High-Res Genotyping Improves Survival for Stem Cell Transplantation
|
By LabMedica International staff writers Posted on 25 Apr 2019 |

Image: The PacBio RS II sequencer uses single molecule, real time (SMRT) sequencing technology (Photo courtesy of Pacific Biosciences).
Allogeneic hematopoietic cell transplantation (HCT) provides a curative treatment option for individuals with hematologic diseases. Recipients and donors are considered to be compatible or “well matched” if they share a high degree of genetic similarity at their human leukocyte antigen (HLA) loci.
HCT was limited to using HLA-identical related donors. Improved knowledge of the transplant process and therapeutic drug development, coupled with increased resolution of HLA typing and a significantly larger pool of volunteer unrelated donors (VUDs) worldwide, has meant that HCT with a VUD now offers comparable survival.
A team of scientists working with the Anthony Nolan Research Institute (London, UK) carried out a large retrospective study consisting of VUD–recipient HCT pairs transplanted between 1996 and 2011. The cohort comprised 891 adult and pediatric patients with hematologic malignancies from 32 UK allogeneic centers were included. Primary outcomes included overall survival (OS), non-relapse mortality (NRM), disease relapse, and acute graft-versus-host disease (aGVHD). Reporting of chronic GVHD follow-up data were insufficient to perform this analysis.
The team used methods of DNA-based HLA typing used previously included sequence specific oligonucleotide probing, Sanger sequencing-based typing, and reference strand-mediated conformational analysis. Retrospective UHR HLA typing of the cohort was performed for the six classic HLA loci using Pacific Biosciences Single Molecule Real-Time sequencing. To determine if there were viable alternatives to a 12/12 ultra-high resolution (UHR) HLA match, they chose to test the HLA-DPB1 T cell epitope (TCE) model of permissible mismatching in this data set.
The scientists reported that of 891 bone marrow donors and their respective, they found that when patients were matched at 12 alleles across six HLA genes, five-year survival was 55% compared to 40% for patients with any degree of mismatch. In addition, they found that 29% of patients who were previously thought to be matched via HLA typing methods that included Sanger sequencing and sequencing-specific oligonucleotide probing, actually had at least one mismatch when they were retrospectively analyzed using long-read sequencing on the Pacific Biosciences RS II platform. And, five-year survival among these patients was also lower at 30%.
Neema P Mayor, PhD, Head of Immunogenetics and lead author of the study, said, “We thought all of these individuals had been well matched, but they were not as well-matched as we had previously thought. Then, when the team analyzed the outcomes, they found that the individuals with mismatches that we didn't know about did significantly worse.” The study was published in the March 2019 issue of the journal Biology of Blood and Marrow Transplantation.
Related Links:
Anthony Nolan Research Institute
HCT was limited to using HLA-identical related donors. Improved knowledge of the transplant process and therapeutic drug development, coupled with increased resolution of HLA typing and a significantly larger pool of volunteer unrelated donors (VUDs) worldwide, has meant that HCT with a VUD now offers comparable survival.
A team of scientists working with the Anthony Nolan Research Institute (London, UK) carried out a large retrospective study consisting of VUD–recipient HCT pairs transplanted between 1996 and 2011. The cohort comprised 891 adult and pediatric patients with hematologic malignancies from 32 UK allogeneic centers were included. Primary outcomes included overall survival (OS), non-relapse mortality (NRM), disease relapse, and acute graft-versus-host disease (aGVHD). Reporting of chronic GVHD follow-up data were insufficient to perform this analysis.
The team used methods of DNA-based HLA typing used previously included sequence specific oligonucleotide probing, Sanger sequencing-based typing, and reference strand-mediated conformational analysis. Retrospective UHR HLA typing of the cohort was performed for the six classic HLA loci using Pacific Biosciences Single Molecule Real-Time sequencing. To determine if there were viable alternatives to a 12/12 ultra-high resolution (UHR) HLA match, they chose to test the HLA-DPB1 T cell epitope (TCE) model of permissible mismatching in this data set.
The scientists reported that of 891 bone marrow donors and their respective, they found that when patients were matched at 12 alleles across six HLA genes, five-year survival was 55% compared to 40% for patients with any degree of mismatch. In addition, they found that 29% of patients who were previously thought to be matched via HLA typing methods that included Sanger sequencing and sequencing-specific oligonucleotide probing, actually had at least one mismatch when they were retrospectively analyzed using long-read sequencing on the Pacific Biosciences RS II platform. And, five-year survival among these patients was also lower at 30%.
Neema P Mayor, PhD, Head of Immunogenetics and lead author of the study, said, “We thought all of these individuals had been well matched, but they were not as well-matched as we had previously thought. Then, when the team analyzed the outcomes, they found that the individuals with mismatches that we didn't know about did significantly worse.” The study was published in the March 2019 issue of the journal Biology of Blood and Marrow Transplantation.
Related Links:
Anthony Nolan Research Institute
Latest Hematology News
- Rapid Cartridge-Based Test Aims to Expand Access to Hemoglobin Disorder Diagnosis
- New Guidelines Aim to Improve AL Amyloidosis Diagnosis
- Automated Hemostasis System Helps Labs of All Sizes Optimize Workflow
- Fast and Easy Test Could Revolutionize Blood Transfusions
- High-Sensitivity Blood Test Improves Assessment of Clotting Risk in Heart Disease Patients
- AI Algorithm Effectively Distinguishes Alpha Thalassemia Subtypes
- MRD Tests Could Predict Survival in Leukemia Patients
- Platelet Activity Blood Test in Middle Age Could Identify Early Alzheimer’s Risk
- Microvesicles Measurement Could Detect Vascular Injury in Sickle Cell Disease Patients
- ADLM’s New Coagulation Testing Guidance to Improve Care for Patients on Blood Thinners
- Viscoelastic Testing Could Improve Treatment of Maternal Hemorrhage
- Pioneering Model Measures Radiation Exposure in Blood for Precise Cancer Treatments
- Platelets Could Improve Early and Minimally Invasive Detection of Cancer
- Portable and Disposable Device Obtains Platelet-Rich Plasma Without Complex Equipment
- Disposable Cartridge-Based Test Delivers Rapid and Accurate CBC Results
- First Point-of-Care Heparin Monitoring Test Provides Results in Under 15 Minutes

Channels
Clinical Chemistry
view channel
Simple Blood Test Offers New Path to Alzheimer’s Assessment in Primary Care
Timely evaluation of cognitive symptoms in primary care is often limited by restricted access to specialized diagnostics and invasive confirmatory procedures. Clinicians need accessible tools to determine... Read more
Existing Hospital Analyzers Can Identify Fake Liquid Medical Products
Counterfeit and substandard medicines remain a serious global health threat, with World Health Organization estimates suggesting that 10.5% of medicines in low- and middle-income countries are either fake... Read moreMolecular Diagnostics
view channel
Changes In Lymphatic Vessels Can Aid Early Identification of Aggressive Oral Cancer
Oral cancers are the most common malignant tumors in the head and neck region and cause more than 188,000 deaths worldwide each year. Unlike many other cancers, even small, early-stage oral tumors can... Read more
Molecular Monitoring Approach Helps Bladder Cancer Patients Avoid Surgery
Muscle-invasive bladder cancer is typically treated with chemotherapy followed by radical cystectomy, the complete removal of the bladder. While often effective, the surgery significantly affects quality... Read more
Genetic Tests to Speed Diagnosis of Lymphatic Disorders
Defects in the lymphatic system affect approximately one in every 3,500 newborns and can lead to severe complications, including organ failure, breathing difficulties, and life-threatening infections.... Read more
New Extraction Kit Enables Consistent, Scalable cfDNA Isolation from Multiple Biofluids
Circulating cell-free DNA (cfDNA) found in plasma, serum, urine, and cerebrospinal fluid is typically present at low concentrations and is often highly fragmented, making efficient recovery challenging... Read moreImmunology
view channel
New Biomarker Predicts Chemotherapy Response in Triple-Negative Breast Cancer
Triple-negative breast cancer is an aggressive form of breast cancer in which patients often show widely varying responses to chemotherapy. Predicting who will benefit from treatment remains challenging,... Read moreBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read more
Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
Immunotherapy has transformed cancer treatment, but only a small proportion of patients experience lasting benefit, with response rates often remaining between 10% and 20%. Clinicians currently lack reliable... Read moreMicrobiology
view channel
Three-Test Panel Launched for Detection of Liver Fluke Infections
Parasitic liver fluke infections remain endemic in parts of Asia, where transmission commonly occurs through consumption of raw freshwater fish or aquatic plants. Chronic infection is a well-established... Read more
Rapid Test Promises Faster Answers for Drug-Resistant Infections
Drug-resistant pathogens continue to pose a growing threat in healthcare facilities, where delayed detection can impede outbreak control and increase mortality. Candida auris is notoriously difficult to... Read more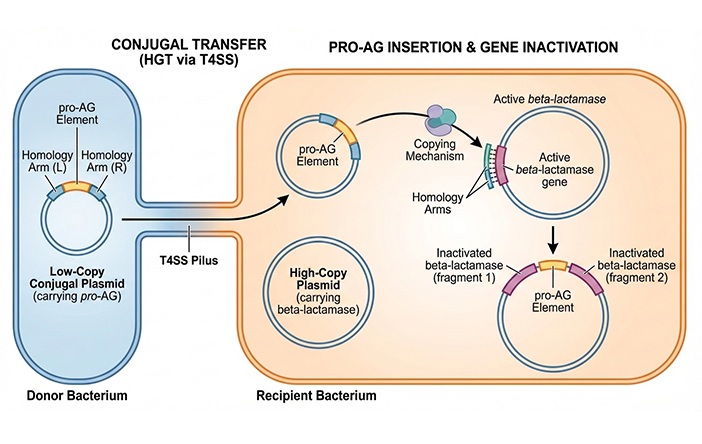
CRISPR-Based Technology Neutralizes Antibiotic-Resistant Bacteria
Antibiotic resistance has accelerated into a global health crisis, with projections estimating more than 10 million deaths per year by 2050 as drug-resistant “superbugs” continue to spread.... Read more
Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
Alzheimer’s disease affects approximately 6.7 million people in the United States and nearly 50 million worldwide, yet early cognitive decline remains difficult to characterize. Increasing evidence suggests... Read morePathology
view channel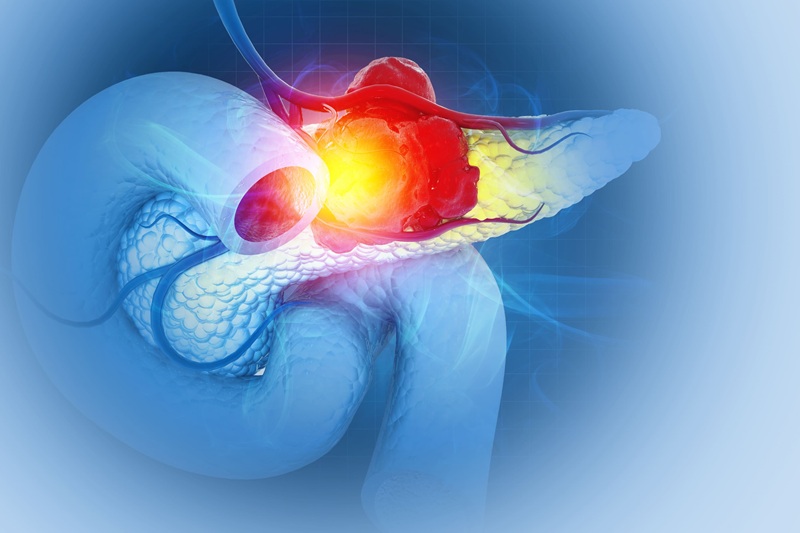
Single Sample Classifier Predicts Cancer-Associated Fibroblast Subtypes in Patient Samples
Pancreatic ductal adenocarcinoma (PDAC) remains one of the deadliest cancers, in part because of its dense tumor microenvironment that influences how tumors grow and respond to treatment.... Read more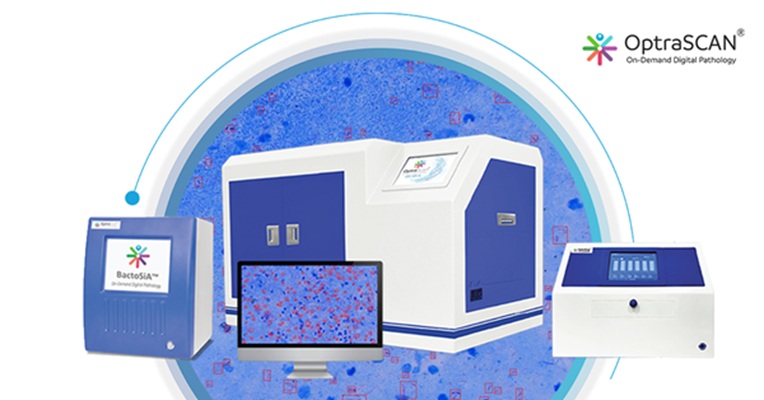
New AI-Driven Platform Standardizes Tuberculosis Smear Microscopy Workflow
Sputum smear microscopy remains central to tuberculosis treatment monitoring and follow-up, particularly in high‑burden settings where serial testing is routine. Yet consistent, repeatable bacillary assessment... Read more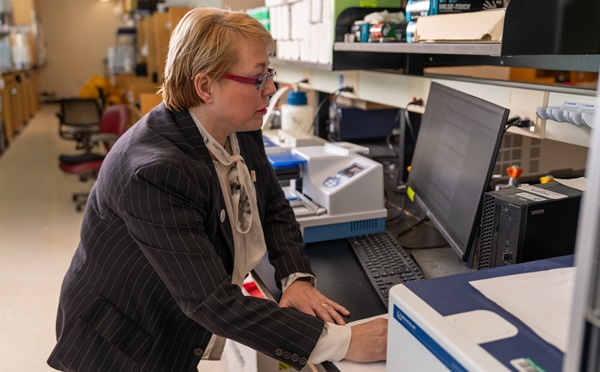
AI Tool Uses Blood Biomarkers to Predict Transplant Complications Before Symptoms Appear
Stem cell and bone marrow transplants can be lifesaving, but serious complications may arise months after patients leave the hospital. One of the most dangerous is chronic graft-versus-host disease, in... Read moreTechnology
view channel
Blood Test “Clocks” Predict Start of Alzheimer’s Symptoms
More than 7 million Americans live with Alzheimer’s disease, and related health and long-term care costs are projected to reach nearly USD 400 billion in 2025. The disease has no cure, and symptoms often... Read more
AI-Powered Biomarker Predicts Liver Cancer Risk
Liver cancer, or hepatocellular carcinoma, causes more than 800,000 deaths worldwide each year and often goes undetected until late stages. Even after treatment, recurrence rates reach 70% to 80%, contributing... Read more
Robotic Technology Unveiled for Automated Diagnostic Blood Draws
Routine diagnostic blood collection is a high‑volume task that can strain staffing and introduce human‑dependent variability, with downstream implications for sample quality and patient experience.... Read more
ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
Clinical laboratories generate billions of test results each year, creating a treasure trove of data with the potential to support more personalized testing, improve operational efficiency, and enhance patient care.... Read moreIndustry
view channel
QuidelOrtho Collaborates with Lifotronic to Expand Global Immunoassay Portfolio
QuidelOrtho (San Diego, CA, USA) has entered a long-term strategic supply agreement with Lifotronic Technology (Shenzhen, China) to expand its global immunoassay portfolio and accelerate customer access... Read more










 (3) (1).png)