Blood Type Linked to Risk of COVID-19 Infection Severity
|
By LabMedica International staff writers Posted on 04 Jan 2021 |
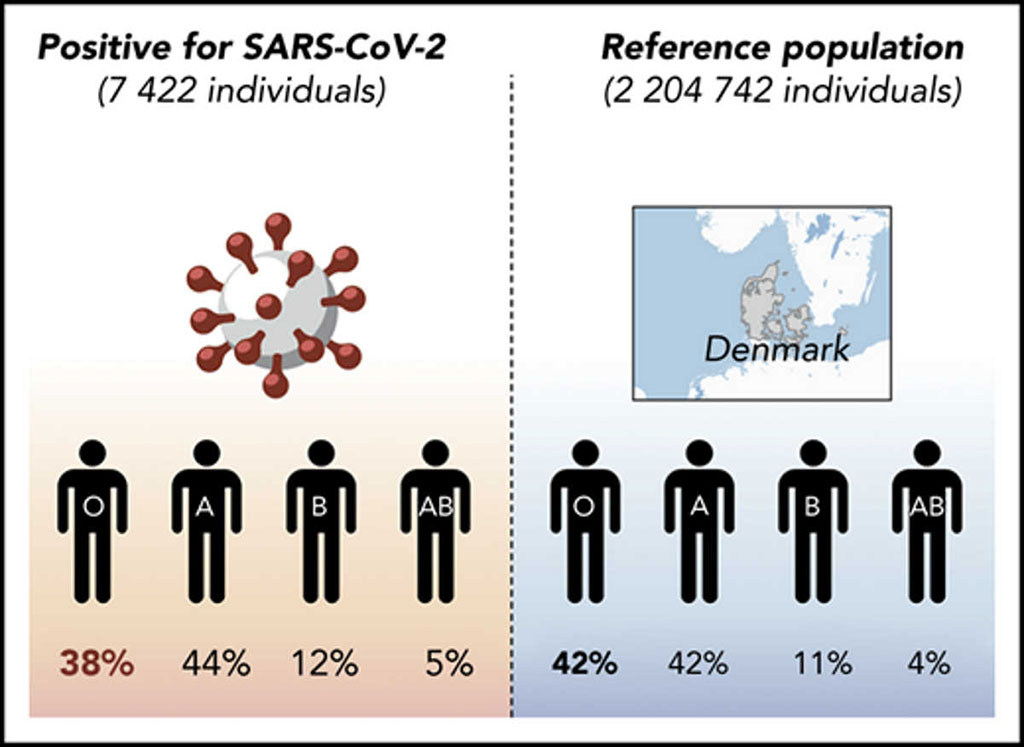
Image: Reduced prevalence of SARS-CoV-2 infection in blood group O individuals reported in Denmark (Photo courtesy of Odense University Hospital).
Identification of risk factors for contracting and developing serious illness following infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is of paramount interest. Development of COVID-19 is associated with age, sex, and comorbidities, such as cardiovascular diseases, although severe disease is not limited to these risk groups.
Blood group A and B glycosyltransferases also affect glycosylation in a large number of cell types, including epithelial cells in the respiratory tract and shed viral particles. A, B, and AB individuals are also at increased risk for thrombosis and cardiovascular diseases, which are important comorbidities among hospitalized COVID-19 patients, possibly mediated by glycosylation of proteins involved in hemostasis.
Clinical Immunologists at the Odense University Hospital (Odense, Denmark) and their colleagues analyzed data in a retrospective cohort study, of over 840,000 individuals in Denmark who underwent testing by polymerase chain reaction for SARS-CoV-2 between February 27 and July 30, 2020. Most of those tested (56%) had available ABO and RhD blood group information. The team also used ABO and RhD data of 2,204,742 individuals not tested for SARS-CoV-2 as a reference. This corresponded to approximately 38% of the entire Danish population.
The scientists reported that of the 473,654 tested individuals who had a known blood group, 7,422 were positive for SARS-CoV-2 and 466,232 were negative. The positive and negative groups had similar proportions of men (32.9% versus 32%) and similar median ages (52 years versus 50 years). Among patients with SARS-CoV-2, considerably fewer (38.4%) had blood type O than other tested blood types. When excluding blood type O, they observed no significant differences among patients with blood types A, B and AB. They also observed no difference in the RhD group between positive cases and the reference population. The investigators reported relative risk (RR) for contracting SARS-CoV-2 of 0.87 for blood type O, 1.09 for blood type A, 1.06 for blood type B and 1.15 for blood type AB.
Torben Barington, MD, a Professor of Medicine and the senior author of the study, said, “ABO blood groups are increasingly recognized to influence susceptibility to certain viruses, including SARS-CoV-1 and norovirus. A, B and AB individuals are also at increased risk for thrombosis and cardiovascular diseases, which are important comorbidities among hospitalized COVID-19 patients, possibly mediated by glycosylation of proteins involved in hemostasis.” The study was originally published on October 14, 2020 in the journal Blood Advances.
Related Links:
Odense University Hospital
Blood group A and B glycosyltransferases also affect glycosylation in a large number of cell types, including epithelial cells in the respiratory tract and shed viral particles. A, B, and AB individuals are also at increased risk for thrombosis and cardiovascular diseases, which are important comorbidities among hospitalized COVID-19 patients, possibly mediated by glycosylation of proteins involved in hemostasis.
Clinical Immunologists at the Odense University Hospital (Odense, Denmark) and their colleagues analyzed data in a retrospective cohort study, of over 840,000 individuals in Denmark who underwent testing by polymerase chain reaction for SARS-CoV-2 between February 27 and July 30, 2020. Most of those tested (56%) had available ABO and RhD blood group information. The team also used ABO and RhD data of 2,204,742 individuals not tested for SARS-CoV-2 as a reference. This corresponded to approximately 38% of the entire Danish population.
The scientists reported that of the 473,654 tested individuals who had a known blood group, 7,422 were positive for SARS-CoV-2 and 466,232 were negative. The positive and negative groups had similar proportions of men (32.9% versus 32%) and similar median ages (52 years versus 50 years). Among patients with SARS-CoV-2, considerably fewer (38.4%) had blood type O than other tested blood types. When excluding blood type O, they observed no significant differences among patients with blood types A, B and AB. They also observed no difference in the RhD group between positive cases and the reference population. The investigators reported relative risk (RR) for contracting SARS-CoV-2 of 0.87 for blood type O, 1.09 for blood type A, 1.06 for blood type B and 1.15 for blood type AB.
Torben Barington, MD, a Professor of Medicine and the senior author of the study, said, “ABO blood groups are increasingly recognized to influence susceptibility to certain viruses, including SARS-CoV-1 and norovirus. A, B and AB individuals are also at increased risk for thrombosis and cardiovascular diseases, which are important comorbidities among hospitalized COVID-19 patients, possibly mediated by glycosylation of proteins involved in hemostasis.” The study was originally published on October 14, 2020 in the journal Blood Advances.
Related Links:
Odense University Hospital
Latest Hematology News
- Next Generation Instrument Screens for Hemoglobin Disorders in Newborns
- First 4-in-1 Nucleic Acid Test for Arbovirus Screening to Reduce Risk of Transfusion-Transmitted Infections
- POC Finger-Prick Blood Test Determines Risk of Neutropenic Sepsis in Patients Undergoing Chemotherapy
- First Affordable and Rapid Test for Beta Thalassemia Demonstrates 99% Diagnostic Accuracy
- Handheld White Blood Cell Tracker to Enable Rapid Testing For Infections
- Smart Palm-size Optofluidic Hematology Analyzer Enables POCT of Patients’ Blood Cells
- Automated Hematology Platform Offers High Throughput Analytical Performance
- New Tool Analyzes Blood Platelets Faster, Easily and Accurately
- First Rapid-Result Hematology Analyzer Reports Measures of Infection and Severity at POC
- Bleeding Risk Diagnostic Test to Reduce Preventable Complications in Hospitals
- True POC Hematology Analyzer with Direct Capillary Sampling Enhances Ease-of-Use and Testing Throughput
- Point of Care CBC Analyzer with Direct Capillary Sampling Enhances Ease-of-Use and Testing Throughput
- Blood Test Could Predict Outcomes in Emergency Department and Hospital Admissions
- Novel Technology Diagnoses Immunothrombosis Using Breath Gas Analysis
- Advanced Hematology System Allows Labs to Process Up To 119 Complete Blood Count Results per Hour
- Unique AI-Based Approach Automates Clinical Analysis of Blood Data
Channels
Clinical Chemistry
view channel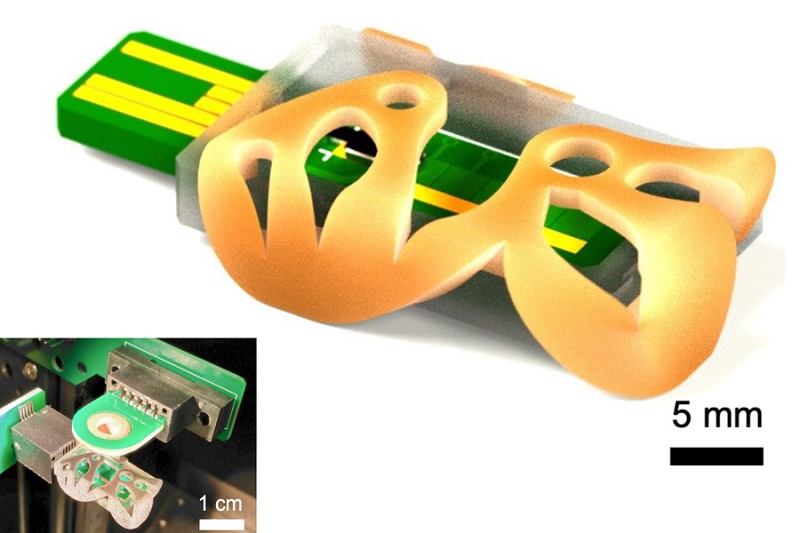
3D Printed Point-Of-Care Mass Spectrometer Outperforms State-Of-The-Art Models
Mass spectrometry is a precise technique for identifying the chemical components of a sample and has significant potential for monitoring chronic illness health states, such as measuring hormone levels... Read more.jpg)
POC Biomedical Test Spins Water Droplet Using Sound Waves for Cancer Detection
Exosomes, tiny cellular bioparticles carrying a specific set of proteins, lipids, and genetic materials, play a crucial role in cell communication and hold promise for non-invasive diagnostics.... Read more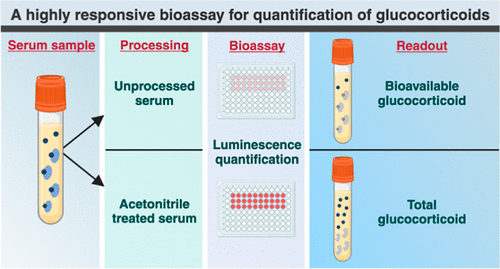
Highly Reliable Cell-Based Assay Enables Accurate Diagnosis of Endocrine Diseases
The conventional methods for measuring free cortisol, the body's stress hormone, from blood or saliva are quite demanding and require sample processing. The most common method, therefore, involves collecting... Read moreMolecular Diagnostics
view channelUltrasound-Aided Blood Testing Detects Cancer Biomarkers from Cells
Ultrasound imaging serves as a noninvasive method to locate and monitor cancerous tumors effectively. However, crucial details about the cancer, such as the specific types of cells and genetic mutations... Read more_1.jpg)
New DNA Origami Technique to Advance Disease Diagnosis
DNA origami is a method used to create nanostructures with exceptional precision, utilizing DNA strands as the foundational building blocks. These structures, however, are inherently fragile and prone... Read more.jpg)
New Respiratory Syndromic Testing Panel Provides Fast and Accurate Results
Respiratory tract infections are a major reason for emergency department visits and hospitalizations. According to the CDC, the U.S. sees up to 41 million influenza cases annually, resulting in several... Read more
New Synthetic Biomarker Technology Differentiates Between Prior Zika and Dengue Infections
Until now, researchers and clinicians have lacked diagnostic tools to easily differentiate between past infections with different flaviviruses—a family of mostly mosquito- and tick-borne viruses that include... Read moreImmunology
view channel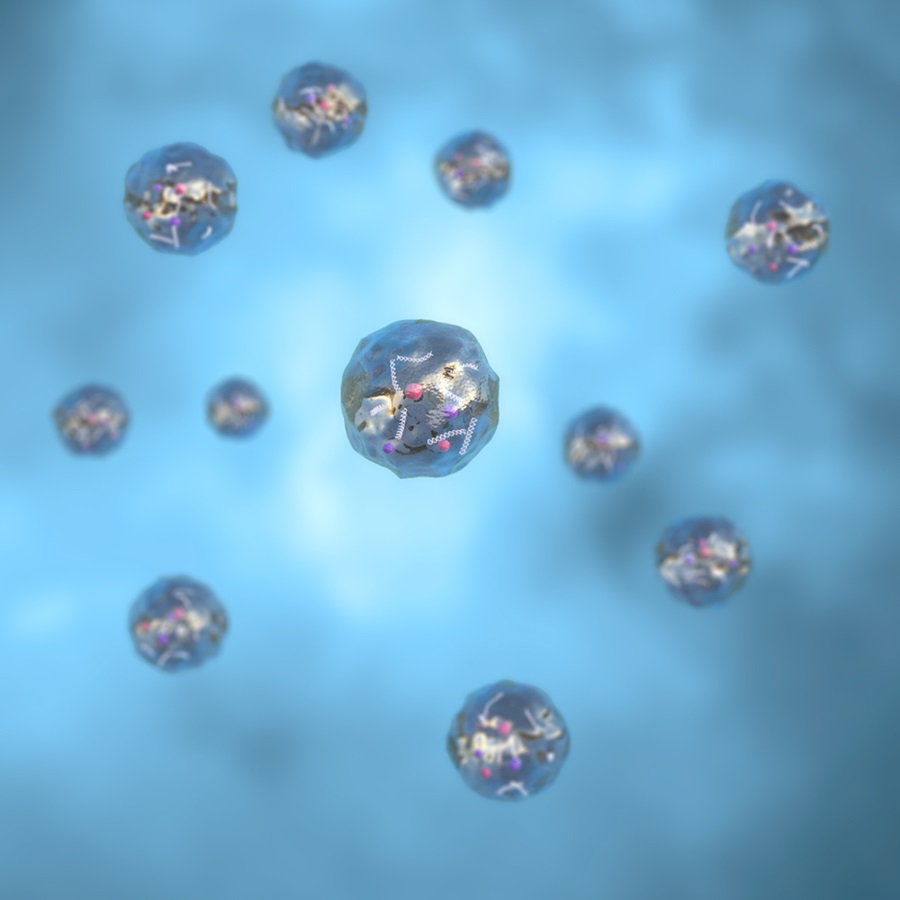
Diagnostic Blood Test for Cellular Rejection after Organ Transplant Could Replace Surgical Biopsies
Transplanted organs constantly face the risk of being rejected by the recipient's immune system which differentiates self from non-self using T cells and B cells. T cells are commonly associated with acute... Read more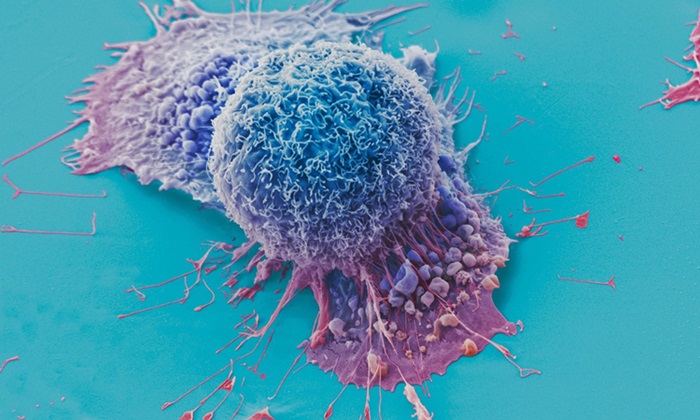
AI Tool Precisely Matches Cancer Drugs to Patients Using Information from Each Tumor Cell
Current strategies for matching cancer patients with specific treatments often depend on bulk sequencing of tumor DNA and RNA, which provides an average profile from all cells within a tumor sample.... Read more
Genetic Testing Combined With Personalized Drug Screening On Tumor Samples to Revolutionize Cancer Treatment
Cancer treatment typically adheres to a standard of care—established, statistically validated regimens that are effective for the majority of patients. However, the disease’s inherent variability means... Read moreMicrobiology
view channel
Integrated Solution Ushers New Era of Automated Tuberculosis Testing
Tuberculosis (TB) is responsible for 1.3 million deaths every year, positioning it as one of the top killers globally due to a single infectious agent. In 2022, around 10.6 million people were diagnosed... Read more
Automated Sepsis Test System Enables Rapid Diagnosis for Patients with Severe Bloodstream Infections
Sepsis affects up to 50 million people globally each year, with bacteraemia, formerly known as blood poisoning, being a major cause. In the United States alone, approximately two million individuals are... Read moreEnhanced Rapid Syndromic Molecular Diagnostic Solution Detects Broad Range of Infectious Diseases
GenMark Diagnostics (Carlsbad, CA, USA), a member of the Roche Group (Basel, Switzerland), has rebranded its ePlex® system as the cobas eplex system. This rebranding under the globally renowned cobas name... Read more
Clinical Decision Support Software a Game-Changer in Antimicrobial Resistance Battle
Antimicrobial resistance (AMR) is a serious global public health concern that claims millions of lives every year. It primarily results from the inappropriate and excessive use of antibiotics, which reduces... Read morePathology
view channelHyperspectral Dark-Field Microscopy Enables Rapid and Accurate Identification of Cancerous Tissues
Breast cancer remains a major cause of cancer-related mortality among women. Breast-conserving surgery (BCS), also known as lumpectomy, is the removal of the cancerous lump and a small margin of surrounding tissue.... Read more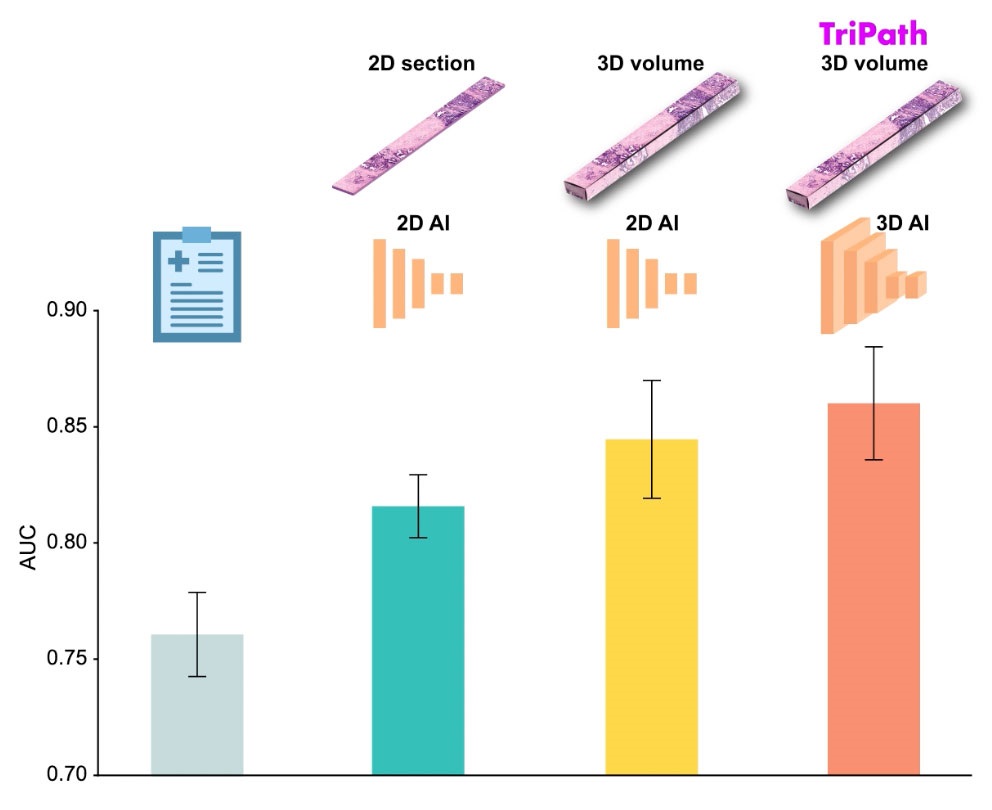
AI Advancements Enable Leap into 3D Pathology
Human tissue is complex, intricate, and naturally three-dimensional. However, the thin two-dimensional tissue slices commonly used by pathologists to diagnose diseases provide only a limited view of the... Read more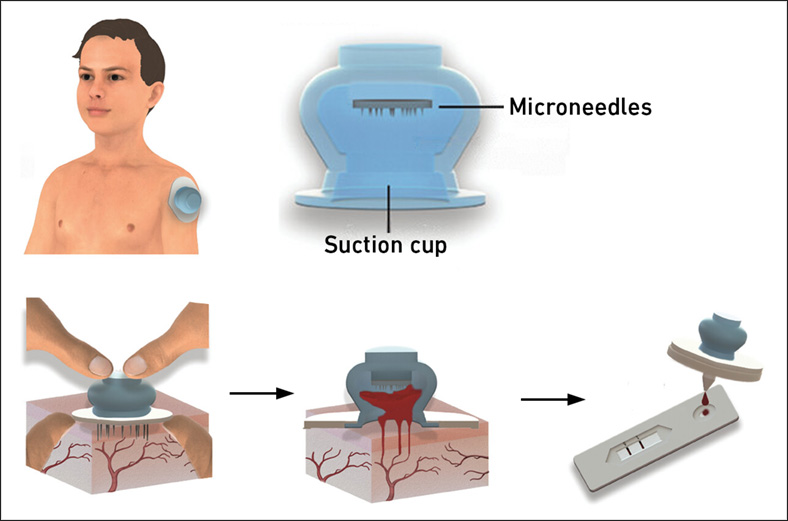
New Blood Test Device Modeled on Leeches to Help Diagnose Malaria
Many individuals have a fear of needles, making the experience of having blood drawn from their arm particularly distressing. An alternative method involves taking blood from the fingertip or earlobe,... Read more
Robotic Blood Drawing Device to Revolutionize Sample Collection for Diagnostic Testing
Blood drawing is performed billions of times each year worldwide, playing a critical role in diagnostic procedures. Despite its importance, clinical laboratories are dealing with significant staff shortages,... Read moreTechnology
view channel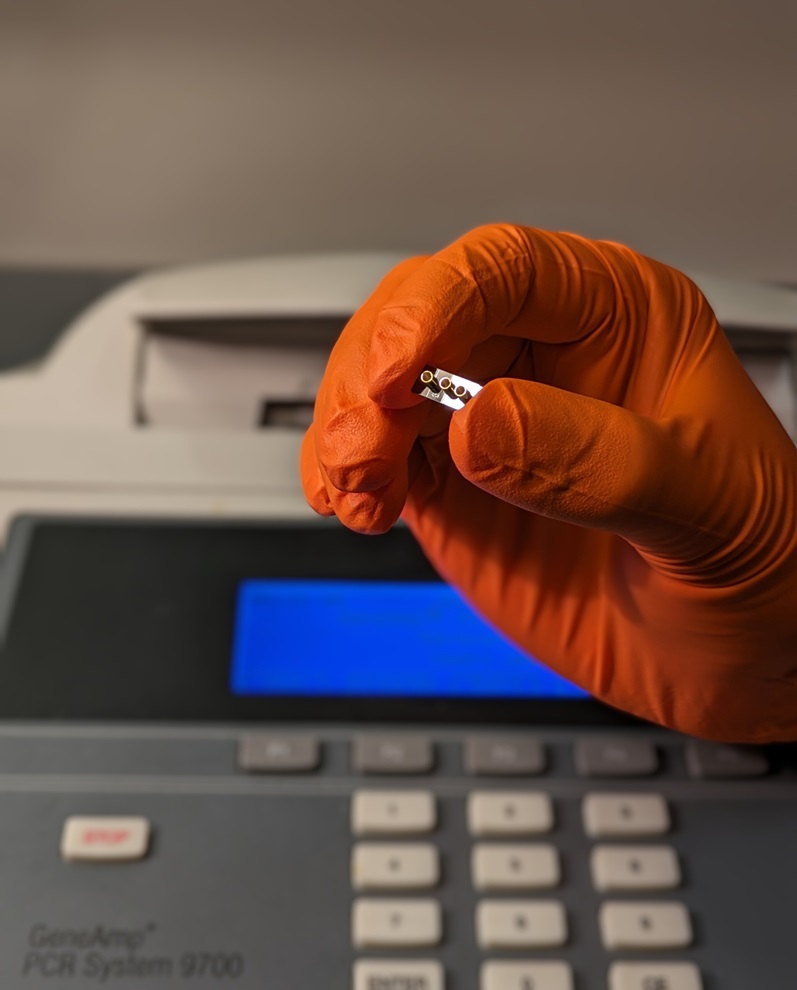
New Diagnostic System Achieves PCR Testing Accuracy
While PCR tests are the gold standard of accuracy for virology testing, they come with limitations such as complexity, the need for skilled lab operators, and longer result times. They also require complex... Read more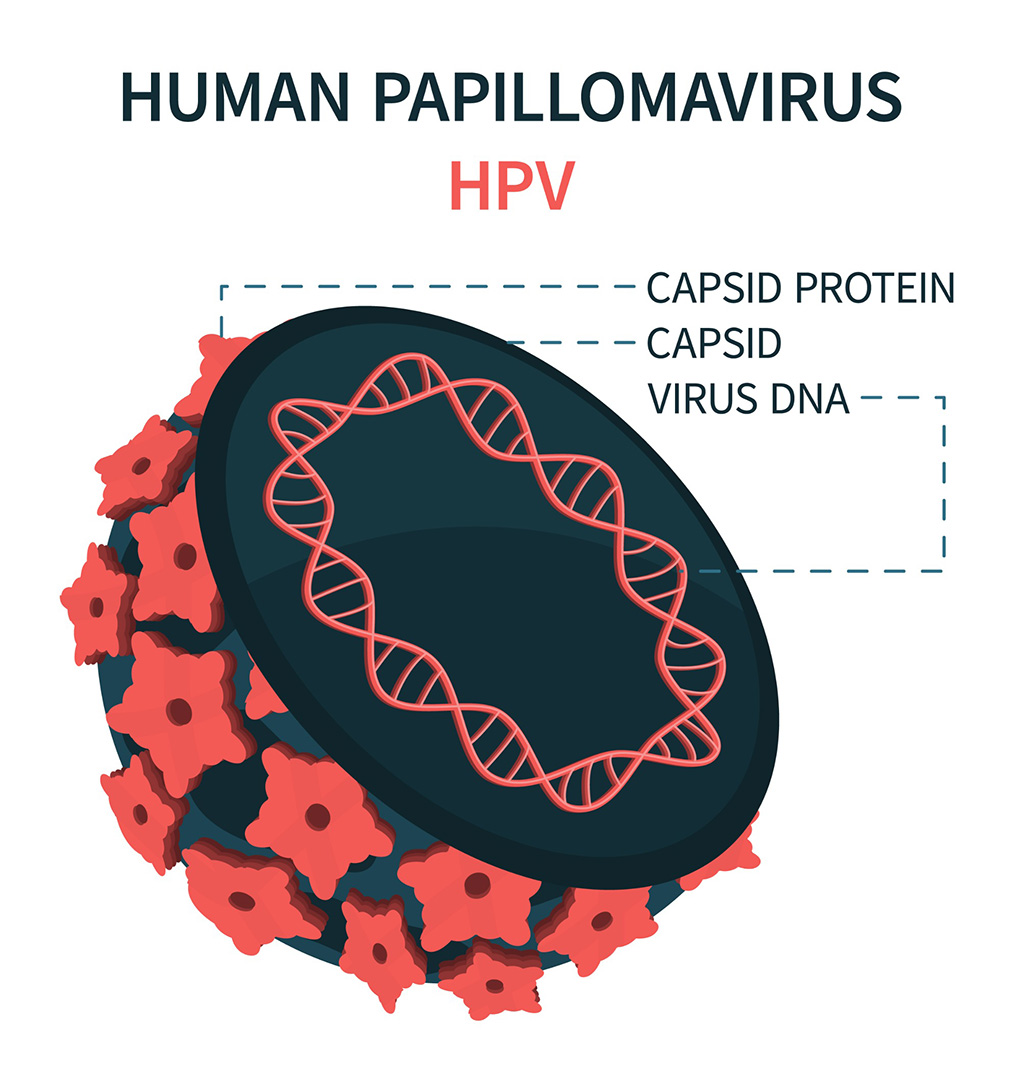
DNA Biosensor Enables Early Diagnosis of Cervical Cancer
Molybdenum disulfide (MoS2), recognized for its potential to form two-dimensional nanosheets like graphene, is a material that's increasingly catching the eye of the scientific community.... Read more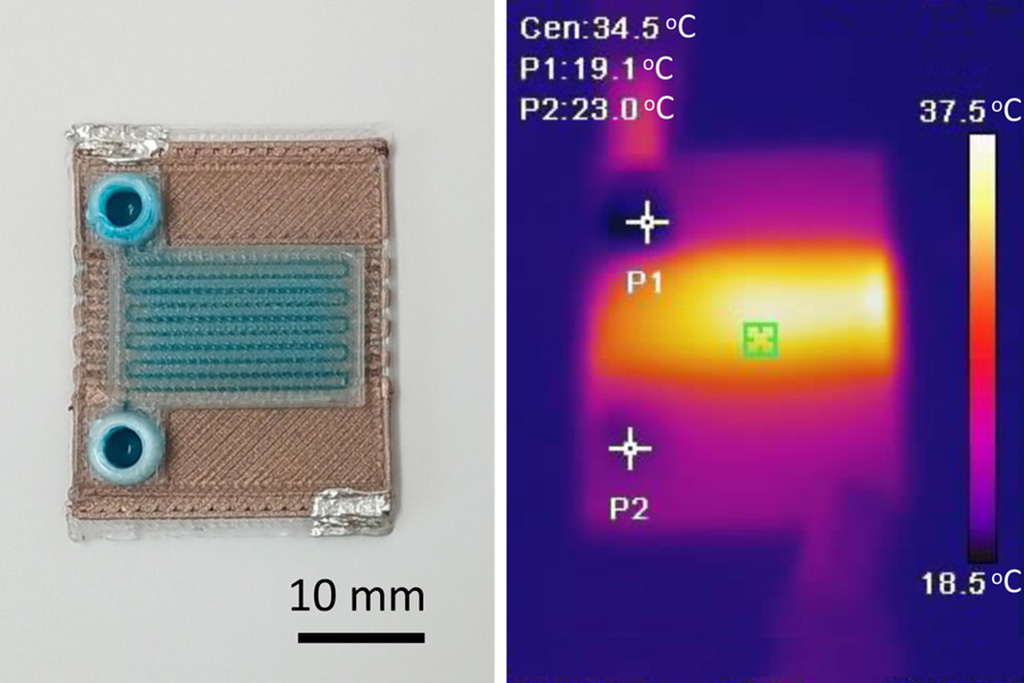
Self-Heating Microfluidic Devices Can Detect Diseases in Tiny Blood or Fluid Samples
Microfluidics, which are miniature devices that control the flow of liquids and facilitate chemical reactions, play a key role in disease detection from small samples of blood or other fluids.... Read more
Breakthrough in Diagnostic Technology Could Make On-The-Spot Testing Widely Accessible
Home testing gained significant importance during the COVID-19 pandemic, yet the availability of rapid tests is limited, and most of them can only drive one liquid across the strip, leading to continued... Read moreIndustry
view channel
Danaher and Johns Hopkins University Collaborate to Improve Neurological Diagnosis
Unlike severe traumatic brain injury (TBI), mild TBI often does not show clear correlations with abnormalities detected through head computed tomography (CT) scans. Consequently, there is a pressing need... Read more
Beckman Coulter and MeMed Expand Host Immune Response Diagnostics Partnership
Beckman Coulter Diagnostics (Brea, CA, USA) and MeMed BV (Haifa, Israel) have expanded their host immune response diagnostics partnership. Beckman Coulter is now an authorized distributor of the MeMed... Read more_1.jpg)