Isoform-Specific Loss Of Dystonin Causes Charcot-Marie-Tooth Disease
|
By LabMedica International staff writers Posted on 20 Aug 2020 |
The HiSeq 2000 Sequencing System (Photo courtesy of Illumina).
Charcot-Marie-Tooth (CMT) disease, also called hereditary motor and sensory neuropathy, is among the most common neurogenetic diseases and is characterized by progressive length-dependent weakness and sensory loss.
CMT is divided into demyelinating (type 1) and axonal (type 2) forms of the disease based on clinical, electrophysiological, histological, and genetic features. Recessively inherited demyelinating neuropathies are called CMT4, whereas recessively inherited axonal neuropathies are called autosomal recessive (AR)-CMT.
Neurologists at the University of Pennsylvania School of Medicine (Philadelphia, PA, USA) and their colleagues applied whole exome sequencing (WES) to analyze the more than 30 million base pairs of DNA that encode the 20,000 proteins in humans. By examining three siblings, two affected and one unaffected, they were able to deduce the genetic basis of mutations that caused the two siblings to be affected.
Genomic DNA was isolated from peripheral blood from all participants. Exome DNA was captured using the SureSelect, Human All Exon5 50 Mb kit (Agilent Technologies, Santa Clara, CA, USA) and sequenced on a HiSeq 2000 (Illumina, San Diego, CA, USA). RNA was isolated from skin using the ZR-Duet DNA/RNA MiniPrep Plus kit (Zymo, Irvine, CA, USA). Complementary DNA (cDNA) was reverse transcribed using SuperScript III First-Strand Synthesis System (Invitrogen, Waltham, MA, USA).
The team identified compound heterozygous mutations in dystonin (DST), which is alternatively spliced to create many plakin family linker proteins (named the bullous pemphigoid antigen 1 [BPAG1] proteins) that function to bridge cytoskeletal filament networks. One mutation (c.250C>T) is predicted to cause a nonsense mutation (p.R84X) that only affects isoform 2 variants, which have an N-terminal transmembrane domain; the other (c.8283+1G>A) mutates a consensus splice donor site and results in a 22 amino acid in-frame deletion in the spectrin repeat domain of all BPAG1a and BPAG1b isoforms.
Steven S. Scherer, MD, PhD, a professor of Neurology and senior author of the study, said, “We are in the era where treatments for genetic diseases are possible. This brother and sister stand to benefit from that approach because we know the gene that is missing, and if we could replace it, that should at least prevent their progression.”
The authors concluded that their findings introduce a novel human phenotype, axonal Charcot-Marie-Tooth, of recessive DST mutations, and provide further evidence that BPAG1 plays an essential role in axonal health. The study was published on July 31, 2020 in the journal Neurology Genetics.
Related Links:
University of Pennsylvania School of Medicine
Agilent Technologies
Illumina
Zymo
Invitrogen - Thermo Fisher
CMT is divided into demyelinating (type 1) and axonal (type 2) forms of the disease based on clinical, electrophysiological, histological, and genetic features. Recessively inherited demyelinating neuropathies are called CMT4, whereas recessively inherited axonal neuropathies are called autosomal recessive (AR)-CMT.
Neurologists at the University of Pennsylvania School of Medicine (Philadelphia, PA, USA) and their colleagues applied whole exome sequencing (WES) to analyze the more than 30 million base pairs of DNA that encode the 20,000 proteins in humans. By examining three siblings, two affected and one unaffected, they were able to deduce the genetic basis of mutations that caused the two siblings to be affected.
Genomic DNA was isolated from peripheral blood from all participants. Exome DNA was captured using the SureSelect, Human All Exon5 50 Mb kit (Agilent Technologies, Santa Clara, CA, USA) and sequenced on a HiSeq 2000 (Illumina, San Diego, CA, USA). RNA was isolated from skin using the ZR-Duet DNA/RNA MiniPrep Plus kit (Zymo, Irvine, CA, USA). Complementary DNA (cDNA) was reverse transcribed using SuperScript III First-Strand Synthesis System (Invitrogen, Waltham, MA, USA).
The team identified compound heterozygous mutations in dystonin (DST), which is alternatively spliced to create many plakin family linker proteins (named the bullous pemphigoid antigen 1 [BPAG1] proteins) that function to bridge cytoskeletal filament networks. One mutation (c.250C>T) is predicted to cause a nonsense mutation (p.R84X) that only affects isoform 2 variants, which have an N-terminal transmembrane domain; the other (c.8283+1G>A) mutates a consensus splice donor site and results in a 22 amino acid in-frame deletion in the spectrin repeat domain of all BPAG1a and BPAG1b isoforms.
Steven S. Scherer, MD, PhD, a professor of Neurology and senior author of the study, said, “We are in the era where treatments for genetic diseases are possible. This brother and sister stand to benefit from that approach because we know the gene that is missing, and if we could replace it, that should at least prevent their progression.”
The authors concluded that their findings introduce a novel human phenotype, axonal Charcot-Marie-Tooth, of recessive DST mutations, and provide further evidence that BPAG1 plays an essential role in axonal health. The study was published on July 31, 2020 in the journal Neurology Genetics.
Related Links:
University of Pennsylvania School of Medicine
Agilent Technologies
Illumina
Zymo
Invitrogen - Thermo Fisher
Latest Molecular Diagnostics News
- New Extraction Kit Enables Consistent, Scalable cfDNA Isolation from Multiple Biofluids
- New CSF Liquid Biopsy Assay Reveals Genomic Insights for CNS Tumors
- AI-Powered Liquid Biopsy Classifies Pediatric Brain Tumors with High Accuracy
- Group A Strep Molecular Test Delivers Definitive Results at POC in 15 Minutes
- Rapid Molecular Test Identifies Sepsis Patients Most Likely to Have Positive Blood Cultures
- Light-Based Sensor Detects Early Molecular Signs of Cancer in Blood
- New Testing Method Predicts Trauma Patient Recovery Days in Advance
- Simple Method Predicts Risk of Brain Tumor Recurrence
- Genetic Test Could Improve Early Detection of Prostate Cancer
- Bone Molecular Maps to Transform Early Osteoarthritis Detection
- POC Testing for Hepatitis B DNA as Effective as Traditional Laboratory Testing
- Fully Automated Immunoassay Test Detects HDV Co‑Infection and Super-Infection
- Abdominal Fluid Testing Can Predict Ovarian Cancer Progression
- POC Test Uses Fingerstick Blood, Serum, Or Plasma Sample to Detect Typhoid Fever
- Rapid Testing Panel Simultaneously Detects 15 Drugs of Abuse in Urine Within 21 Minutes
- New Test Detects Breast Reconstruction-Related Infections Before Symptoms Appear
Channels
Clinical Chemistry
view channel
Existing Hospital Analyzers Can Identify Fake Liquid Medical Products
Counterfeit and substandard medicines remain a serious global health threat, with World Health Organization estimates suggesting that 10.5% of medicines in low- and middle-income countries are either fake... Read more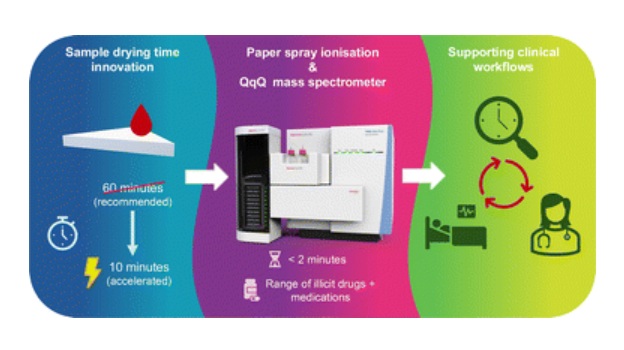
Rapid Blood Testing Method Aids Safer Decision-Making in Drug-Related Emergencies
Acute recreational drug toxicity is a frequent reason for emergency department visits, yet clinicians rarely have access to confirmatory toxicology results in real time. Instead, treatment decisions are... Read moreHematology
view channel
Rapid Cartridge-Based Test Aims to Expand Access to Hemoglobin Disorder Diagnosis
Sickle cell disease and beta thalassemia are hemoglobin disorders that often require referral to specialized laboratories for definitive diagnosis, delaying results for patients and clinicians.... Read more
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read moreImmunology
view channel
New Biomarker Predicts Chemotherapy Response in Triple-Negative Breast Cancer
Triple-negative breast cancer is an aggressive form of breast cancer in which patients often show widely varying responses to chemotherapy. Predicting who will benefit from treatment remains challenging,... Read moreBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read more
Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
Immunotherapy has transformed cancer treatment, but only a small proportion of patients experience lasting benefit, with response rates often remaining between 10% and 20%. Clinicians currently lack reliable... Read moreMicrobiology
view channel
Rapid Test Promises Faster Answers for Drug-Resistant Infections
Drug-resistant pathogens continue to pose a growing threat in healthcare facilities, where delayed detection can impede outbreak control and increase mortality. Candida auris is notoriously difficult to... Read more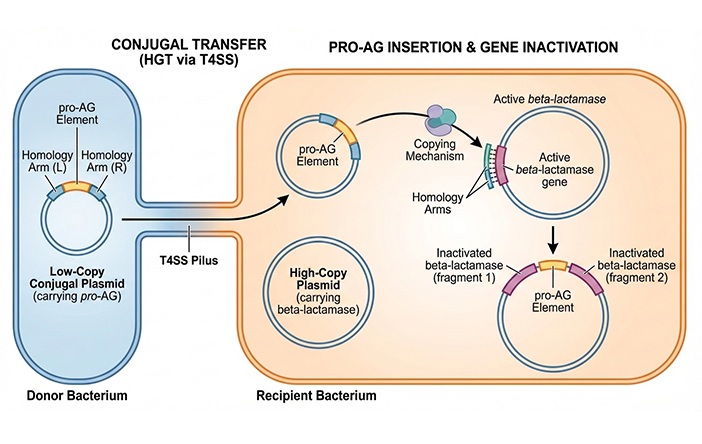
CRISPR-Based Technology Neutralizes Antibiotic-Resistant Bacteria
Antibiotic resistance has accelerated into a global health crisis, with projections estimating more than 10 million deaths per year by 2050 as drug-resistant “superbugs” continue to spread.... Read more
Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
Alzheimer’s disease affects approximately 6.7 million people in the United States and nearly 50 million worldwide, yet early cognitive decline remains difficult to characterize. Increasing evidence suggests... Read morePathology
view channel
Single Sample Classifier Predicts Cancer-Associated Fibroblast Subtypes in Patient Samples
Pancreatic ductal adenocarcinoma (PDAC) remains one of the deadliest cancers, in part because of its dense tumor microenvironment that influences how tumors grow and respond to treatment.... Read more
New AI-Driven Platform Standardizes Tuberculosis Smear Microscopy Workflow
Sputum smear microscopy remains central to tuberculosis treatment monitoring and follow-up, particularly in high‑burden settings where serial testing is routine. Yet consistent, repeatable bacillary assessment... Read more
AI Tool Uses Blood Biomarkers to Predict Transplant Complications Before Symptoms Appear
Stem cell and bone marrow transplants can be lifesaving, but serious complications may arise months after patients leave the hospital. One of the most dangerous is chronic graft-versus-host disease, in... Read moreTechnology
view channel
Blood Test “Clocks” Predict Start of Alzheimer’s Symptoms
More than 7 million Americans live with Alzheimer’s disease, and related health and long-term care costs are projected to reach nearly USD 400 billion in 2025. The disease has no cure, and symptoms often... Read more
AI-Powered Biomarker Predicts Liver Cancer Risk
Liver cancer, or hepatocellular carcinoma, causes more than 800,000 deaths worldwide each year and often goes undetected until late stages. Even after treatment, recurrence rates reach 70% to 80%, contributing... Read more
Robotic Technology Unveiled for Automated Diagnostic Blood Draws
Routine diagnostic blood collection is a high‑volume task that can strain staffing and introduce human‑dependent variability, with downstream implications for sample quality and patient experience.... Read more
ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
Clinical laboratories generate billions of test results each year, creating a treasure trove of data with the potential to support more personalized testing, improve operational efficiency, and enhance patient care.... Read moreIndustry
view channel
QuidelOrtho Collaborates with Lifotronic to Expand Global Immunoassay Portfolio
QuidelOrtho (San Diego, CA, USA) has entered a long-term strategic supply agreement with Lifotronic Technology (Shenzhen, China) to expand its global immunoassay portfolio and accelerate customer access... Read more
















