Unique Antibody Profile Differentiates Gluten Sensitivity from Celiac Disease
|
By LabMedica International staff writers Posted on 17 Sep 2020 |
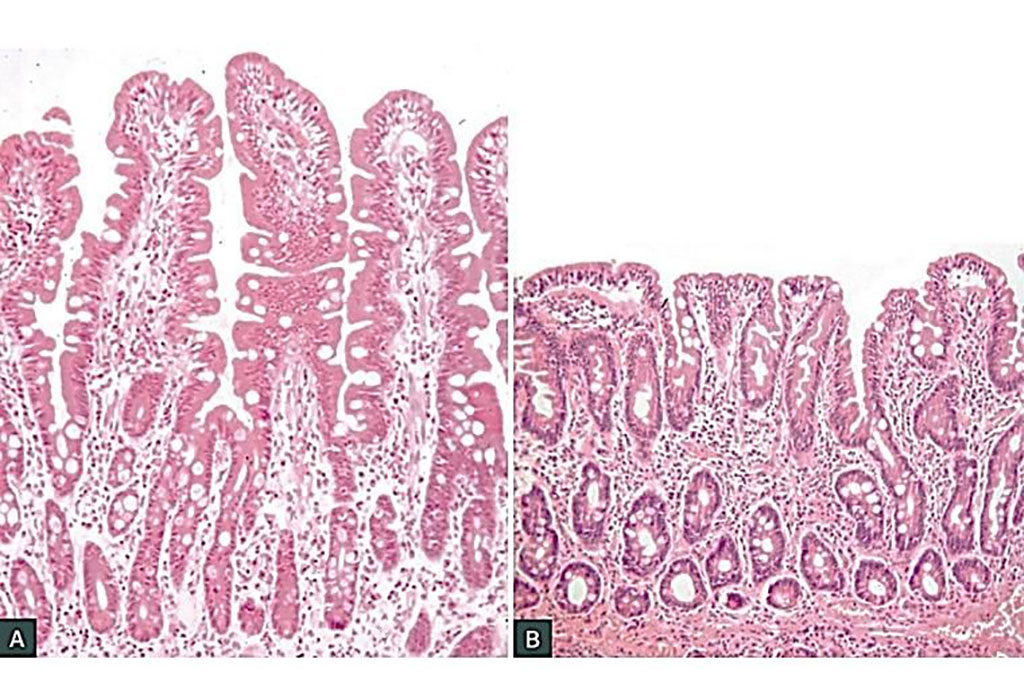
Image: Histology of normal small intestinal mucosa in adequately treated celiac disease (A). Untreated coeliac disease shows the classic triad of infiltration of the epithelium with lymphocytes, crypt hyperplasia and villous atrophy (B) (Photo courtesy of Professor Jason Tye-Din, MBBS PhD).
Until recently, many doctors often dismissed the complaints of people who claimed to be sensitive to foods containing gluten but did not have celiac disease, a well-documented autoimmune disease triggered by exposure to the dietary protein found in wheat, rye, and barley.
Celiac disease (CD) is an autoimmune enteropathy triggered by exposure to gluten proteins, leading to intestinal inflammation and villous atrophy in genetically predisposed individuals. It is associated with robust B cell and antibody responses to gluten and to the transglutaminase 2 (TG2) autoantigen.
A team of scientists from various institutions and led by those at the Columbia University Medical Center (New York, NY, USA) analyzed blood samples from 40 patients with celiac disease, 80 patients with non-celiac gluten sensitivity (NCGS), and 40 healthy controls, all of whom consumed an unrestricted, gluten-containing diet. The most common gastrointestinal symptoms included bloating, abdominal pain, diarrhea, nausea, and heartburn, while the most prominent extra-intestinal symptoms were fatigue, headache, anxiety, cognitive difficulties, and numbness in arms and legs.
Serum levels of total IgG reactivity to gluten and individual IgG subclass reactivities to gluten were measured separately by an enzyme-linked immunosorbent assay (ELISA). Serum levels of intestinal fatty acid-binding protein (FABP2) were also measured. FABP2 is a cytosolic protein specific to intestinal epithelial cells that is released into systemic circulation upon cellular damage. The team measured IgA antibody to recombinant human TG2, a sensitive and specific serologic marker for CD. The investigators performed HLA genotyping to assess CD genetic predisposition.
The scientists reported that the anti-gliadin IgG response in CD patients was comprised primarily of IgG1 and IgG3, which were significantly increased in comparison with the healthy and NCGS cohorts. There was a modest elevation in anti-gliadin IgG2 compared with the healthy group and no comparative increase in the IgG4 subclass. Within the NCGS cohort, however, the lower contributions of anti-gliadin IgG1 and IgG3 in comparison with CD was compensated by significantly elevated IgG4 (compared with CD and healthy cohorts) and IgG2 (compared with healthy cohort). Serum concentrations of intestinal fatty acid-binding protein (FABP2), a specific marker of intestinal epithelial cell damage, were similarly elevated in the CD and NCGS groups in comparison with healthy cohort.
Armin Alaedini, PhD, an assistant professor of medicine and a senior author of the study, said, “We found that the B cells of celiac disease patients produced a subclass profile of IgG antibodies with a strong inflammatory potential that is linked to autoimmune activity and intestinal cell damage. In contrast, the patients with non-celiac gluten sensitivity produced IgG antibodies that are associated with a more restrained inflammatory response.” The study was published online July 21, 2020 in the journal Gastroenterology.
Related Links:
Columbia University Medical Center
Celiac disease (CD) is an autoimmune enteropathy triggered by exposure to gluten proteins, leading to intestinal inflammation and villous atrophy in genetically predisposed individuals. It is associated with robust B cell and antibody responses to gluten and to the transglutaminase 2 (TG2) autoantigen.
A team of scientists from various institutions and led by those at the Columbia University Medical Center (New York, NY, USA) analyzed blood samples from 40 patients with celiac disease, 80 patients with non-celiac gluten sensitivity (NCGS), and 40 healthy controls, all of whom consumed an unrestricted, gluten-containing diet. The most common gastrointestinal symptoms included bloating, abdominal pain, diarrhea, nausea, and heartburn, while the most prominent extra-intestinal symptoms were fatigue, headache, anxiety, cognitive difficulties, and numbness in arms and legs.
Serum levels of total IgG reactivity to gluten and individual IgG subclass reactivities to gluten were measured separately by an enzyme-linked immunosorbent assay (ELISA). Serum levels of intestinal fatty acid-binding protein (FABP2) were also measured. FABP2 is a cytosolic protein specific to intestinal epithelial cells that is released into systemic circulation upon cellular damage. The team measured IgA antibody to recombinant human TG2, a sensitive and specific serologic marker for CD. The investigators performed HLA genotyping to assess CD genetic predisposition.
The scientists reported that the anti-gliadin IgG response in CD patients was comprised primarily of IgG1 and IgG3, which were significantly increased in comparison with the healthy and NCGS cohorts. There was a modest elevation in anti-gliadin IgG2 compared with the healthy group and no comparative increase in the IgG4 subclass. Within the NCGS cohort, however, the lower contributions of anti-gliadin IgG1 and IgG3 in comparison with CD was compensated by significantly elevated IgG4 (compared with CD and healthy cohorts) and IgG2 (compared with healthy cohort). Serum concentrations of intestinal fatty acid-binding protein (FABP2), a specific marker of intestinal epithelial cell damage, were similarly elevated in the CD and NCGS groups in comparison with healthy cohort.
Armin Alaedini, PhD, an assistant professor of medicine and a senior author of the study, said, “We found that the B cells of celiac disease patients produced a subclass profile of IgG antibodies with a strong inflammatory potential that is linked to autoimmune activity and intestinal cell damage. In contrast, the patients with non-celiac gluten sensitivity produced IgG antibodies that are associated with a more restrained inflammatory response.” The study was published online July 21, 2020 in the journal Gastroenterology.
Related Links:
Columbia University Medical Center
Latest Immunology News
- New Biomarker Predicts Chemotherapy Response in Triple-Negative Breast Cancer
- Blood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
- Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
- Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
- Blood Test Could Identify Colon Cancer Patients to Benefit from NSAIDs
- Blood Test Could Detect Adverse Immunotherapy Effects
- Routine Blood Test Can Predict Who Benefits Most from CAR T-Cell Therapy
- New Test Distinguishes Vaccine-Induced False Positives from Active HIV Infection
- Gene Signature Test Predicts Response to Key Breast Cancer Treatment
- Chip Captures Cancer Cells from Blood to Help Select Right Breast Cancer Treatment
- Blood-Based Liquid Biopsy Model Analyzes Immunotherapy Effectiveness
- Signature Genes Predict T-Cell Expansion in Cancer Immunotherapy
- Molecular Microscope Diagnostic System Assesses Lung Transplant Rejection
- Blood Test Tracks Treatment Resistance in High-Grade Serous Ovarian Cancer
- Luminescent Probe Measures Immune Cell Activity in Real Time
- Blood-Based Immune Cell Signatures Could Guide Treatment Decisions for Critically Ill Patients
Channels
Clinical Chemistry
view channel
Simple Blood Test Offers New Path to Alzheimer’s Assessment in Primary Care
Timely evaluation of cognitive symptoms in primary care is often limited by restricted access to specialized diagnostics and invasive confirmatory procedures. Clinicians need accessible tools to determine... Read more
Existing Hospital Analyzers Can Identify Fake Liquid Medical Products
Counterfeit and substandard medicines remain a serious global health threat, with World Health Organization estimates suggesting that 10.5% of medicines in low- and middle-income countries are either fake... Read moreMolecular Diagnostics
view channel
New Genome Sequencing Technique Measures Epstein-Barr Virus in Blood
The Epstein–Barr virus (EBV) infects up to 95% of adults worldwide and remains in the body for life. While usually kept under control, the virus is linked to cancers such as Hodgkin’s lymphoma and autoimmune... Read more
Blood Test Boosts Early Detection of Brain Cancer
Brain and central nervous system (CNS) tumors are often diagnosed at an advanced stage, when treatment options are limited, and survival rates remain low. Around 300,000 new cases are diagnosed each year... Read moreHematology
view channel
Rapid Cartridge-Based Test Aims to Expand Access to Hemoglobin Disorder Diagnosis
Sickle cell disease and beta thalassemia are hemoglobin disorders that often require referral to specialized laboratories for definitive diagnosis, delaying results for patients and clinicians.... Read more
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read moreMicrobiology
view channel
Three-Test Panel Launched for Detection of Liver Fluke Infections
Parasitic liver fluke infections remain endemic in parts of Asia, where transmission commonly occurs through consumption of raw freshwater fish or aquatic plants. Chronic infection is a well-established... Read more
Rapid Test Promises Faster Answers for Drug-Resistant Infections
Drug-resistant pathogens continue to pose a growing threat in healthcare facilities, where delayed detection can impede outbreak control and increase mortality. Candida auris is notoriously difficult to... Read more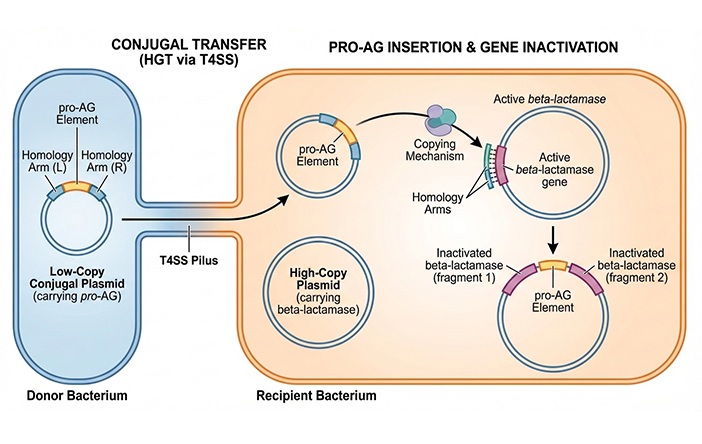
CRISPR-Based Technology Neutralizes Antibiotic-Resistant Bacteria
Antibiotic resistance has accelerated into a global health crisis, with projections estimating more than 10 million deaths per year by 2050 as drug-resistant “superbugs” continue to spread.... Read more
Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
Alzheimer’s disease affects approximately 6.7 million people in the United States and nearly 50 million worldwide, yet early cognitive decline remains difficult to characterize. Increasing evidence suggests... Read morePathology
view channel
Single Sample Classifier Predicts Cancer-Associated Fibroblast Subtypes in Patient Samples
Pancreatic ductal adenocarcinoma (PDAC) remains one of the deadliest cancers, in part because of its dense tumor microenvironment that influences how tumors grow and respond to treatment.... Read more
New AI-Driven Platform Standardizes Tuberculosis Smear Microscopy Workflow
Sputum smear microscopy remains central to tuberculosis treatment monitoring and follow-up, particularly in high‑burden settings where serial testing is routine. Yet consistent, repeatable bacillary assessment... Read more
AI Tool Uses Blood Biomarkers to Predict Transplant Complications Before Symptoms Appear
Stem cell and bone marrow transplants can be lifesaving, but serious complications may arise months after patients leave the hospital. One of the most dangerous is chronic graft-versus-host disease, in... Read moreTechnology
view channel
Blood Test “Clocks” Predict Start of Alzheimer’s Symptoms
More than 7 million Americans live with Alzheimer’s disease, and related health and long-term care costs are projected to reach nearly USD 400 billion in 2025. The disease has no cure, and symptoms often... Read more
AI-Powered Biomarker Predicts Liver Cancer Risk
Liver cancer, or hepatocellular carcinoma, causes more than 800,000 deaths worldwide each year and often goes undetected until late stages. Even after treatment, recurrence rates reach 70% to 80%, contributing... Read more
Robotic Technology Unveiled for Automated Diagnostic Blood Draws
Routine diagnostic blood collection is a high‑volume task that can strain staffing and introduce human‑dependent variability, with downstream implications for sample quality and patient experience.... Read more
ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
Clinical laboratories generate billions of test results each year, creating a treasure trove of data with the potential to support more personalized testing, improve operational efficiency, and enhance patient care.... Read moreIndustry
view channel
QuidelOrtho Collaborates with Lifotronic to Expand Global Immunoassay Portfolio
QuidelOrtho (San Diego, CA, USA) has entered a long-term strategic supply agreement with Lifotronic Technology (Shenzhen, China) to expand its global immunoassay portfolio and accelerate customer access... Read more