Biomarkers Diagnose and Predict Acute Pancreatitis
|
By LabMedica International staff writers Posted on 08 Jul 2021 |
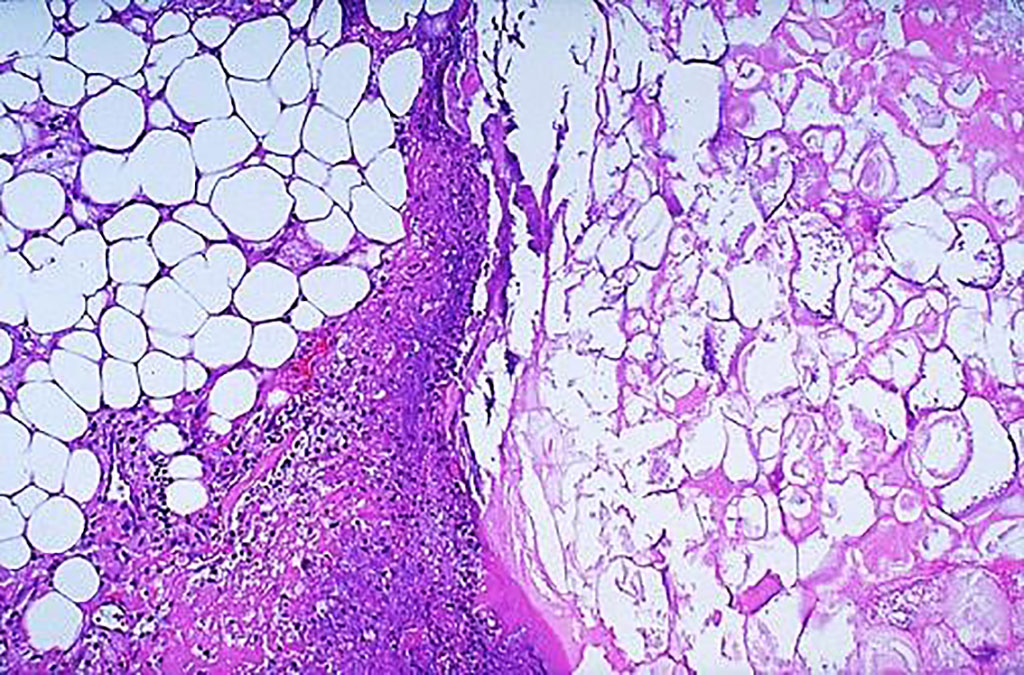
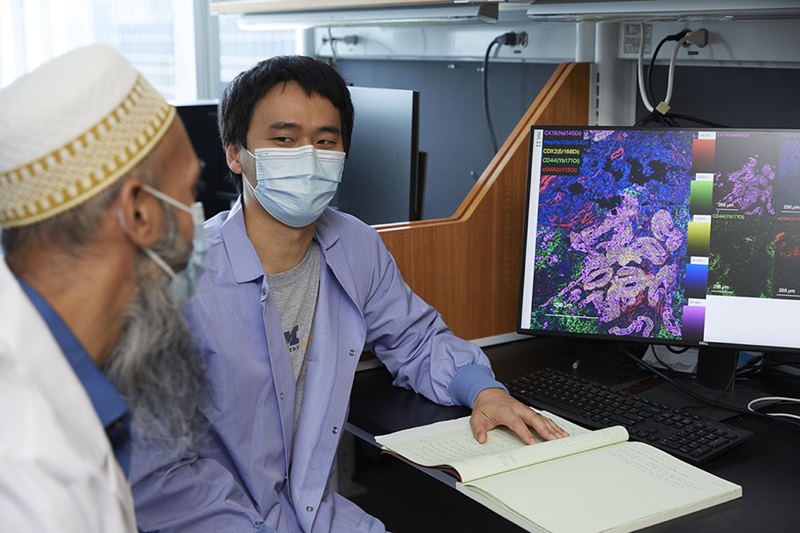
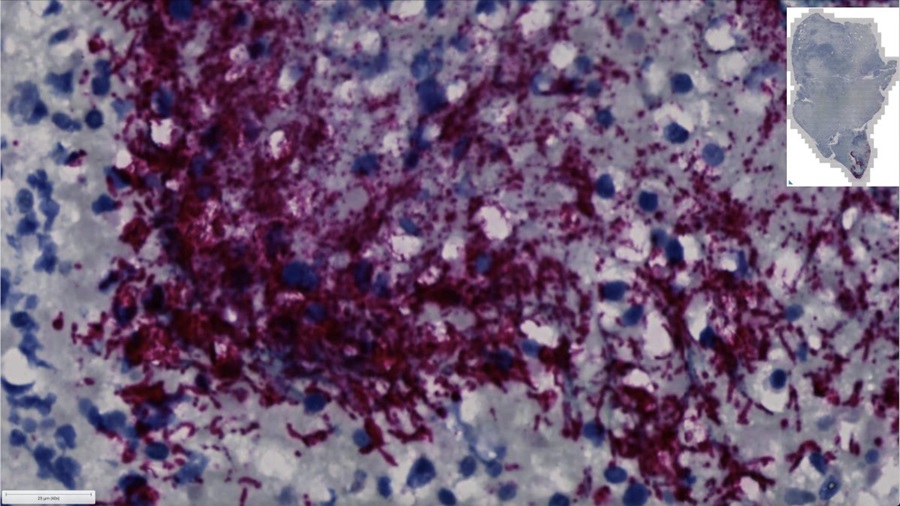
Image: Histology of acute pancreatitis. Microscopically, the fat necrosis consists of steatocytes (adipocytes) that have lost their nuclei and whose cytoplasm has a granular pink appearance as seen on the right. Some hemorrhage is seen at the left in this case of acute pancreatitis (Photo courtesy of Texas A&M University)
Acute pancreatitis (AP) is an inflammatory reaction caused by the activated pancreatic enzymes in the pancreas, which leads to subsequent pancreatic autodigestion, edema, hemorrhage, necrosis, and even distal organ dysfunction.
Conventional biomarkers such as amylase, lipase, C-reactive protein (CRP), and leukocytes are less specific in assessing the severity of AP. Control of the systemic inflammatory response is a key factor in the prognosis of AP; thus, pro-inflammatory markers can be mined as potential diagnostic and prognostic indicators of AP.
Clinical Laboratorians at the Zhejiang University School of Medicine (Hangzhou, China) included in a study 451 participants, including 343 AP patients and 108 healthy controls. According to the clinical outcome within 28 days, all patients were divided into the deceased group and survival group, while the survival group included four subgroups based on the clinical manifestations: pancreatic infection and necrosis, pancreatic tissue accumulation, extrapancreatic infection, and new-onset diabetes, some of which overlapped with each other.
Systemic inflammatory response syndrome (SIRS) score were evaluated for each patient within 24, 24, and 48 hours of admission, respectively. Laboratory indicators included were plasma levels of plasma procalcitonin (PCT), heparin-binding protein (HBP), and interleukin-6 (IL-6) on days 1, 3, 7, and 10 after admission for all patients in the study. Patient outcomes were recorded: death, infectious pancreatic necrosis, necrotic tissue accumulation, septic shock, new-onset diabetes, and extrapancreatic infection.
The investigators reported that a statistically significant increase in the mean plasma analyte levels was detected in the study group compared to the control group. Multivariate comparison showed that plasma levels of PCT, HBP, and IL-6 were all significantly different among the three groups at different sampling times (1st, 3rd, 7th, and 10th day of admission). The combination of the three indicators had significantly higher diagnostic value than either the individual markers or pairwise combinations. The levels of the three were all significantly higher in severe acute pancreatitis (SAP) patients than in non-SAP patients. The patients with high levels had a worse prognosis than those with low levels.
The authors concluded that the combined detection of plasma PCT, HBP, and IL-6 provided a new idea for the diagnosis of patients with AP; increased concentrations of PCT, HBP, or IL-6 within three days of admission were associated with AP severity and poor prognosis; high concentrations of PCT, HBP, or IL-6 may be the useful predictors of SAP and the independent risk factors for AP. The study was published on June 21, 2021 in the Journal of Clinical Laboratory Analysis.
Related Links:
Zhejiang University School of Medicine
Conventional biomarkers such as amylase, lipase, C-reactive protein (CRP), and leukocytes are less specific in assessing the severity of AP. Control of the systemic inflammatory response is a key factor in the prognosis of AP; thus, pro-inflammatory markers can be mined as potential diagnostic and prognostic indicators of AP.
Clinical Laboratorians at the Zhejiang University School of Medicine (Hangzhou, China) included in a study 451 participants, including 343 AP patients and 108 healthy controls. According to the clinical outcome within 28 days, all patients were divided into the deceased group and survival group, while the survival group included four subgroups based on the clinical manifestations: pancreatic infection and necrosis, pancreatic tissue accumulation, extrapancreatic infection, and new-onset diabetes, some of which overlapped with each other.
Systemic inflammatory response syndrome (SIRS) score were evaluated for each patient within 24, 24, and 48 hours of admission, respectively. Laboratory indicators included were plasma levels of plasma procalcitonin (PCT), heparin-binding protein (HBP), and interleukin-6 (IL-6) on days 1, 3, 7, and 10 after admission for all patients in the study. Patient outcomes were recorded: death, infectious pancreatic necrosis, necrotic tissue accumulation, septic shock, new-onset diabetes, and extrapancreatic infection.
The investigators reported that a statistically significant increase in the mean plasma analyte levels was detected in the study group compared to the control group. Multivariate comparison showed that plasma levels of PCT, HBP, and IL-6 were all significantly different among the three groups at different sampling times (1st, 3rd, 7th, and 10th day of admission). The combination of the three indicators had significantly higher diagnostic value than either the individual markers or pairwise combinations. The levels of the three were all significantly higher in severe acute pancreatitis (SAP) patients than in non-SAP patients. The patients with high levels had a worse prognosis than those with low levels.
The authors concluded that the combined detection of plasma PCT, HBP, and IL-6 provided a new idea for the diagnosis of patients with AP; increased concentrations of PCT, HBP, or IL-6 within three days of admission were associated with AP severity and poor prognosis; high concentrations of PCT, HBP, or IL-6 may be the useful predictors of SAP and the independent risk factors for AP. The study was published on June 21, 2021 in the Journal of Clinical Laboratory Analysis.
Related Links:
Zhejiang University School of Medicine
Latest Clinical Chem. News
- 3D Printed Point-Of-Care Mass Spectrometer Outperforms State-Of-The-Art Models
- POC Biomedical Test Spins Water Droplet Using Sound Waves for Cancer Detection
- Highly Reliable Cell-Based Assay Enables Accurate Diagnosis of Endocrine Diseases
- New Blood Testing Method Detects Potent Opioids in Under Three Minutes
- Wireless Hepatitis B Test Kit Completes Screening and Data Collection in One Step
- Pain-Free, Low-Cost, Sensitive, Radiation-Free Device Detects Breast Cancer in Urine
- Spit Test Detects Breast Cancer in Five Seconds
- Electrochemical Sensors with Next-Generation Coating Advances Precision Diagnostics at POC
- First-Of-Its-Kind Handheld Device Accurately Detects Fentanyl in Urine within Seconds
- New Fluorescent Sensor Array Lights up Alzheimer’s-Related Proteins for Earlier Detection
- Automated Mass Spectrometry-Based Clinical Analyzer Could Transform Lab Testing
- Highly Sensitive pH Sensor to Aid Detection of Cancers and Vector-Borne Viruses
- Non-Invasive Sensor Monitors Changes in Saliva Compositions to Rapidly Diagnose Diabetes
- Breakthrough Immunoassays to Aid in Risk Assessment of Preeclampsia
- Urine Test for Monitoring Changes in Kidney Health Markers Can Predict New-Onset Heart Failure
- AACC Releases Comprehensive Diabetes Testing Guidelines
Channels
Molecular Diagnostics
view channel
Blood Test Accurately Predicts Lung Cancer Risk and Reduces Need for Scans
Lung cancer is extremely hard to detect early due to the limitations of current screening technologies, which are costly, sometimes inaccurate, and less commonly endorsed by healthcare professionals compared... Read more
Unique Autoantibody Signature to Help Diagnose Multiple Sclerosis Years before Symptom Onset
Autoimmune diseases such as multiple sclerosis (MS) are thought to occur partly due to unusual immune responses to common infections. Early MS symptoms, including dizziness, spasms, and fatigue, often... Read more
Blood Test Could Detect HPV-Associated Cancers 10 Years before Clinical Diagnosis
Human papilloma virus (HPV) is known to cause various cancers, including those of the genitals, anus, mouth, throat, and cervix. HPV-associated oropharyngeal cancer (HPV+OPSCC) is the most common HPV-associated... Read moreHematology
view channel
Next Generation Instrument Screens for Hemoglobin Disorders in Newborns
Hemoglobinopathies, the most widespread inherited conditions globally, affect about 7% of the population as carriers, with 2.7% of newborns being born with these conditions. The spectrum of clinical manifestations... Read more
First 4-in-1 Nucleic Acid Test for Arbovirus Screening to Reduce Risk of Transfusion-Transmitted Infections
Arboviruses represent an emerging global health threat, exacerbated by climate change and increased international travel that is facilitating their spread across new regions. Chikungunya, dengue, West... Read more
POC Finger-Prick Blood Test Determines Risk of Neutropenic Sepsis in Patients Undergoing Chemotherapy
Neutropenia, a decrease in neutrophils (a type of white blood cell crucial for fighting infections), is a frequent side effect of certain cancer treatments. This condition elevates the risk of infections,... Read more
First Affordable and Rapid Test for Beta Thalassemia Demonstrates 99% Diagnostic Accuracy
Hemoglobin disorders rank as some of the most prevalent monogenic diseases globally. Among various hemoglobin disorders, beta thalassemia, a hereditary blood disorder, affects about 1.5% of the world's... Read moreImmunology
view channel
Diagnostic Blood Test for Cellular Rejection after Organ Transplant Could Replace Surgical Biopsies
Transplanted organs constantly face the risk of being rejected by the recipient's immune system which differentiates self from non-self using T cells and B cells. T cells are commonly associated with acute... Read more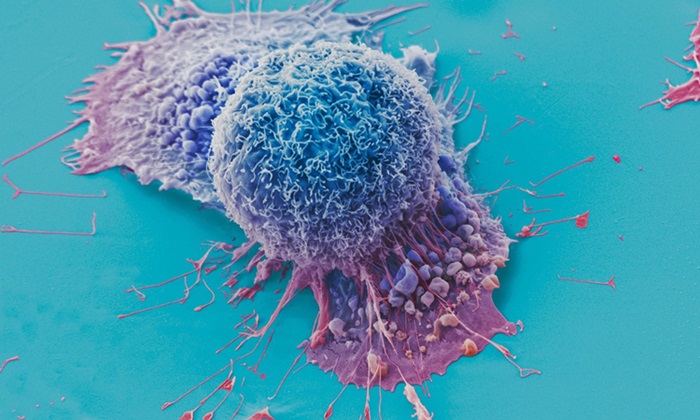
AI Tool Precisely Matches Cancer Drugs to Patients Using Information from Each Tumor Cell
Current strategies for matching cancer patients with specific treatments often depend on bulk sequencing of tumor DNA and RNA, which provides an average profile from all cells within a tumor sample.... Read more
Genetic Testing Combined With Personalized Drug Screening On Tumor Samples to Revolutionize Cancer Treatment
Cancer treatment typically adheres to a standard of care—established, statistically validated regimens that are effective for the majority of patients. However, the disease’s inherent variability means... Read moreMicrobiology
view channel
New CE-Marked Hepatitis Assays to Help Diagnose Infections Earlier
According to the World Health Organization (WHO), an estimated 354 million individuals globally are afflicted with chronic hepatitis B or C. These viruses are the leading causes of liver cirrhosis, liver... Read more
1 Hour, Direct-From-Blood Multiplex PCR Test Identifies 95% of Sepsis-Causing Pathogens
Sepsis contributes to one in every three hospital deaths in the US, and globally, septic shock carries a mortality rate of 30-40%. Diagnosing sepsis early is challenging due to its non-specific symptoms... Read morePathology
view channelAI-Powered Digital Imaging System to Revolutionize Cancer Diagnosis
The process of biopsy is important for confirming the presence of cancer. In the conventional histopathology technique, tissue is excised, sliced, stained, mounted on slides, and examined under a microscope... Read more
New Mycobacterium Tuberculosis Panel to Support Real-Time Surveillance and Combat Antimicrobial Resistance
Tuberculosis (TB), the leading cause of death from an infectious disease globally, is a contagious bacterial infection that primarily spreads through the coughing of patients with active pulmonary TB.... Read moreTechnology
view channel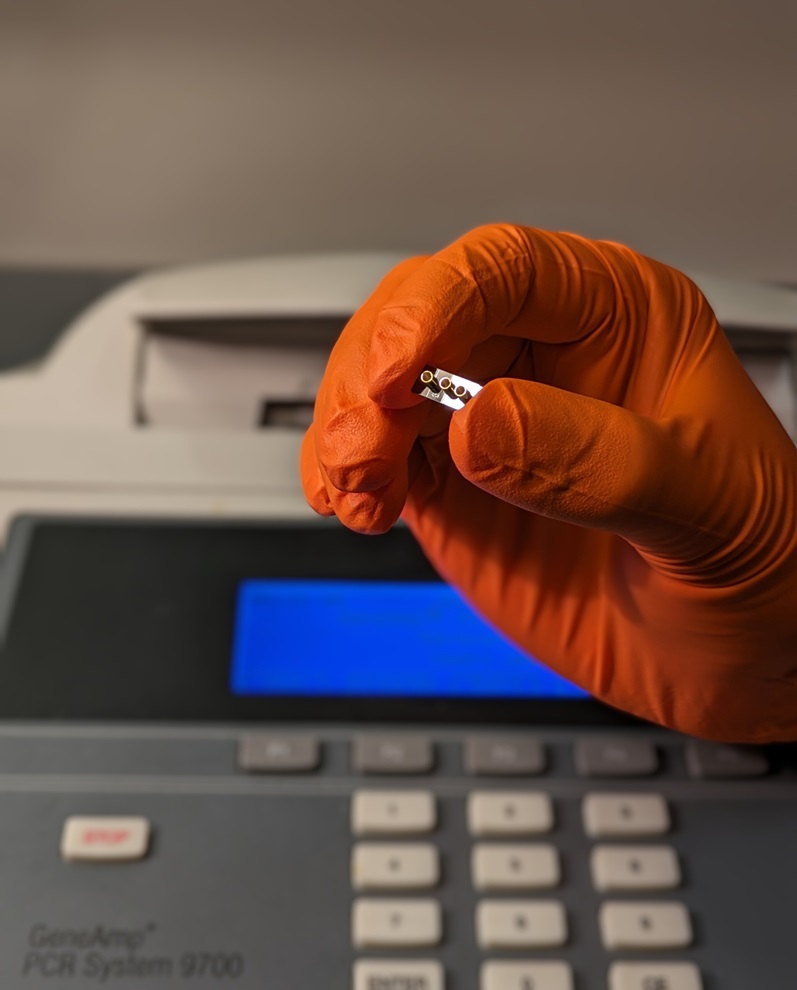
New Diagnostic System Achieves PCR Testing Accuracy
While PCR tests are the gold standard of accuracy for virology testing, they come with limitations such as complexity, the need for skilled lab operators, and longer result times. They also require complex... Read more
DNA Biosensor Enables Early Diagnosis of Cervical Cancer
Molybdenum disulfide (MoS2), recognized for its potential to form two-dimensional nanosheets like graphene, is a material that's increasingly catching the eye of the scientific community.... Read more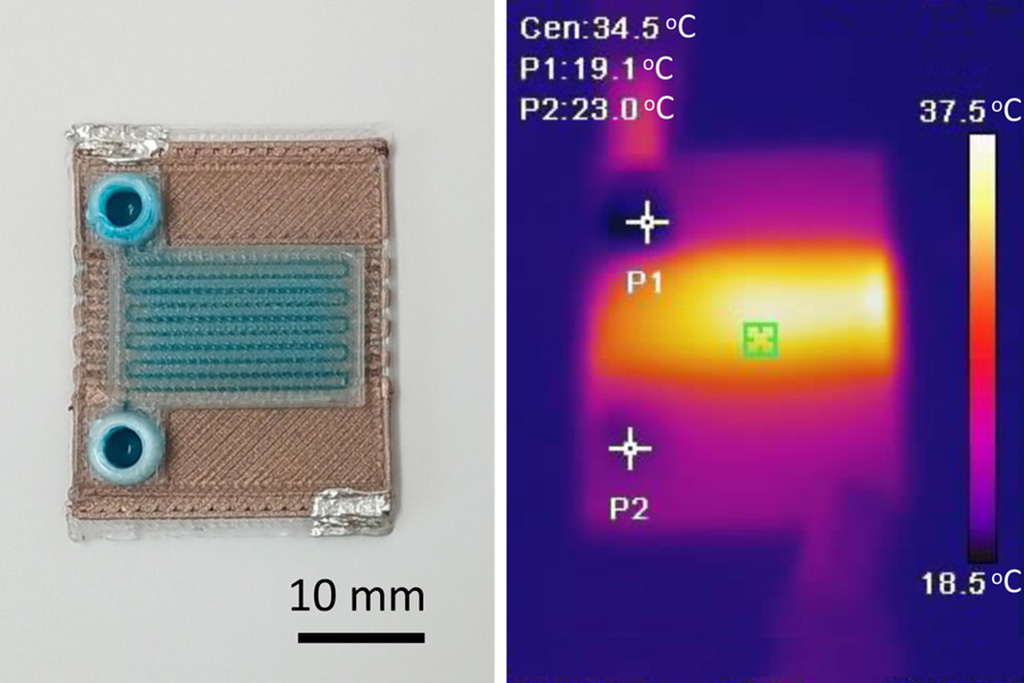
Self-Heating Microfluidic Devices Can Detect Diseases in Tiny Blood or Fluid Samples
Microfluidics, which are miniature devices that control the flow of liquids and facilitate chemical reactions, play a key role in disease detection from small samples of blood or other fluids.... Read more
Breakthrough in Diagnostic Technology Could Make On-The-Spot Testing Widely Accessible
Home testing gained significant importance during the COVID-19 pandemic, yet the availability of rapid tests is limited, and most of them can only drive one liquid across the strip, leading to continued... Read moreIndustry
view channel
ECCMID Congress Name Changes to ESCMID Global
Over the last few years, the European Society of Clinical Microbiology and Infectious Diseases (ESCMID, Basel, Switzerland) has evolved remarkably. The society is now stronger and broader than ever before... Read more
Bosch and Randox Partner to Make Strategic Investment in Vivalytic Analysis Platform
Given the presence of so many diseases, determining whether a patient is presenting the symptoms of a simple cold, the flu, or something as severe as life-threatening meningitis is usually only possible... Read more
Siemens to Close Fast Track Diagnostics Business
Siemens Healthineers (Erlangen, Germany) has announced its intention to close its Fast Track Diagnostics unit, a small collection of polymerase chain reaction (PCR) testing products that is part of the... Read more












.jpg)