New Technology Could Help Diagnose Sepsis in Hours
|
By LabMedica International staff writers Posted on 08 Nov 2016 |

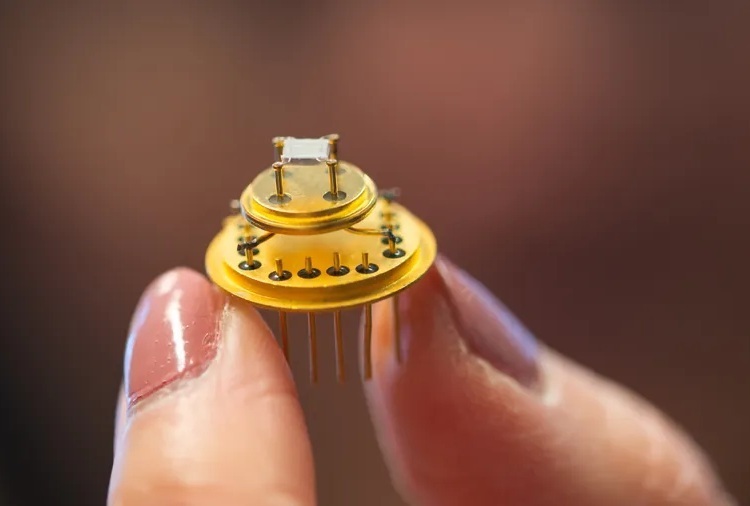
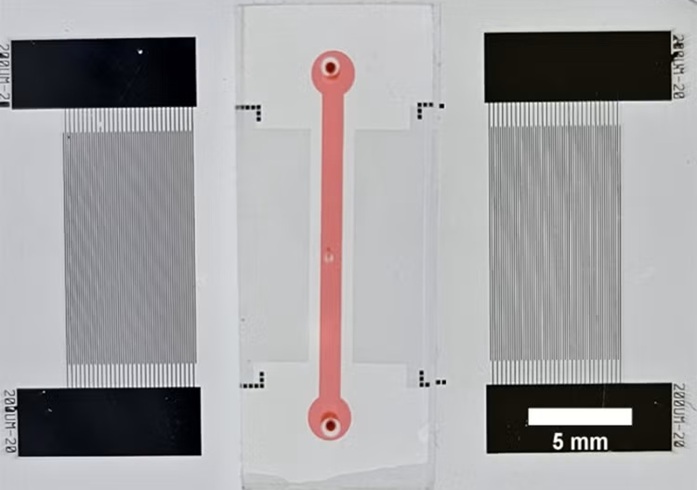
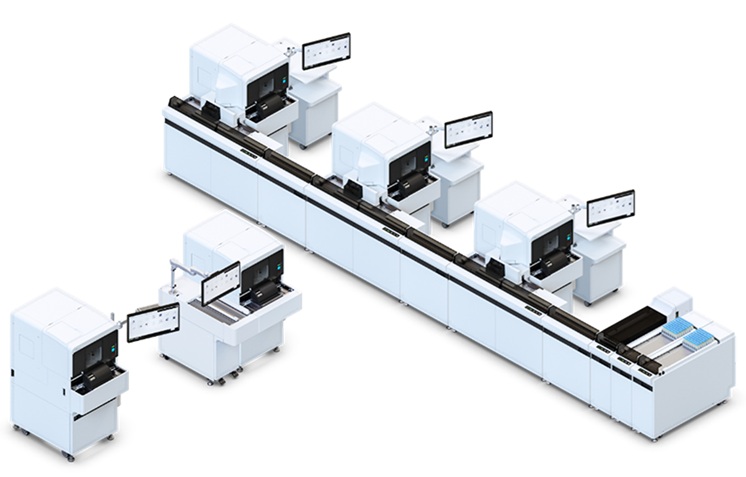
Image: A new microfluidics chip being developed for a blood test to rapidly diagnose sepsis would enable doctors to intervene sooner and as necessary, as well as to monitor treatment progress (Photo courtesy of Pappas Lab / Texas Tech University).
Researchers have developed a microfluidics chip that detected mock-sepsis conditions within a few hours, instead of at least two days by currently used methods. As sepsis left untreated can be fatal in as little as two days, a rapid blood test would provide medical professionals with a critical window of time in which to begin early antibiotics treatment of diagnosed patients.
“Normally when you detect sepsis, you do it through bacterial culture; that takes two days on the short end to 15 days on the long end. Most people die of sepsis at two days. The detection currently is on the exact same time scale as mortality, so we’re trying to speed that up,” said Dimitri Pappas, associate professor of chemistry at Texas Tech University (Lubbock, TX, USA), “Instead of the bacteria, we’re looking at the body’s immune response to those bacteria, because that’s what you really care about: the bacteria cause the infection, but it’s the body’s response that causes sepsis.” It begins with a systemic inflammatory response then progresses into sepsis and eventually septic shock, in which blood pressure plummets and organs fail.
“In the elderly, in people who are immune-compromised – people who have had surgeries, for example, or burns or they’re already fighting off infection – and in children as well, you see a runaway immune response where the body’s act of saving itself can actually be lethal,” said Prof. Pappas. When not fatal, sepsis can result in amputation of a limb or prolonged hospitalization.
Sepsis is suspected by a patient’s abnormal body temperature and rapid heart and breathing rates. “Those are all incredibly crude measurements,” said Prof. Pappas, “It leads to a lot of false positives.” Because doctors know the bacterial culture likely will take longer than a septic patient’s life span, they often order treatment immediately. “The way they treat sepsis right now is through a massive antibiotic administration,” said Prof. Pappas “That’s good, actually, but if you do it prophylactically and when it’s not needed, you’re basically helping create drug-resistant bacteria. So there’s a need to detect sepsis and to treat it but not to over treat it.”
To successfully treat septic patients, doctors need two critical pieces of information: the microorganism causing the infection and whether it can be eradicated by antibiotics. “Waiting for that information over several days is one of the main problems and reasons for the devastating outcomes,” said Dr. John Griswold, professor and chair emeritus, Department of Surgery, TTU’s Health Sciences Center, “Dr. Pappas has developed a test that should give us at least the indication of bacterial invasion within a matter of hours as opposed to days. The sooner we have an indication of microorganism invasion, the sooner we are on the path to successful treatment of these very sick patients.” Prof. Griswold added that sepsis is considered one of the most costly diseases in healthcare.
Prof. Pappas and graduate student Ye Zhang recently filed a provisional patent for a microfluidics chip that can speed up detection. “We can take a blood sample, introduce it into this chip and capture one cell type or move fluids around and add chemicals to dye the cells certain colors and do diagnostic measurements,” said Prof. Pappas.
Using their chip, a sepsis diagnosis can be confirmed in just four hours. “That rapid detection will let doctors intervene sooner and intervene when necessary, but it also allows them not just to detect it but to follow up treatment,” said Prof. Pappas, “you can follow and retest them over time to make sure the body’s response is returning to normal.”
Another advantage is that the chip requires less than a drop of blood per test. “It’s so minimal we could do this multiple times throughout the course of the treatment of the patient. If they’re not septic at hour zero, but they still look septic by other methods, we could test them in six hours and see if they’ve progressed or not,” said Prof. Pappas.
The chips are designed to detect certain white blood cells activated by the immune system to fight the infection. To this point, all testing has been done with using transformed stem cells. “We have stem cells that we transform into white blood cells, then we trick them into thinking there’s an infection. We add those infection-response blood cells to human blood in the concentrations we want and the timeframe we want,” said Prof. Pappas. The blood is then tested to see if the chip registers it as septic. “That allows us to refine the technique to make sure it’ll work, because human samples are far more variable,” he said, “Before moving to humans, we had to show it’ll work in the first place.”
“Ultimately, this type of work – for it to be successful – has to be commercialized,” he said. “It has to be out there in the hands of physicians.” The next step is to test the chip with patient blood. In collaboration with Dr. Griswold, Dr. Pappas will now begin enrolling patients.
Related Links:
Texas Tech University
“Normally when you detect sepsis, you do it through bacterial culture; that takes two days on the short end to 15 days on the long end. Most people die of sepsis at two days. The detection currently is on the exact same time scale as mortality, so we’re trying to speed that up,” said Dimitri Pappas, associate professor of chemistry at Texas Tech University (Lubbock, TX, USA), “Instead of the bacteria, we’re looking at the body’s immune response to those bacteria, because that’s what you really care about: the bacteria cause the infection, but it’s the body’s response that causes sepsis.” It begins with a systemic inflammatory response then progresses into sepsis and eventually septic shock, in which blood pressure plummets and organs fail.
“In the elderly, in people who are immune-compromised – people who have had surgeries, for example, or burns or they’re already fighting off infection – and in children as well, you see a runaway immune response where the body’s act of saving itself can actually be lethal,” said Prof. Pappas. When not fatal, sepsis can result in amputation of a limb or prolonged hospitalization.
Sepsis is suspected by a patient’s abnormal body temperature and rapid heart and breathing rates. “Those are all incredibly crude measurements,” said Prof. Pappas, “It leads to a lot of false positives.” Because doctors know the bacterial culture likely will take longer than a septic patient’s life span, they often order treatment immediately. “The way they treat sepsis right now is through a massive antibiotic administration,” said Prof. Pappas “That’s good, actually, but if you do it prophylactically and when it’s not needed, you’re basically helping create drug-resistant bacteria. So there’s a need to detect sepsis and to treat it but not to over treat it.”
To successfully treat septic patients, doctors need two critical pieces of information: the microorganism causing the infection and whether it can be eradicated by antibiotics. “Waiting for that information over several days is one of the main problems and reasons for the devastating outcomes,” said Dr. John Griswold, professor and chair emeritus, Department of Surgery, TTU’s Health Sciences Center, “Dr. Pappas has developed a test that should give us at least the indication of bacterial invasion within a matter of hours as opposed to days. The sooner we have an indication of microorganism invasion, the sooner we are on the path to successful treatment of these very sick patients.” Prof. Griswold added that sepsis is considered one of the most costly diseases in healthcare.
Prof. Pappas and graduate student Ye Zhang recently filed a provisional patent for a microfluidics chip that can speed up detection. “We can take a blood sample, introduce it into this chip and capture one cell type or move fluids around and add chemicals to dye the cells certain colors and do diagnostic measurements,” said Prof. Pappas.
Using their chip, a sepsis diagnosis can be confirmed in just four hours. “That rapid detection will let doctors intervene sooner and intervene when necessary, but it also allows them not just to detect it but to follow up treatment,” said Prof. Pappas, “you can follow and retest them over time to make sure the body’s response is returning to normal.”
Another advantage is that the chip requires less than a drop of blood per test. “It’s so minimal we could do this multiple times throughout the course of the treatment of the patient. If they’re not septic at hour zero, but they still look septic by other methods, we could test them in six hours and see if they’ve progressed or not,” said Prof. Pappas.
The chips are designed to detect certain white blood cells activated by the immune system to fight the infection. To this point, all testing has been done with using transformed stem cells. “We have stem cells that we transform into white blood cells, then we trick them into thinking there’s an infection. We add those infection-response blood cells to human blood in the concentrations we want and the timeframe we want,” said Prof. Pappas. The blood is then tested to see if the chip registers it as septic. “That allows us to refine the technique to make sure it’ll work, because human samples are far more variable,” he said, “Before moving to humans, we had to show it’ll work in the first place.”
“Ultimately, this type of work – for it to be successful – has to be commercialized,” he said. “It has to be out there in the hands of physicians.” The next step is to test the chip with patient blood. In collaboration with Dr. Griswold, Dr. Pappas will now begin enrolling patients.
Related Links:
Texas Tech University
Latest Technology News
- AI Model Outperforms Clinicians in Rare Disease Detection
- AI-Driven Diagnostic Demonstrates High Accuracy in Detecting Periprosthetic Joint Infection
- Blood Test “Clocks” Predict Start of Alzheimer’s Symptoms
- AI-Powered Biomarker Predicts Liver Cancer Risk
- Robotic Technology Unveiled for Automated Diagnostic Blood Draws
- ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
- Aptamer Biosensor Technology to Transform Virus Detection
- AI Models Could Predict Pre-Eclampsia and Anemia Earlier Using Routine Blood Tests
Channels
Clinical Chemistry
view channel
Blood Test Tracks Transplant Health Using Donor DNA
Organ transplantation offers life-saving treatment for patients with end-stage disease, but complications such as rejection remain a constant risk. Monitoring transplanted organs typically relies on invasive... Read more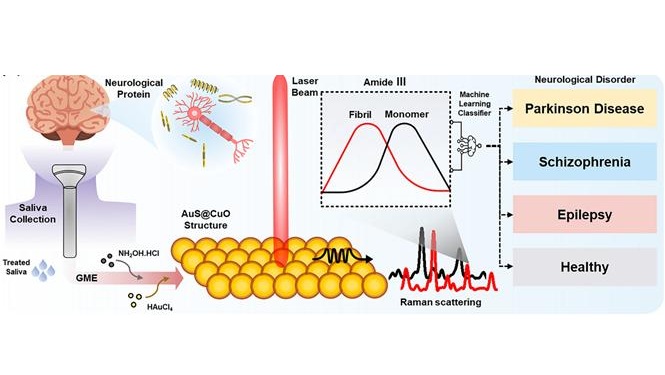
AI Sensor Detects Neurological Disorders Using Single Saliva Drop
Neurological disorders such as Parkinson’s disease and Alzheimer’s disease often develop gradually and present subtle symptoms in their early stages. Because early signs are frequently vague or atypical,... Read moreMolecular Diagnostics
view channel
Blood Test Predicts Dementia in Women 25 Years Before Symptoms Begin
Dementia and Alzheimer’s disease often develop silently over many years before symptoms appear. Detecting risk earlier could allow preventive strategies to begin long before memory problems interfere with... Read more
Serial Liquid Biopsies Reveal Therapy Resistance in Metastatic Prostate Cancer
Metastatic Prostate cancer can rapidly adapt under treatment, making it difficult to detect resistance before clinical progression. Genomic results from archival tumor tissue may no longer reflect the... Read moreHematology
view channel
Rapid Cartridge-Based Test Aims to Expand Access to Hemoglobin Disorder Diagnosis
Sickle cell disease and beta thalassemia are hemoglobin disorders that often require referral to specialized laboratories for definitive diagnosis, delaying results for patients and clinicians.... Read more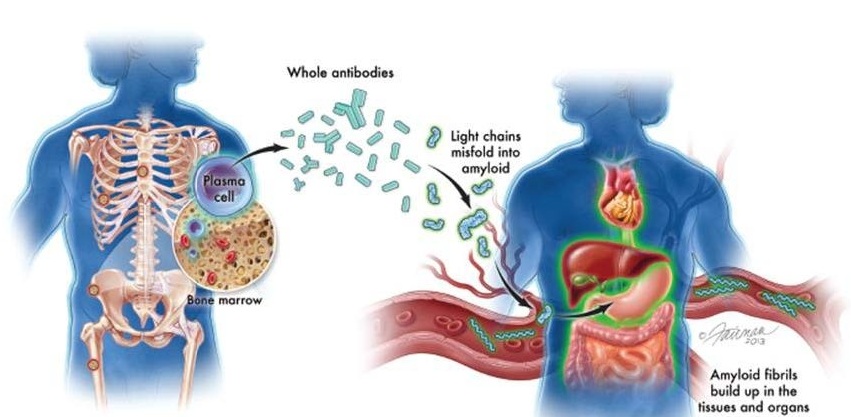
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read moreImmunology
view channel
Cancer Mutation ‘Fingerprints’ to Improve Prediction of Immunotherapy Response
Cancer cells accumulate thousands of genetic mutations, but not all mutations affect tumors in the same way. Some make cancer cells more visible to the immune system, while others allow tumors to evade... Read more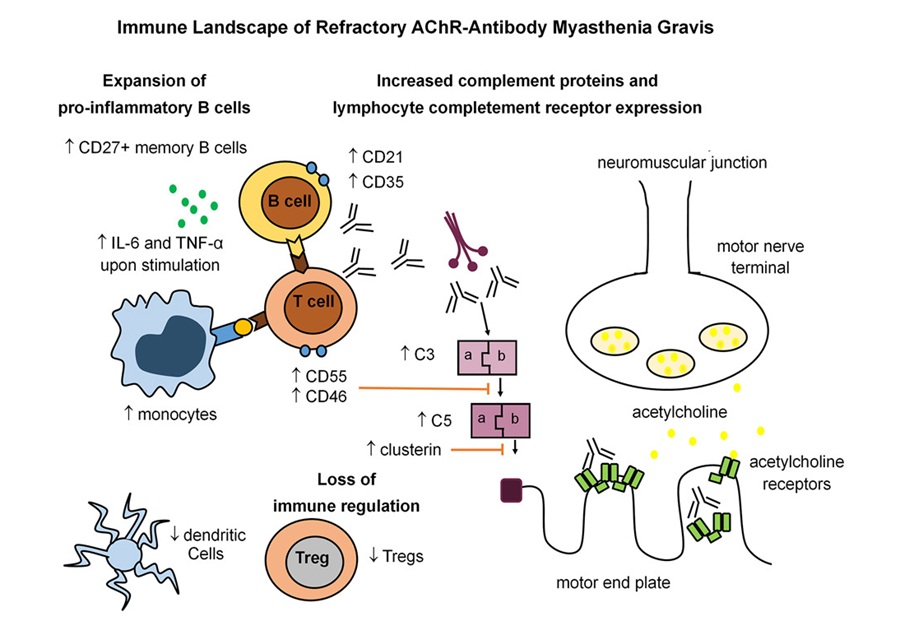
Immune Signature Identified in Treatment-Resistant Myasthenia Gravis
Myasthenia gravis is a rare autoimmune disorder in which immune attack at the neuromuscular junction causes fluctuating weakness that can impair vision, movement, speech, swallowing, and breathing.... Read more
New Biomarker Predicts Chemotherapy Response in Triple-Negative Breast Cancer
Triple-negative breast cancer is an aggressive form of breast cancer in which patients often show widely varying responses to chemotherapy. Predicting who will benefit from treatment remains challenging,... Read moreBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read morePathology
view channel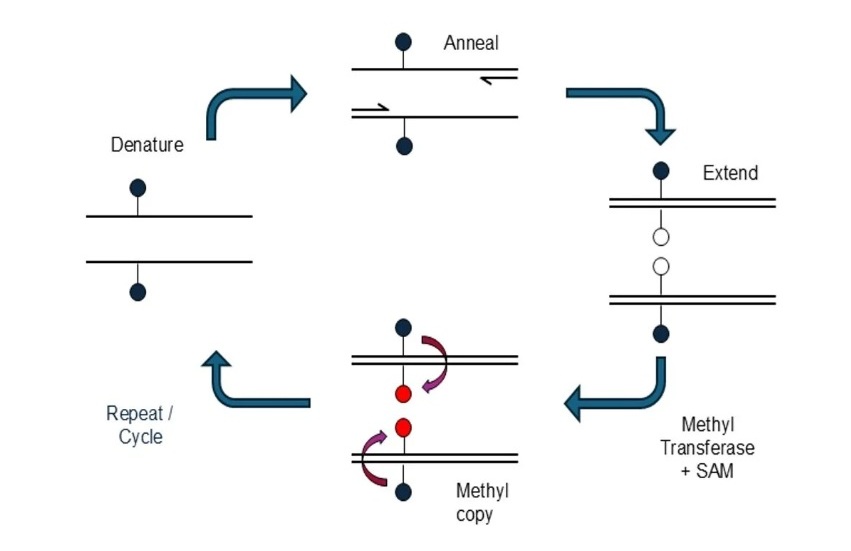
Novel mcPCR Technology to Transform Testing of Clinical Samples
DNA methylation is an important biological marker used in the diagnosis and monitoring of many diseases, including cancer. These chemical modifications to DNA influence gene activity and can reveal early... Read more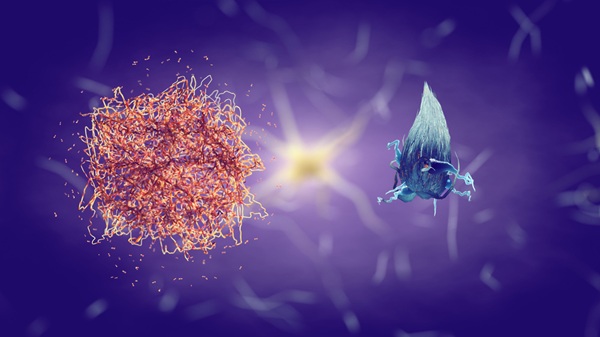
Sex Differences in Alzheimer’s Biomarkers Linked to Faster Cognitive Decline
Sex differences in Alzheimer’s disease present ongoing diagnostic challenges, with women often experiencing a disproportionate disease burden even when preclinical amyloid-beta levels are similar to men.... Read moreTechnology
view channel
AI Model Outperforms Clinicians in Rare Disease Detection
Rare diseases affect an estimated 300 million people worldwide, yet diagnosis is often protracted and error-prone. Many conditions present with heterogeneous signs that overlap with common disorders, leading... Read more
AI-Driven Diagnostic Demonstrates High Accuracy in Detecting Periprosthetic Joint Infection
Periprosthetic joint infection (PJI) is a rare but serious complication affecting 1% to 2% of primary joint replacement surgeries. The condition occurs when bacteria or fungi infect tissues around an implanted... Read moreIndustry
view channel
MGI Tech Strengthens Sequencing Portfolio with Dual Acquisition
MGI Tech Co., Ltd. (Shenzhen, China) announced the acquisition of STOmics and CycloneSEQ on March 3, 2026, as part of its “SEQALL+GLI+Omics” strategy. According to the company, the combined portfolio spans... Read more
Agilent Technologies Acquires Pathology Diagnostics Company Biocare Medical
Agilent Technologies (Santa Clara, CA, USA) has entered into a definitive agreement to acquire Biocare Medical (Pacheco, CA, USA), expanding its pathology portfolio through the addition of highly complementary... Read more