Blood Test Predicts Response to Immunotherapy in Metastatic NSCLC
|
By LabMedica International staff writers Posted on 10 Mar 2020 |
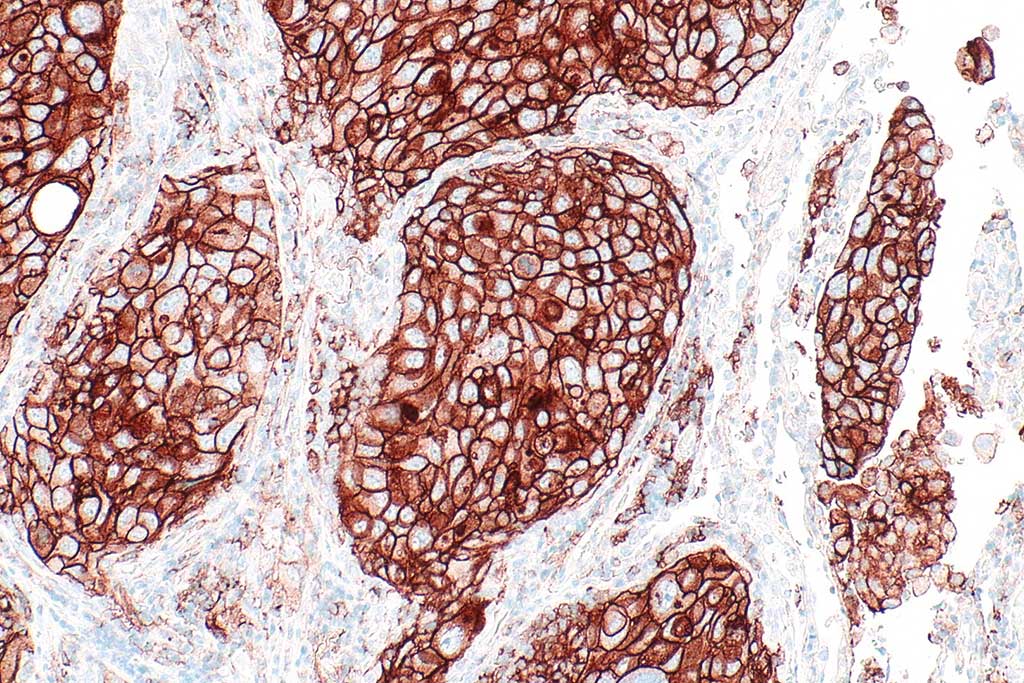
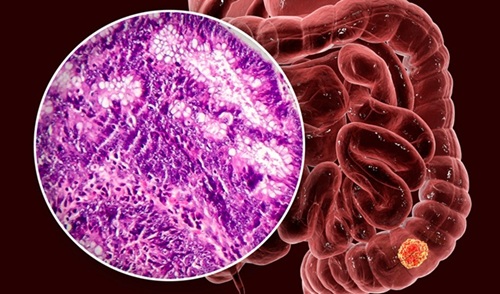
Image: Immunohistological micrograph showing a programmed death-ligand 1 (PD-L1) positive non-small cell lung carcinoma (Photo courtesy of Creative Commons BY-SA 4.0/Wikimedia).
Non-small cell lung cancer (NSCLC) patients with higher measures of tumor mutations that show up in a blood test generally have a better clinical response to PD-1-based immunotherapy treatments than patients with a lower measure of mutations.
NSCLC is the most common form of lung cancer, accounting for about 84% of all lung cancer cases. In patients with metastatic disease the five-year survival rate is just 6%. Immunotherapy with a PD-1 inhibitor, either alone or in combination with chemotherapy, is the standard first-line treatment in these cases when cancers do not have a targetable mutation.
Oncologists at the University of Pennsylvania (Philadelphia, PA, USA) and their colleagues enrolled 66 patients with newly diagnosed metastatic non-small cell lung cancer (mNSCLC) starting first-line pembrolizumab-based therapy, either alone or in combination with chemotherapy. Response was assessed using response evaluation criteria in solid tumors (RECIST 1.1.) rules. Associations were made for patient characteristics, 6-month durable clinical benefit (DCB), progression free survival (PFS), and overall survival (OS).
With a simple blood draw, the scientists can screen for mutations in 500 different genes. They used this liquid biopsy panel to measure the tumor mutational burden (TMB), essentially the number of mutations detectable in the blood of the enrolled patients, 52 of whom were evaluable for the trial. TMB is typically reported as mutations per megabase (Mb), which is the number non-synonymous, somatic mutations divided by the size of the genome coding area. The median TMB was 16.8 mutations per Mb and was significantly higher for patients who experienced a durable clinical benefit (DCB) compared to those who did not. A DCB means a patient experienced a complete response, a partial response, or stable disease for more than six months. Patients who achieved a DCB had a median of 21.3 mutations per Mb, compared to 12.4 in patients who did not achieve a DCB.
The team then examined the progression-free survival (PFS) and overall survival (OS) of both groups. The 28 patients with more than 16 detectable mutations per Mb had a median PFS of 14.1 months compared to 4.7 months for the 24 patients in the lower TMB group. Median OS was not reached for the high TMB group. The low TMB group had a median OS of 8.8 months.
Erica L. Carpenter, MBA, PhD, an assistant professor and senior author of the study, said, “We believe this is the largest study to show correlation between blood-based tumor mutational burden and clinical outcomes after first-line PD-1-based treatment, including combination chemo-immunotherapy, for NSCLC.”
The authors concluded that pTMB greater than or equal to 16 mutations/Mb is associated with improved PFS after first-line standard of care pembrolizumab-based therapy in mNSCLC. STK11/KEAP1/PTEN and ERBB2 mutations may help identify pTMB-high patients unlikely to respond. The study was published on February 26, 2020 in the journal Clinical Cancer Research.
Related Links:
University of Pennsylvania
NSCLC is the most common form of lung cancer, accounting for about 84% of all lung cancer cases. In patients with metastatic disease the five-year survival rate is just 6%. Immunotherapy with a PD-1 inhibitor, either alone or in combination with chemotherapy, is the standard first-line treatment in these cases when cancers do not have a targetable mutation.
Oncologists at the University of Pennsylvania (Philadelphia, PA, USA) and their colleagues enrolled 66 patients with newly diagnosed metastatic non-small cell lung cancer (mNSCLC) starting first-line pembrolizumab-based therapy, either alone or in combination with chemotherapy. Response was assessed using response evaluation criteria in solid tumors (RECIST 1.1.) rules. Associations were made for patient characteristics, 6-month durable clinical benefit (DCB), progression free survival (PFS), and overall survival (OS).
With a simple blood draw, the scientists can screen for mutations in 500 different genes. They used this liquid biopsy panel to measure the tumor mutational burden (TMB), essentially the number of mutations detectable in the blood of the enrolled patients, 52 of whom were evaluable for the trial. TMB is typically reported as mutations per megabase (Mb), which is the number non-synonymous, somatic mutations divided by the size of the genome coding area. The median TMB was 16.8 mutations per Mb and was significantly higher for patients who experienced a durable clinical benefit (DCB) compared to those who did not. A DCB means a patient experienced a complete response, a partial response, or stable disease for more than six months. Patients who achieved a DCB had a median of 21.3 mutations per Mb, compared to 12.4 in patients who did not achieve a DCB.
The team then examined the progression-free survival (PFS) and overall survival (OS) of both groups. The 28 patients with more than 16 detectable mutations per Mb had a median PFS of 14.1 months compared to 4.7 months for the 24 patients in the lower TMB group. Median OS was not reached for the high TMB group. The low TMB group had a median OS of 8.8 months.
Erica L. Carpenter, MBA, PhD, an assistant professor and senior author of the study, said, “We believe this is the largest study to show correlation between blood-based tumor mutational burden and clinical outcomes after first-line PD-1-based treatment, including combination chemo-immunotherapy, for NSCLC.”
The authors concluded that pTMB greater than or equal to 16 mutations/Mb is associated with improved PFS after first-line standard of care pembrolizumab-based therapy in mNSCLC. STK11/KEAP1/PTEN and ERBB2 mutations may help identify pTMB-high patients unlikely to respond. The study was published on February 26, 2020 in the journal Clinical Cancer Research.
Related Links:
University of Pennsylvania
Latest Pathology News
- Engineered Yeast Cells Enable Rapid Testing of Cancer Immunotherapy
- First-Of-Its-Kind Test Identifies Autism Risk at Birth
- AI Algorithms Improve Genetic Mutation Detection in Cancer Diagnostics
- Skin Biopsy Offers New Diagnostic Method for Neurodegenerative Diseases
- Fast Label-Free Method Identifies Aggressive Cancer Cells
- New X-Ray Method Promises Advances in Histology
- Single-Cell Profiling Technique Could Guide Early Cancer Detection
- Intraoperative Tumor Histology to Improve Cancer Surgeries
- Rapid Stool Test Could Help Pinpoint IBD Diagnosis
- AI-Powered Label-Free Optical Imaging Accurately Identifies Thyroid Cancer During Surgery
- Deep Learning–Based Method Improves Cancer Diagnosis
- ADLM Updates Expert Guidance on Urine Drug Testing for Patients in Emergency Departments
- New Age-Based Blood Test Thresholds to Catch Ovarian Cancer Earlier
- Genetics and AI Improve Diagnosis of Aortic Stenosis
- AI Tool Simultaneously Identifies Genetic Mutations and Disease Type
- Rapid Low-Cost Tests Can Prevent Child Deaths from Contaminated Medicinal Syrups
Channels
Clinical Chemistry
view channel
New PSA-Based Prognostic Model Improves Prostate Cancer Risk Assessment
Prostate cancer is the second-leading cause of cancer death among American men, and about one in eight will be diagnosed in their lifetime. Screening relies on blood levels of prostate-specific antigen... Read more
Extracellular Vesicles Linked to Heart Failure Risk in CKD Patients
Chronic kidney disease (CKD) affects more than 1 in 7 Americans and is strongly associated with cardiovascular complications, which account for more than half of deaths among people with CKD.... Read moreMolecular Diagnostics
view channel
Diagnostic Device Predicts Treatment Response for Brain Tumors Via Blood Test
Glioblastoma is one of the deadliest forms of brain cancer, largely because doctors have no reliable way to determine whether treatments are working in real time. Assessing therapeutic response currently... Read more
Blood Test Detects Early-Stage Cancers by Measuring Epigenetic Instability
Early-stage cancers are notoriously difficult to detect because molecular changes are subtle and often missed by existing screening tools. Many liquid biopsies rely on measuring absolute DNA methylation... Read more
“Lab-On-A-Disc” Device Paves Way for More Automated Liquid Biopsies
Extracellular vesicles (EVs) are tiny particles released by cells into the bloodstream that carry molecular information about a cell’s condition, including whether it is cancerous. However, EVs are highly... Read more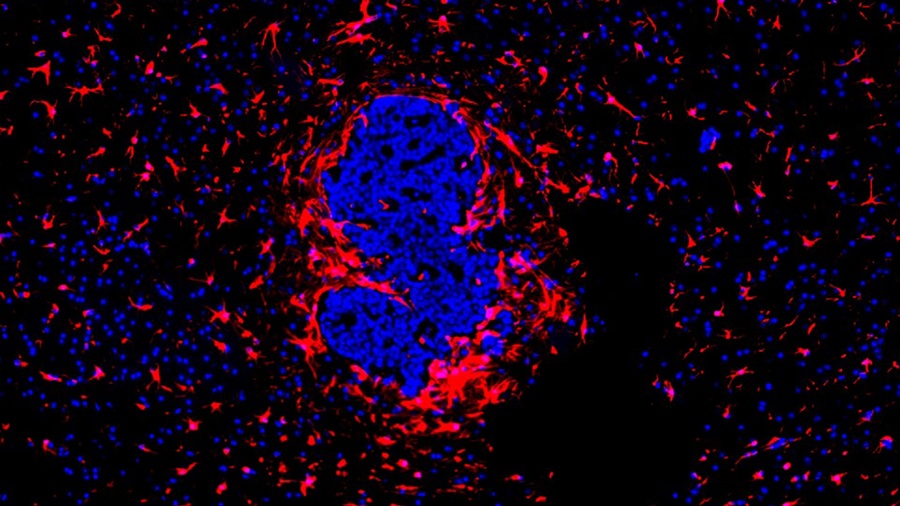
Blood Test Identifies Inflammatory Breast Cancer Patients at Increased Risk of Brain Metastasis
Brain metastasis is a frequent and devastating complication in patients with inflammatory breast cancer, an aggressive subtype with limited treatment options. Despite its high incidence, the biological... Read moreHematology
view channel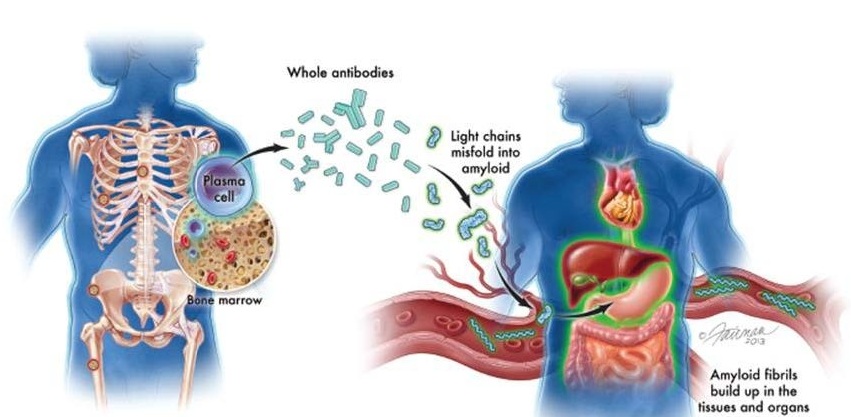
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read more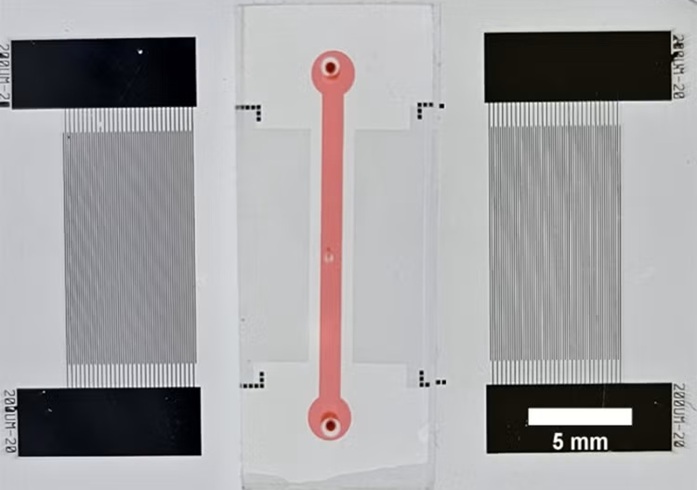
Fast and Easy Test Could Revolutionize Blood Transfusions
Blood transfusions are a cornerstone of modern medicine, yet red blood cells can deteriorate quietly while sitting in cold storage for weeks. Although blood units have a fixed expiration date, cells from... Read more
Automated Hemostasis System Helps Labs of All Sizes Optimize Workflow
High-volume hemostasis sections must sustain rapid turnaround while managing reruns and reflex testing. Manual tube handling and preanalytical checks can strain staff time and increase opportunities for error.... Read more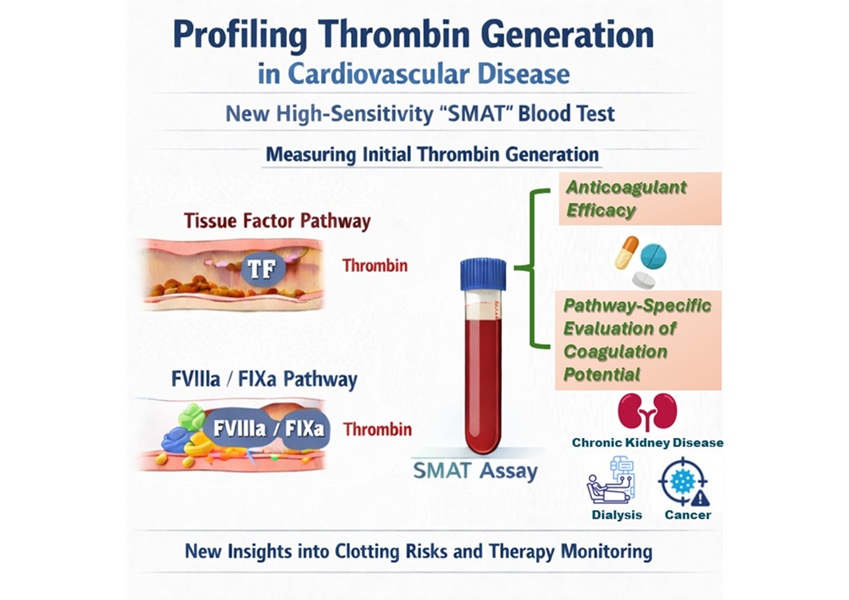
High-Sensitivity Blood Test Improves Assessment of Clotting Risk in Heart Disease Patients
Blood clotting is essential for preventing bleeding, but even small imbalances can lead to serious conditions such as thrombosis or dangerous hemorrhage. In cardiovascular disease, clinicians often struggle... Read moreImmunology
view channelBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read more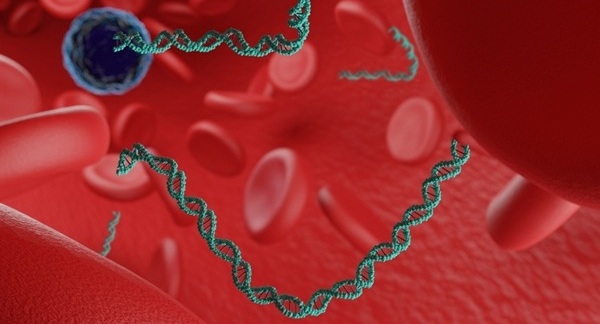
Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
Immunotherapy has transformed cancer treatment, but only a small proportion of patients experience lasting benefit, with response rates often remaining between 10% and 20%. Clinicians currently lack reliable... Read moreMicrobiology
view channel
Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
Alzheimer’s disease affects approximately 6.7 million people in the United States and nearly 50 million worldwide, yet early cognitive decline remains difficult to characterize. Increasing evidence suggests... Read moreAI-Powered Platform Enables Rapid Detection of Drug-Resistant C. Auris Pathogens
Infections caused by the pathogenic yeast Candida auris pose a significant threat to hospitalized patients, particularly those with weakened immune systems or those who have invasive medical devices.... Read moreTechnology
view channel
Robotic Technology Unveiled for Automated Diagnostic Blood Draws
Routine diagnostic blood collection is a high‑volume task that can strain staffing and introduce human‑dependent variability, with downstream implications for sample quality and patient experience.... Read more
ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
Clinical laboratories generate billions of test results each year, creating a treasure trove of data with the potential to support more personalized testing, improve operational efficiency, and enhance patient care.... Read moreAptamer Biosensor Technology to Transform Virus Detection
Rapid and reliable virus detection is essential for controlling outbreaks, from seasonal influenza to global pandemics such as COVID-19. Conventional diagnostic methods, including cell culture, antigen... Read more
AI Models Could Predict Pre-Eclampsia and Anemia Earlier Using Routine Blood Tests
Pre-eclampsia and anemia are major contributors to maternal and child mortality worldwide, together accounting for more than half a million deaths each year and leaving millions with long-term health complications.... Read moreIndustry
view channelNew Collaboration Brings Automated Mass Spectrometry to Routine Laboratory Testing
Mass spectrometry is a powerful analytical technique that identifies and quantifies molecules based on their mass and electrical charge. Its high selectivity, sensitivity, and accuracy make it indispensable... Read more
AI-Powered Cervical Cancer Test Set for Major Rollout in Latin America
Noul Co., a Korean company specializing in AI-based blood and cancer diagnostics, announced it will supply its intelligence (AI)-based miLab CER cervical cancer diagnostic solution to Mexico under a multi‑year... Read more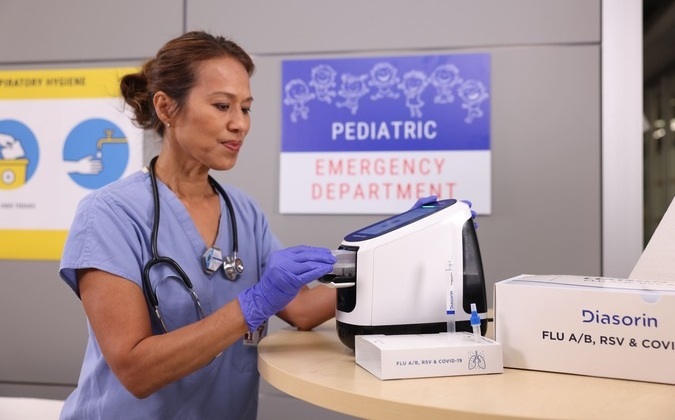
Diasorin and Fisher Scientific Enter into US Distribution Agreement for Molecular POC Platform
Diasorin (Saluggia, Italy) has entered into an exclusive distribution agreement with Fisher Scientific, part of Thermo Fisher Scientific (Waltham, MA, USA), for the LIAISON NES molecular point-of-care... Read more