Blood Test Predicts Survival in Liver Cancer Patients
Posted on 20 Sep 2024
Hepatocellular carcinoma (HCC) is the most common form of liver cancer and ranks as the fourth leading cause of cancer-related deaths worldwide. For patients with advanced HCC, several systemic treatments are available that travel through the bloodstream to target cancer cells throughout the body. One such treatment involves the combination of the drugs atezolizumab and bevacizumab, known as Atezo/Bev therapy, which is generally recommended as the first-line treatment for liver cancer. However, there are currently no reliable markers to predict the therapy’s effectiveness. Researchers have now discovered that serum autoantibody levels may serve as a predictive marker for treatment response in liver cancer patients.
In a recent study, a research team from Okayama University (Okayama, Japan) investigated the use of anti-PD1 autoantibodies as a prognostic marker for cancer. To identify a reliable marker for predicting treatment efficacy, the researchers focused on autoantibodies—antibodies produced by the immune system that target the body’s own proteins. These autoantibodies have been found in various types of cancer and can be easily detected in blood serum, making them promising biomarker candidates. The researchers hypothesized that anti-PD-1 autoantibodies could influence the effectiveness of Atezo/Bev therapy, as they target the same cellular pathways as atezolizumab.
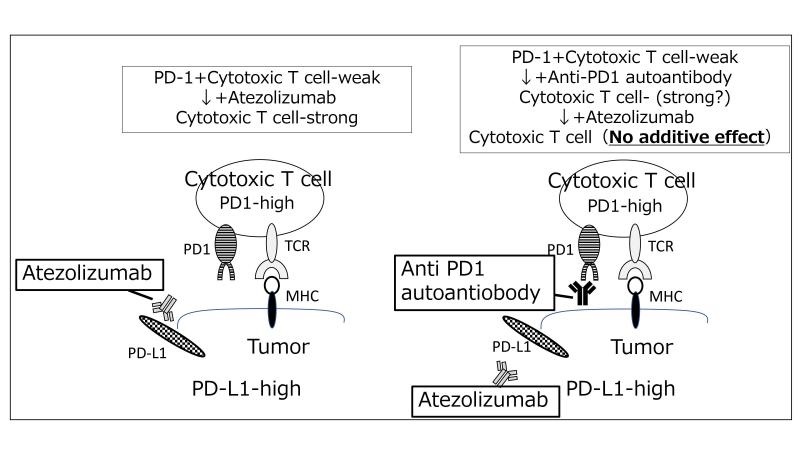
To test this hypothesis, the researchers conducted a study involving 63 patients with advanced HCC who received Atezo/Bev therapy. They measured the levels of anti-PD-1 autoantibodies in the patients’ blood serum both before and after treatment, analyzing the relationship between these levels and the patients’ treatment outcomes. Their findings, published in Gastro Hep Advances, revealed a statistically significant correlation between higher levels of anti-PD-1 autoantibodies and lower survival rates. This suggests that anti-PD-1 autoantibodies could serve as a potential biomarker for predicting the response to immune checkpoint inhibitors, including atezolizumab, in patients with HCC. However, further research is needed to better understand the biological role of these autoantibodies in cancer immunotherapy.
“Ours is the first study to report that higher serum anti-PD-1 autoantibody levels were associated with a poor prognosis in patients who received Atezo/Bev as first-line therapy,” said Dr. Akinobu Takaki from the Department of Gastroenterology and Hepatology, Okayama University who led the research team. “Notably, serum levels of anti-PD-1 autoantibody may serve as a novel potential biomarker for predicting the efficacy of immune checkpoint inhibitors in patients with HCC. Overall, our findings will bring hope to patients with liver cancer and pave the way for development of improved treatment regimens in the future.”