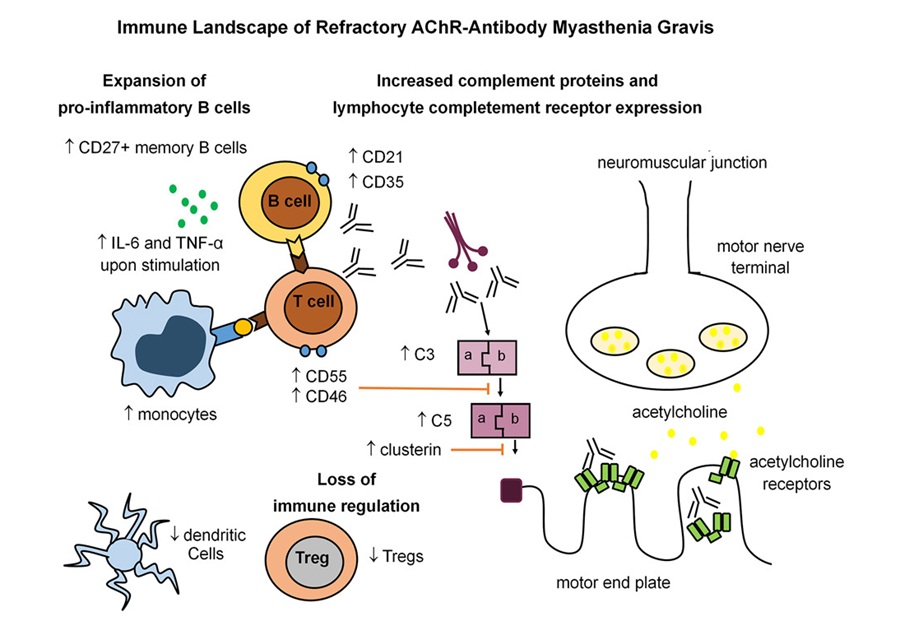
Immune Signature Identified in Treatment-Resistant Myasthenia Gravis
Myasthenia gravis is a rare autoimmune disorder in which immune attack at the neuromuscular junction causes fluctuating weakness that can impair vision, movement, speech, swallowing, and breathing.... Read more
New Biomarker Predicts Chemotherapy Response in Triple-Negative Breast Cancer
Triple-negative breast cancer is an aggressive form of breast cancer in which patients often show widely varying responses to chemotherapy. Predicting who will benefit from treatment remains challenging,... Read moreBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read morePathology
view channel
Molecular Imaging to Reduce Need for Melanoma Biopsies
Melanoma is the deadliest form of skin cancer and accounts for the vast majority of skin cancer-related deaths. Because early melanomas can closely resemble benign moles, clinicians often rely on visual... Read more
Urine Specimen Collection System Improves Diagnostic Accuracy and Efficiency
Urine testing is a critical, non-invasive diagnostic tool used to detect conditions such as pregnancy, urinary tract infections, metabolic disorders, cancer, and kidney disease. However, contaminated or... Read moreTechnology
view channel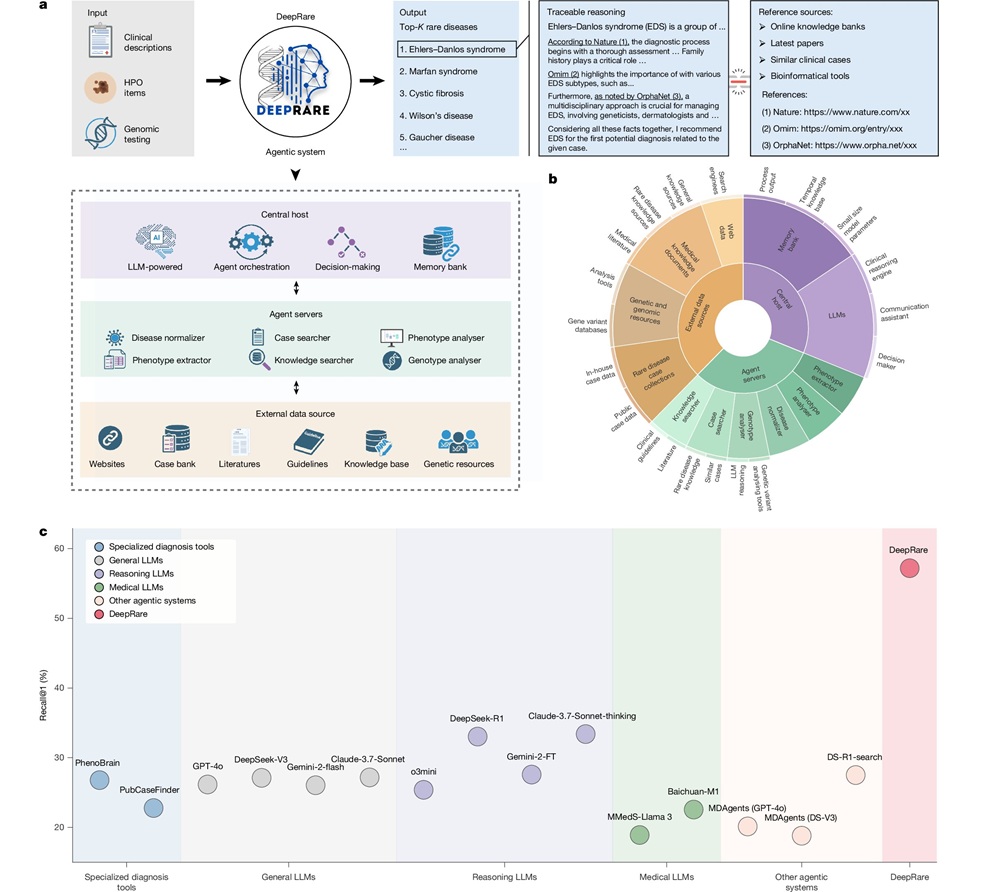
AI Model Outperforms Clinicians in Rare Disease Detection
Rare diseases affect an estimated 300 million people worldwide, yet diagnosis is often protracted and error-prone. Many conditions present with heterogeneous signs that overlap with common disorders, leading... Read more
AI-Driven Diagnostic Demonstrates High Accuracy in Detecting Periprosthetic Joint Infection
Periprosthetic joint infection (PJI) is a rare but serious complication affecting 1% to 2% of primary joint replacement surgeries. The condition occurs when bacteria or fungi infect tissues around an implanted... Read moreIndustry
view channel
Cepheid Joins CDC Initiative to Strengthen U.S. Pandemic Testing Preparednesss
Cepheid (Sunnyvale, CA, USA) has been selected by the U.S. Centers for Disease Control and Prevention (CDC) as one of four national collaborators in a federal initiative to speed rapid diagnostic technologies... Read more
QuidelOrtho Collaborates with Lifotronic to Expand Global Immunoassay Portfolio
QuidelOrtho (San Diego, CA, USA) has entered a long-term strategic supply agreement with Lifotronic Technology (Shenzhen, China) to expand its global immunoassay portfolio and accelerate customer access... Read more