Blood Test Detects New Breast Cancer Subtype
|
By LabMedica International staff writers Posted on 14 Sep 2016 |

Image: The QX200 Droplet Digital Polymerase Chain reaction (ddPCR) system (Photo courtesy of Bio-Rad).
A blood test has been developed that detects when the most common form of breast cancer has become resistant to treatment could double the average time it takes for the disease to progress, from around two and a half to around six months.
The test detects mutations to a gene called estrogen receptor 1, or ESR1, which indicate that receptors for the female hormone estrogen in the cancer cells that are usually driven by the hormone have evolved to stay permanently switched on without it which means hormonal treatments that block estrogen production will no longer be effective.
Scientists at the Institute of Cancer Research (London, UK) and their colleagues analyzed blood samples from a total of 783 women enrolled on two major phase III clinical trials of new treatments for advanced estrogen receptor positive breast cancer, which accounts for three quarters of all cases. DNA extraction was performed using the QIAamp Circulating Nucleic Acid Kit (Qiagen, Hilden, Germany).
Total free DNA was quantified from plasma using RNase P as the reference gene. For ESR1 mutation analysis, the team used commercially available multiplex droplet digital polymerase chain reaction (ddPCR) assays for the seven most common ESR1 mutations. The ddPCR was performed on a QX200 system (Bio-Rad, Hercules, CA, USA). A multiplex assay was considered mutation positive if at least two ESR1 mutant droplets were observed. The results obtained on the multiplex ddPCR were further characterized using uniplex ddPCR assays.
The investigators found that nearly 40% of the 162 patient blood samples available, taken going into the trial, were found to have mutations in the estrogen receptor. These women responded better to fulvestrant, which delayed progression of the disease for 5.7 months, compared to 2.6 months on exemestane. For women without ESR1 mutations both treatments, fulvestrant and exemestane, had the same effectiveness.
The scientists also looked at a second trial that had compared treatment with fulvestrant and a placebo to fulvestrant and palbociclib. They found 25.3 %of patient blood samples had estrogen receptor mutations going into this trial. But because palbociclib targets different molecules, the patients had the same outcomes regardless of whether or not they had the mutation in the estrogen receptor.
Nicholas Turner, MD, PhD, a medical oncologist and team leader said, “Our results show that breast cancer with and without ESR1 mutations are distinct subtypes that respond differently to treatment. These subtypes can be diagnosed simply and cheaply from a blood test, and should be considered for future clinical trials of advanced breast cancer to ensure patients are receiving the best treatment for their cancer. For the first time we should able to use a potentially simple test to help us pick the best treatment for women with advanced cancer after their initial treatment has failed. We do need to confirm the results in another trial before we can implement this clinically.” The study was published on September 1, 2016, in the Journal of Clinical Oncology.
Related Links:
Institute of Cancer Research
Qiagen
Bio-Rad
The test detects mutations to a gene called estrogen receptor 1, or ESR1, which indicate that receptors for the female hormone estrogen in the cancer cells that are usually driven by the hormone have evolved to stay permanently switched on without it which means hormonal treatments that block estrogen production will no longer be effective.
Scientists at the Institute of Cancer Research (London, UK) and their colleagues analyzed blood samples from a total of 783 women enrolled on two major phase III clinical trials of new treatments for advanced estrogen receptor positive breast cancer, which accounts for three quarters of all cases. DNA extraction was performed using the QIAamp Circulating Nucleic Acid Kit (Qiagen, Hilden, Germany).
Total free DNA was quantified from plasma using RNase P as the reference gene. For ESR1 mutation analysis, the team used commercially available multiplex droplet digital polymerase chain reaction (ddPCR) assays for the seven most common ESR1 mutations. The ddPCR was performed on a QX200 system (Bio-Rad, Hercules, CA, USA). A multiplex assay was considered mutation positive if at least two ESR1 mutant droplets were observed. The results obtained on the multiplex ddPCR were further characterized using uniplex ddPCR assays.
The investigators found that nearly 40% of the 162 patient blood samples available, taken going into the trial, were found to have mutations in the estrogen receptor. These women responded better to fulvestrant, which delayed progression of the disease for 5.7 months, compared to 2.6 months on exemestane. For women without ESR1 mutations both treatments, fulvestrant and exemestane, had the same effectiveness.
The scientists also looked at a second trial that had compared treatment with fulvestrant and a placebo to fulvestrant and palbociclib. They found 25.3 %of patient blood samples had estrogen receptor mutations going into this trial. But because palbociclib targets different molecules, the patients had the same outcomes regardless of whether or not they had the mutation in the estrogen receptor.
Nicholas Turner, MD, PhD, a medical oncologist and team leader said, “Our results show that breast cancer with and without ESR1 mutations are distinct subtypes that respond differently to treatment. These subtypes can be diagnosed simply and cheaply from a blood test, and should be considered for future clinical trials of advanced breast cancer to ensure patients are receiving the best treatment for their cancer. For the first time we should able to use a potentially simple test to help us pick the best treatment for women with advanced cancer after their initial treatment has failed. We do need to confirm the results in another trial before we can implement this clinically.” The study was published on September 1, 2016, in the Journal of Clinical Oncology.
Related Links:
Institute of Cancer Research
Qiagen
Bio-Rad
Latest Molecular Diagnostics News
- Diagnostic Device Predicts Treatment Response for Brain Tumors Via Blood Test
- Blood Test Detects Early-Stage Cancers by Measuring Epigenetic Instability
- Two-in-One DNA Analysis Improves Diagnostic Accuracy While Saving Time and Costs
- “Lab-On-A-Disc” Device Paves Way for More Automated Liquid Biopsies
- New Tool Maps Chromosome Shifts in Cancer Cells to Predict Tumor Evolution
- Blood Test Identifies Inflammatory Breast Cancer Patients at Increased Risk of Brain Metastasis
- Newly-Identified Parkinson’s Biomarkers to Enable Early Diagnosis Via Blood Tests
- New Blood Test Could Detect Pancreatic Cancer at More Treatable Stage
- Liquid Biopsy Could Replace Surgical Biopsy for Diagnosing Primary Central Nervous Lymphoma
- New Tool Reveals Hidden Metabolic Weakness in Blood Cancers
- World's First Blood Test Distinguishes Between Benign and Cancerous Lung Nodules
- Rapid Test Uses Mobile Phone to Identify Severe Imported Malaria Within Minutes
- Gut Microbiome Signatures Predict Long-Term Outcomes in Acute Pancreatitis
- Blood Test Promises Faster Answers for Deadly Fungal Infections
- Blood Test Could Detect Infection Exposure History
- Urine-Based MRD Test Tracks Response to Bladder Cancer Surgery
Channels
Clinical Chemistry
view channel
New PSA-Based Prognostic Model Improves Prostate Cancer Risk Assessment
Prostate cancer is the second-leading cause of cancer death among American men, and about one in eight will be diagnosed in their lifetime. Screening relies on blood levels of prostate-specific antigen... Read more
Extracellular Vesicles Linked to Heart Failure Risk in CKD Patients
Chronic kidney disease (CKD) affects more than 1 in 7 Americans and is strongly associated with cardiovascular complications, which account for more than half of deaths among people with CKD.... Read moreMolecular Diagnostics
view channel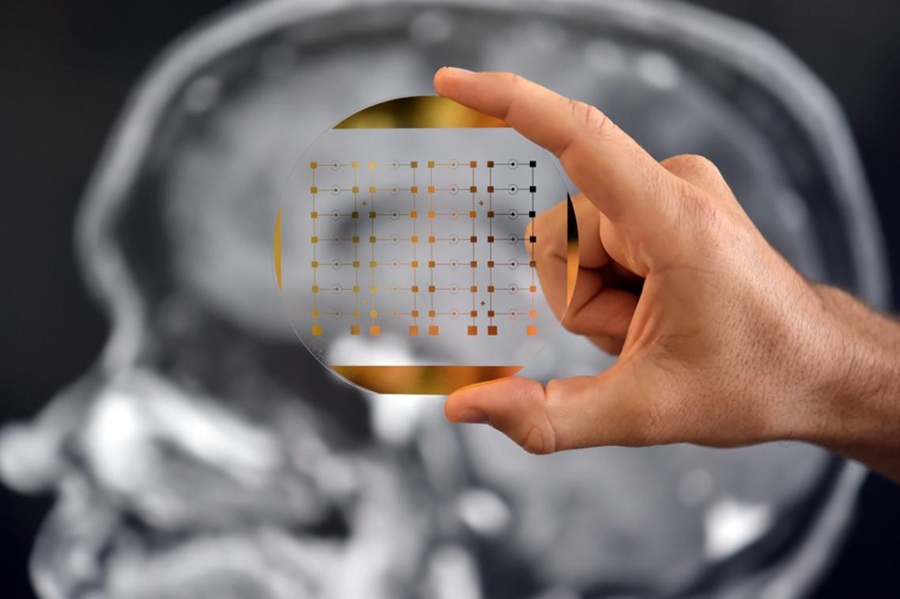
Diagnostic Device Predicts Treatment Response for Brain Tumors Via Blood Test
Glioblastoma is one of the deadliest forms of brain cancer, largely because doctors have no reliable way to determine whether treatments are working in real time. Assessing therapeutic response currently... Read more
Blood Test Detects Early-Stage Cancers by Measuring Epigenetic Instability
Early-stage cancers are notoriously difficult to detect because molecular changes are subtle and often missed by existing screening tools. Many liquid biopsies rely on measuring absolute DNA methylation... Read more
“Lab-On-A-Disc” Device Paves Way for More Automated Liquid Biopsies
Extracellular vesicles (EVs) are tiny particles released by cells into the bloodstream that carry molecular information about a cell’s condition, including whether it is cancerous. However, EVs are highly... Read more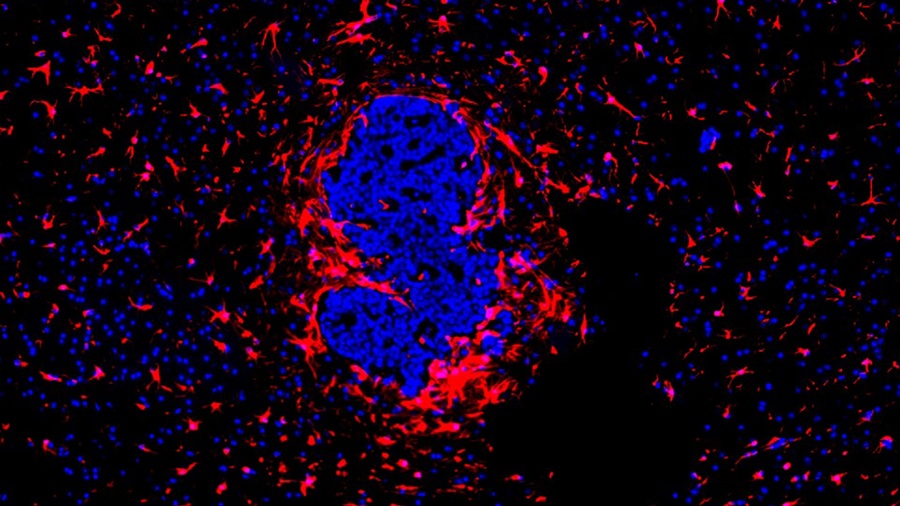
Blood Test Identifies Inflammatory Breast Cancer Patients at Increased Risk of Brain Metastasis
Brain metastasis is a frequent and devastating complication in patients with inflammatory breast cancer, an aggressive subtype with limited treatment options. Despite its high incidence, the biological... Read moreHematology
view channel
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read more
Fast and Easy Test Could Revolutionize Blood Transfusions
Blood transfusions are a cornerstone of modern medicine, yet red blood cells can deteriorate quietly while sitting in cold storage for weeks. Although blood units have a fixed expiration date, cells from... Read more
Automated Hemostasis System Helps Labs of All Sizes Optimize Workflow
High-volume hemostasis sections must sustain rapid turnaround while managing reruns and reflex testing. Manual tube handling and preanalytical checks can strain staff time and increase opportunities for error.... Read more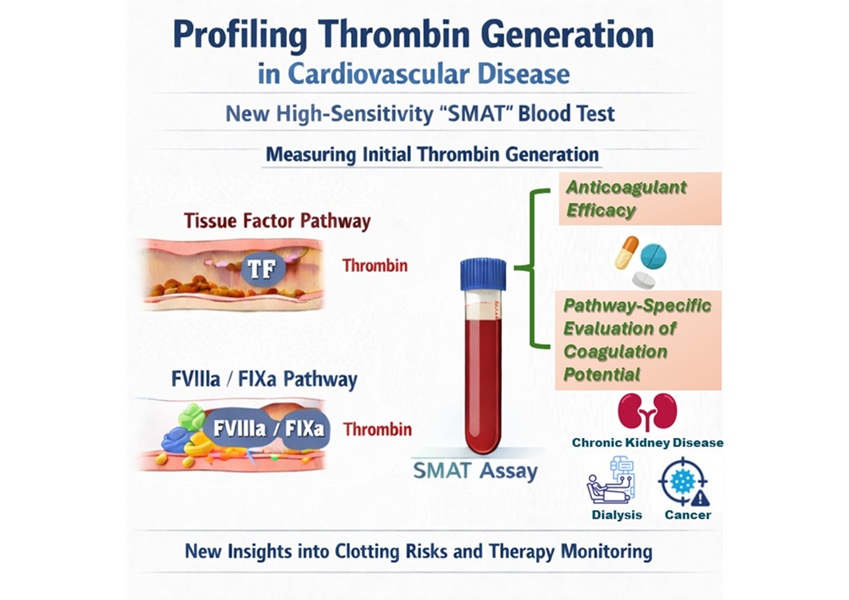
High-Sensitivity Blood Test Improves Assessment of Clotting Risk in Heart Disease Patients
Blood clotting is essential for preventing bleeding, but even small imbalances can lead to serious conditions such as thrombosis or dangerous hemorrhage. In cardiovascular disease, clinicians often struggle... Read moreImmunology
view channelBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read more
Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
Immunotherapy has transformed cancer treatment, but only a small proportion of patients experience lasting benefit, with response rates often remaining between 10% and 20%. Clinicians currently lack reliable... Read moreMicrobiology
view channel
Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
Alzheimer’s disease affects approximately 6.7 million people in the United States and nearly 50 million worldwide, yet early cognitive decline remains difficult to characterize. Increasing evidence suggests... Read moreAI-Powered Platform Enables Rapid Detection of Drug-Resistant C. Auris Pathogens
Infections caused by the pathogenic yeast Candida auris pose a significant threat to hospitalized patients, particularly those with weakened immune systems or those who have invasive medical devices.... Read moreTechnology
view channel
Robotic Technology Unveiled for Automated Diagnostic Blood Draws
Routine diagnostic blood collection is a high‑volume task that can strain staffing and introduce human‑dependent variability, with downstream implications for sample quality and patient experience.... Read more
ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
Clinical laboratories generate billions of test results each year, creating a treasure trove of data with the potential to support more personalized testing, improve operational efficiency, and enhance patient care.... Read moreAptamer Biosensor Technology to Transform Virus Detection
Rapid and reliable virus detection is essential for controlling outbreaks, from seasonal influenza to global pandemics such as COVID-19. Conventional diagnostic methods, including cell culture, antigen... Read more
AI Models Could Predict Pre-Eclampsia and Anemia Earlier Using Routine Blood Tests
Pre-eclampsia and anemia are major contributors to maternal and child mortality worldwide, together accounting for more than half a million deaths each year and leaving millions with long-term health complications.... Read moreIndustry
view channelNew Collaboration Brings Automated Mass Spectrometry to Routine Laboratory Testing
Mass spectrometry is a powerful analytical technique that identifies and quantifies molecules based on their mass and electrical charge. Its high selectivity, sensitivity, and accuracy make it indispensable... Read more
AI-Powered Cervical Cancer Test Set for Major Rollout in Latin America
Noul Co., a Korean company specializing in AI-based blood and cancer diagnostics, announced it will supply its intelligence (AI)-based miLab CER cervical cancer diagnostic solution to Mexico under a multi‑year... Read more
Diasorin and Fisher Scientific Enter into US Distribution Agreement for Molecular POC Platform
Diasorin (Saluggia, Italy) has entered into an exclusive distribution agreement with Fisher Scientific, part of Thermo Fisher Scientific (Waltham, MA, USA), for the LIAISON NES molecular point-of-care... Read more