Screening Test Evaluated for Early Detection of Ovarian Cancer
|
By LabMedica International staff writers Posted on 23 Sep 2013 |
Image: Cancer antigen 125 (CA-125) enzyme-linked immunosorbent assay kit (Photo courtesy of Alibaba Group).
A protein that has long been recognized for predicting ovarian cancer recurrence now shows promise as a screening tool for the initial phases of the disease.
The simple blood test could offer a much-needed screening tool to detect ovarian cancer in its early stages, even in the most aggressive forms, in postmenopausal women at average risk for the disease.
Scientists at the MD Anderson Cancer Center (Houston, TX, USA) collaborating with other institutions, enrolled 4,051 women from seven sites across the USA, for a prospective, single-arm, 11-year study. All were healthy, postmenopausal women, ages 50 to 74 years, with no strong family history of breast or ovarian cancer. The study’s primary endpoint was specificity, or few false positives. In addition, the study looked at the positive predictive value, or the number of operations required to detect a case of ovarian cancer.
Each woman received a baseline cancer antigen 125 (CA-125) blood test. The Risk of Ovarian Cancer Algorithm (ROCA) was used as a mathematical model based on the patient’s age and CA-125 score. Women were stratified to one of three risks groups, with the respective follow-up: “low,” came back in a year for a follow-up blood test; “intermediate,” further monitoring with repeat CA-125 blood test in three months; and “high,” referred to receive transvaginal sonography (TVS) and to see a gynecologic oncologist.
The average annual rate of referral to a CA125 test in three months was 5.8%, and the average annual referral rate to TVS and review by a gynecologic oncologist was 0.9%. Ten women underwent surgery on the basis of TVS. Cumulatively, 117 women (2.9%) were determined to be high risk, providing a positive predictive value of 40% for detecting invasive ovarian cancer and the specificity was 99.9%.
Robert C. Bast, MD, the senior author of the study, said, “CA-125 is shed by only 80% of ovarian cancers. At present, we are planning a second trial that will evaluate a panel with four blood tests including CA-125 to detect the cancers we may otherwise miss with CA-125 alone. The current strategy is not perfect, but it appears to be a promising first step.” Prof. Bast, who co-invented the CA-125 assay, has worked closely with Fujirebio Diagnostics, Inc. (Malvern, PA, USA) to develop a clinical laboratory test. The study was published on August 26, 2013, in the journal Cancer.
Related Links:
MD Anderson Cancer Center
Fujirebio Diagnostics
The simple blood test could offer a much-needed screening tool to detect ovarian cancer in its early stages, even in the most aggressive forms, in postmenopausal women at average risk for the disease.
Scientists at the MD Anderson Cancer Center (Houston, TX, USA) collaborating with other institutions, enrolled 4,051 women from seven sites across the USA, for a prospective, single-arm, 11-year study. All were healthy, postmenopausal women, ages 50 to 74 years, with no strong family history of breast or ovarian cancer. The study’s primary endpoint was specificity, or few false positives. In addition, the study looked at the positive predictive value, or the number of operations required to detect a case of ovarian cancer.
Each woman received a baseline cancer antigen 125 (CA-125) blood test. The Risk of Ovarian Cancer Algorithm (ROCA) was used as a mathematical model based on the patient’s age and CA-125 score. Women were stratified to one of three risks groups, with the respective follow-up: “low,” came back in a year for a follow-up blood test; “intermediate,” further monitoring with repeat CA-125 blood test in three months; and “high,” referred to receive transvaginal sonography (TVS) and to see a gynecologic oncologist.
The average annual rate of referral to a CA125 test in three months was 5.8%, and the average annual referral rate to TVS and review by a gynecologic oncologist was 0.9%. Ten women underwent surgery on the basis of TVS. Cumulatively, 117 women (2.9%) were determined to be high risk, providing a positive predictive value of 40% for detecting invasive ovarian cancer and the specificity was 99.9%.
Robert C. Bast, MD, the senior author of the study, said, “CA-125 is shed by only 80% of ovarian cancers. At present, we are planning a second trial that will evaluate a panel with four blood tests including CA-125 to detect the cancers we may otherwise miss with CA-125 alone. The current strategy is not perfect, but it appears to be a promising first step.” Prof. Bast, who co-invented the CA-125 assay, has worked closely with Fujirebio Diagnostics, Inc. (Malvern, PA, USA) to develop a clinical laboratory test. The study was published on August 26, 2013, in the journal Cancer.
Related Links:
MD Anderson Cancer Center
Fujirebio Diagnostics
Latest Immunology News
- Blood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
- Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
- Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
- Blood Test Could Identify Colon Cancer Patients to Benefit from NSAIDs
- Blood Test Could Detect Adverse Immunotherapy Effects
- Routine Blood Test Can Predict Who Benefits Most from CAR T-Cell Therapy
- New Test Distinguishes Vaccine-Induced False Positives from Active HIV Infection
- Gene Signature Test Predicts Response to Key Breast Cancer Treatment
- Chip Captures Cancer Cells from Blood to Help Select Right Breast Cancer Treatment
- Blood-Based Liquid Biopsy Model Analyzes Immunotherapy Effectiveness
- Signature Genes Predict T-Cell Expansion in Cancer Immunotherapy
- Molecular Microscope Diagnostic System Assesses Lung Transplant Rejection
- Blood Test Tracks Treatment Resistance in High-Grade Serous Ovarian Cancer
- Luminescent Probe Measures Immune Cell Activity in Real Time
- Blood-Based Immune Cell Signatures Could Guide Treatment Decisions for Critically Ill Patients
- Novel Tool Predicts Most Effective Multiple Sclerosis Medication for Patients
Channels
Clinical Chemistry
view channel
New PSA-Based Prognostic Model Improves Prostate Cancer Risk Assessment
Prostate cancer is the second-leading cause of cancer death among American men, and about one in eight will be diagnosed in their lifetime. Screening relies on blood levels of prostate-specific antigen... Read more
Extracellular Vesicles Linked to Heart Failure Risk in CKD Patients
Chronic kidney disease (CKD) affects more than 1 in 7 Americans and is strongly associated with cardiovascular complications, which account for more than half of deaths among people with CKD.... Read moreMolecular Diagnostics
view channel
Diagnostic Device Predicts Treatment Response for Brain Tumors Via Blood Test
Glioblastoma is one of the deadliest forms of brain cancer, largely because doctors have no reliable way to determine whether treatments are working in real time. Assessing therapeutic response currently... Read more
Blood Test Detects Early-Stage Cancers by Measuring Epigenetic Instability
Early-stage cancers are notoriously difficult to detect because molecular changes are subtle and often missed by existing screening tools. Many liquid biopsies rely on measuring absolute DNA methylation... Read more
“Lab-On-A-Disc” Device Paves Way for More Automated Liquid Biopsies
Extracellular vesicles (EVs) are tiny particles released by cells into the bloodstream that carry molecular information about a cell’s condition, including whether it is cancerous. However, EVs are highly... Read more
Blood Test Identifies Inflammatory Breast Cancer Patients at Increased Risk of Brain Metastasis
Brain metastasis is a frequent and devastating complication in patients with inflammatory breast cancer, an aggressive subtype with limited treatment options. Despite its high incidence, the biological... Read moreHematology
view channel
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read more
Fast and Easy Test Could Revolutionize Blood Transfusions
Blood transfusions are a cornerstone of modern medicine, yet red blood cells can deteriorate quietly while sitting in cold storage for weeks. Although blood units have a fixed expiration date, cells from... Read more
Automated Hemostasis System Helps Labs of All Sizes Optimize Workflow
High-volume hemostasis sections must sustain rapid turnaround while managing reruns and reflex testing. Manual tube handling and preanalytical checks can strain staff time and increase opportunities for error.... Read more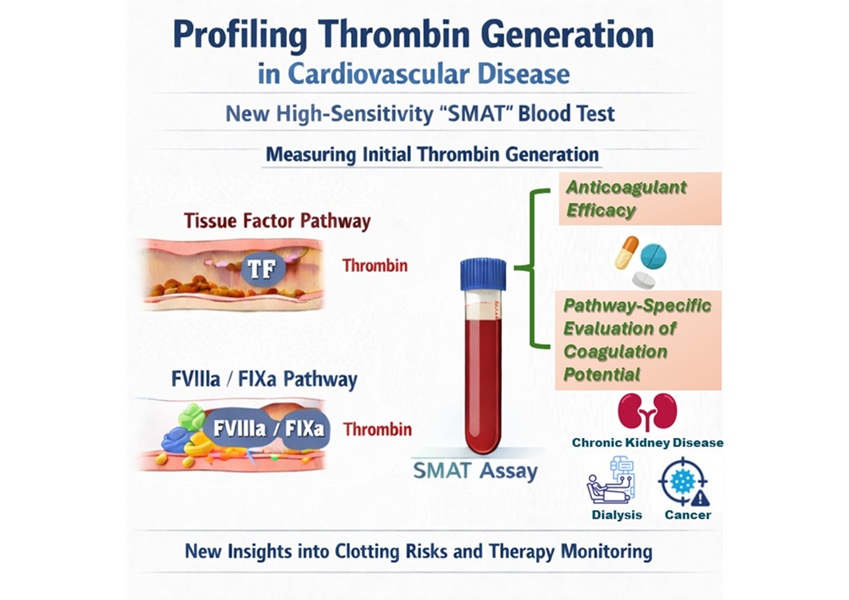
High-Sensitivity Blood Test Improves Assessment of Clotting Risk in Heart Disease Patients
Blood clotting is essential for preventing bleeding, but even small imbalances can lead to serious conditions such as thrombosis or dangerous hemorrhage. In cardiovascular disease, clinicians often struggle... Read moreMicrobiology
view channel
Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
Alzheimer’s disease affects approximately 6.7 million people in the United States and nearly 50 million worldwide, yet early cognitive decline remains difficult to characterize. Increasing evidence suggests... Read moreAI-Powered Platform Enables Rapid Detection of Drug-Resistant C. Auris Pathogens
Infections caused by the pathogenic yeast Candida auris pose a significant threat to hospitalized patients, particularly those with weakened immune systems or those who have invasive medical devices.... Read morePathology
view channel
Engineered Yeast Cells Enable Rapid Testing of Cancer Immunotherapy
Developing new cancer immunotherapies is a slow, costly, and high-risk process, particularly for CAR T cell treatments that must precisely recognize cancer-specific antigens. Small differences in tumor... Read more
First-Of-Its-Kind Test Identifies Autism Risk at Birth
Autism spectrum disorder is treatable, and extensive research shows that early intervention can significantly improve cognitive, social, and behavioral outcomes. Yet in the United States, the average age... Read moreTechnology
view channel
Robotic Technology Unveiled for Automated Diagnostic Blood Draws
Routine diagnostic blood collection is a high‑volume task that can strain staffing and introduce human‑dependent variability, with downstream implications for sample quality and patient experience.... Read more
ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
Clinical laboratories generate billions of test results each year, creating a treasure trove of data with the potential to support more personalized testing, improve operational efficiency, and enhance patient care.... Read moreAptamer Biosensor Technology to Transform Virus Detection
Rapid and reliable virus detection is essential for controlling outbreaks, from seasonal influenza to global pandemics such as COVID-19. Conventional diagnostic methods, including cell culture, antigen... Read more
AI Models Could Predict Pre-Eclampsia and Anemia Earlier Using Routine Blood Tests
Pre-eclampsia and anemia are major contributors to maternal and child mortality worldwide, together accounting for more than half a million deaths each year and leaving millions with long-term health complications.... Read moreIndustry
view channelNew Collaboration Brings Automated Mass Spectrometry to Routine Laboratory Testing
Mass spectrometry is a powerful analytical technique that identifies and quantifies molecules based on their mass and electrical charge. Its high selectivity, sensitivity, and accuracy make it indispensable... Read more
AI-Powered Cervical Cancer Test Set for Major Rollout in Latin America
Noul Co., a Korean company specializing in AI-based blood and cancer diagnostics, announced it will supply its intelligence (AI)-based miLab CER cervical cancer diagnostic solution to Mexico under a multi‑year... Read more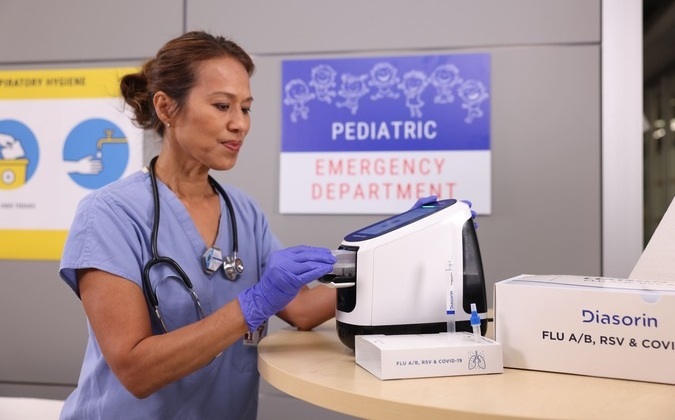
Diasorin and Fisher Scientific Enter into US Distribution Agreement for Molecular POC Platform
Diasorin (Saluggia, Italy) has entered into an exclusive distribution agreement with Fisher Scientific, part of Thermo Fisher Scientific (Waltham, MA, USA), for the LIAISON NES molecular point-of-care... Read more