High Plasma Glucose Raises Baby Heart-Defect Risk
|
By LabMedica International staff writers Posted on 27 Dec 2017 |

Image: Testing for blood glucose levels during early pregnancy to assess the risk of congenital heart disease (Photo courtesy of Paras Hospitals).
For many years, physicians have known that women with diabetes face an increased risk of giving birth to babies with heart defects and some studies have also suggested a link between nondiabetic mothers' blood sugar levels and babies' heart defect risk.
One challenge associated with conducting such studies was the fact that maternal blood glucose is not routinely measured in nondiabetic pregnant women. Instead, women typically receive an oral glucose tolerance test halfway through pregnancy to determine whether they have gestational diabetes, but this test is performed well after the fetal heart has formed.
A team of scientists mainly from Stanford University Medical Center (Stanford, CA, USA) studied medical records from 19,107 pairs of mothers and their babies born between 2009 and 2015. The records included details of the mothers' prenatal care, including blood test results and any cardiac diagnoses made for the babies during pregnancy or after birth. The scientists analyzed blood glucose levels from any blood sample collected from the mothers between four weeks prior to the estimated date of conception and the end of the 14th gestational week, just after the completion of the first trimester of pregnancy. These early blood glucose measurements were available for 2,292, or 13%, of women in the study. They also looked at the results of oral glucose tolerance tests (OGTT) performed around 20 weeks of gestation, which were available for 9,511, or just under half, of the women in the study.
After excluding women who had diabetes before pregnancy or who developed it during pregnancy, the results showed that the risk of giving birth to a child with a congenital heart defect was elevated by 8% for every increase of 10 mg/dL in blood glucose levels in the early stages of pregnancy. The mean early glucose value was 96 mg/dL (5.3 mmol/L) in pregnancies without congenital heart disease (CHD) versus 107 mg/dL (6.0 mmol/L) in pregnancies with CHD. The respective mean 1-hour OGTT values were 117 mg/dL (6.5 mmol/L) and 122 mg/dL (6.8 mmol/L).
The findings demonstrate that higher random plasma glucose values measured during early pregnancy correlate with increased risk for congenital heart disease in offspring of mothers who do not have diabetes. Furthermore, plasma glucose measured during early pregnancy was more associated with risk for congenital heart disease in offspring, compared with the OGTT which is often used to risk-stratify pregnancies for fetal-echocardiographic screening.
James R. Priest, MD, an assistant professor of pediatric cardiology and the senior author of the study, said, “Most women who have a child with congenital heart disease are not diabetic. We found that in women who don't already have diabetes or develop diabetes during pregnancy, we can still measure risk for having a child with congenital heart disease by looking at their glucose values during the first trimester of pregnancy.” The study was published on December 15, 2017, in The Journal of Pediatrics.
Related Links:
Stanford University Medical Center
One challenge associated with conducting such studies was the fact that maternal blood glucose is not routinely measured in nondiabetic pregnant women. Instead, women typically receive an oral glucose tolerance test halfway through pregnancy to determine whether they have gestational diabetes, but this test is performed well after the fetal heart has formed.
A team of scientists mainly from Stanford University Medical Center (Stanford, CA, USA) studied medical records from 19,107 pairs of mothers and their babies born between 2009 and 2015. The records included details of the mothers' prenatal care, including blood test results and any cardiac diagnoses made for the babies during pregnancy or after birth. The scientists analyzed blood glucose levels from any blood sample collected from the mothers between four weeks prior to the estimated date of conception and the end of the 14th gestational week, just after the completion of the first trimester of pregnancy. These early blood glucose measurements were available for 2,292, or 13%, of women in the study. They also looked at the results of oral glucose tolerance tests (OGTT) performed around 20 weeks of gestation, which were available for 9,511, or just under half, of the women in the study.
After excluding women who had diabetes before pregnancy or who developed it during pregnancy, the results showed that the risk of giving birth to a child with a congenital heart defect was elevated by 8% for every increase of 10 mg/dL in blood glucose levels in the early stages of pregnancy. The mean early glucose value was 96 mg/dL (5.3 mmol/L) in pregnancies without congenital heart disease (CHD) versus 107 mg/dL (6.0 mmol/L) in pregnancies with CHD. The respective mean 1-hour OGTT values were 117 mg/dL (6.5 mmol/L) and 122 mg/dL (6.8 mmol/L).
The findings demonstrate that higher random plasma glucose values measured during early pregnancy correlate with increased risk for congenital heart disease in offspring of mothers who do not have diabetes. Furthermore, plasma glucose measured during early pregnancy was more associated with risk for congenital heart disease in offspring, compared with the OGTT which is often used to risk-stratify pregnancies for fetal-echocardiographic screening.
James R. Priest, MD, an assistant professor of pediatric cardiology and the senior author of the study, said, “Most women who have a child with congenital heart disease are not diabetic. We found that in women who don't already have diabetes or develop diabetes during pregnancy, we can still measure risk for having a child with congenital heart disease by looking at their glucose values during the first trimester of pregnancy.” The study was published on December 15, 2017, in The Journal of Pediatrics.
Related Links:
Stanford University Medical Center
Latest Clinical Chem. News
- New Blood Test Index Offers Earlier Detection of Liver Scarring
- Electronic Nose Smells Early Signs of Ovarian Cancer in Blood
- Simple Blood Test Offers New Path to Alzheimer’s Assessment in Primary Care
- Existing Hospital Analyzers Can Identify Fake Liquid Medical Products
- Rapid Blood Testing Method Aids Safer Decision-Making in Drug-Related Emergencies
- New PSA-Based Prognostic Model Improves Prostate Cancer Risk Assessment
- Extracellular Vesicles Linked to Heart Failure Risk in CKD Patients
- Study Compares Analytical Performance of Quantitative Hepatitis B Surface Antigen Assays
- Blood Test Could Predict and Identify Early Relapses in Myeloma Patients
- Compact Raman Imaging System Detects Subtle Tumor Signals
- Noninvasive Blood-Glucose Monitoring to Replace Finger Pricks for Diabetics
- POC Breath Diagnostic System to Detect Pneumonia-Causing Pathogens
- Online Tool Detects Drug Exposure Directly from Patient Samples
- Chemical Imaging Probe Could Track and Treat Prostate Cancer
- Mismatch Between Two Common Kidney Function Tests Indicates Serious Health Problems
- VOCs Show Promise for Early Multi-Cancer Detection
Channels
Molecular Diagnostics
view channel
New Blood Test Can Help Predict Testicular Cancer Recurrence
Stage 1 testicular germ cell tumor is typically treated with surgery followed by active surveillance. Although most patients experience strong long-term outcomes, about one in four will see their cancer... Read more
New Test Detects Alzheimer’s by Analyzing Altered Protein Shapes in Blood
Alzheimer’s disease begins developing years before memory loss or other symptoms become visible. Misfolded proteins gradually accumulate in the brain, disrupting normal cellular processes.... Read more
New Diagnostic Markers for Multiple Sclerosis Discovered in Cerebrospinal Fluid
Multiple sclerosis (MS) affects nearly three million people worldwide and can cause symptoms such as numbness, visual disturbances, fatigue, and neurological disability. Diagnosing the disease can be challenging... Read moreHematology
view channel
Rapid Cartridge-Based Test Aims to Expand Access to Hemoglobin Disorder Diagnosis
Sickle cell disease and beta thalassemia are hemoglobin disorders that often require referral to specialized laboratories for definitive diagnosis, delaying results for patients and clinicians.... Read more
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read moreImmunology
view channel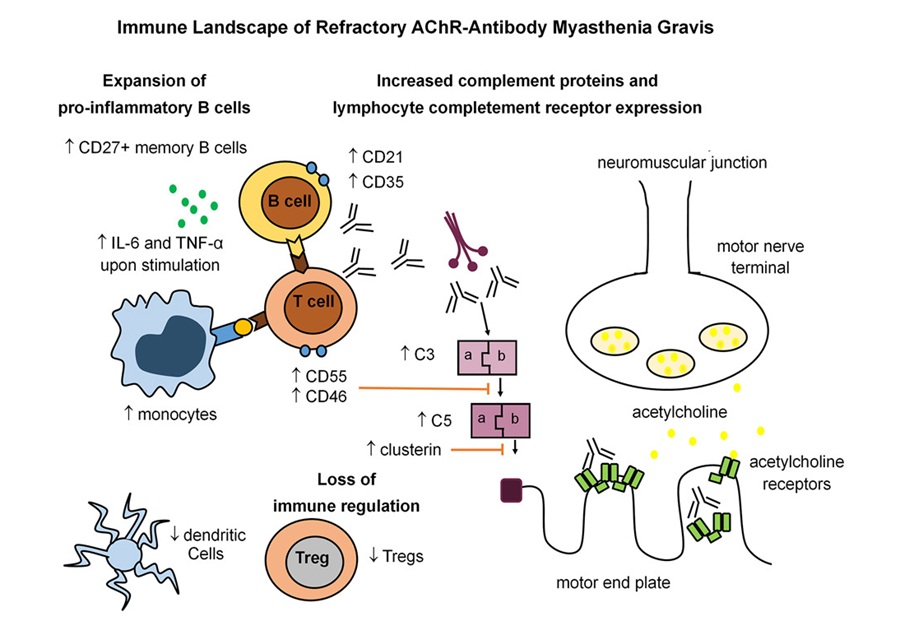
Immune Signature Identified in Treatment-Resistant Myasthenia Gravis
Myasthenia gravis is a rare autoimmune disorder in which immune attack at the neuromuscular junction causes fluctuating weakness that can impair vision, movement, speech, swallowing, and breathing.... Read more
New Biomarker Predicts Chemotherapy Response in Triple-Negative Breast Cancer
Triple-negative breast cancer is an aggressive form of breast cancer in which patients often show widely varying responses to chemotherapy. Predicting who will benefit from treatment remains challenging,... Read moreBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read moreMicrobiology
view channel
Rapid Sequencing Could Transform Tuberculosis Care
Tuberculosis remains the world’s leading cause of death from a single infectious agent, responsible for more than one million deaths each year. Diagnosing and monitoring the disease can be slow because... Read more
Blood-Based Viral Signature Identified in Crohn’s Disease
Crohn’s disease is a chronic inflammatory intestinal disorder affecting approximately 0.4% of the European population, with symptoms and progression that vary widely. Although viral components of the microbiome... Read morePathology
view channel
Molecular Imaging to Reduce Need for Melanoma Biopsies
Melanoma is the deadliest form of skin cancer and accounts for the vast majority of skin cancer-related deaths. Because early melanomas can closely resemble benign moles, clinicians often rely on visual... Read more
Urine Specimen Collection System Improves Diagnostic Accuracy and Efficiency
Urine testing is a critical, non-invasive diagnostic tool used to detect conditions such as pregnancy, urinary tract infections, metabolic disorders, cancer, and kidney disease. However, contaminated or... Read moreTechnology
view channel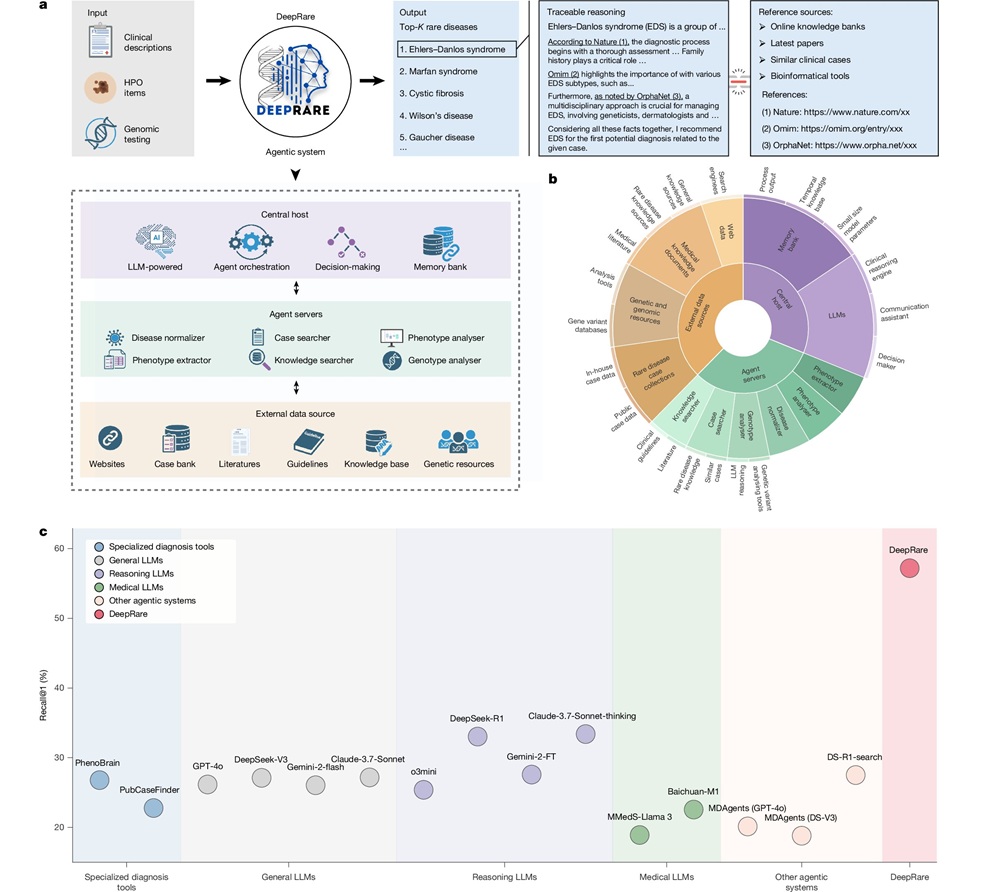
AI Model Outperforms Clinicians in Rare Disease Detection
Rare diseases affect an estimated 300 million people worldwide, yet diagnosis is often protracted and error-prone. Many conditions present with heterogeneous signs that overlap with common disorders, leading... Read more
AI-Driven Diagnostic Demonstrates High Accuracy in Detecting Periprosthetic Joint Infection
Periprosthetic joint infection (PJI) is a rare but serious complication affecting 1% to 2% of primary joint replacement surgeries. The condition occurs when bacteria or fungi infect tissues around an implanted... Read moreIndustry
view channel
Cepheid Joins CDC Initiative to Strengthen U.S. Pandemic Testing Preparednesss
Cepheid (Sunnyvale, CA, USA) has been selected by the U.S. Centers for Disease Control and Prevention (CDC) as one of four national collaborators in a federal initiative to speed rapid diagnostic technologies... Read more
QuidelOrtho Collaborates with Lifotronic to Expand Global Immunoassay Portfolio
QuidelOrtho (San Diego, CA, USA) has entered a long-term strategic supply agreement with Lifotronic Technology (Shenzhen, China) to expand its global immunoassay portfolio and accelerate customer access... Read more