Hyaluronic Acid Turbidimetric Assay Compared to Standard Method
|
By LabMedica International staff writers Posted on 13 Jan 2016 |

Image: The Hitachi 917 Automatic Disk-Chemistry Analyzer (Photo courtesy of Roche Diagnostics).
Circulating hyaluronic acid (HA) in human adults is primarily produced in the peripheral soft connective tissue and transported to the systemic circulation via lymph drainage and the majority of HA is removed from circulation by hepatic elimination.
HA is essentially non-immunogenic, which has excluded direct immunochemical methods of measurement. To accommodate this, several advanced methods of measurements have been used including enzymatic degradation; hyaluronic-binding protein (HABP) linked enzyme-linked immunosorbent assay (ELISA) and high-performance liquid chromatography.
Scientists at the Nordsjaellands Hospital, University of Copenhagen, (Denmark) and their colleagues measured HA concentrations in 39 samples of serum from 39 randomly selected intensive care unit (ICU) patients. The HA was measured by a particle-enhanced turbidimetric immunoassay (PETIA) and enzyme-linked immunosorbent assay (ELISA) in a 40-sample dilution series and the 39 ICU patients.
The HA was measured with the PETIA (Corgenix; Broomfield, CO, USA) in ICU samples on the Hitachi 917 (Roche Diagnostics, GmbH; Mannheim, Germany) and in the dilution series on Modular P (Roche Diagnostics GmbH) analyzers (test assay), and by Corgenix HA ELISA using double determination (reference method).
The scientists found that in the ICU patients, the median HA concentration was 159.0 ng/mL (interquartile range (IQR) 117.5–362.5 ng/mL) with ELISA and 157.5 ng/ml (IQR 92.5–359.6 ng/mL) with PETIA. The mean difference was 12.88 ng/mL which was statistically significant and the 95% limits of agreement were −91.17 to 116.9 ng/mL. In the dilution series, the mean difference was −59.26 ng/mL (95% CI, −74.68 to 43.84 ng/mL, and the 95% limits of agreement were 35.23 to −153.8 ng/mL.
The authors concluded that there was random variation between the PETIA and ELISA test that could affect performance in a clinical context. The new clinical biochemistry assay for HA determination will allow for large studies of the clinical utility of HA. The study was published online on December 14, 2015, in the Journal of Clinical Laboratory Analysis.
Related Links:
Nordsjaellands Hospital
Corgenix
Roche Diagnostics GmbH
HA is essentially non-immunogenic, which has excluded direct immunochemical methods of measurement. To accommodate this, several advanced methods of measurements have been used including enzymatic degradation; hyaluronic-binding protein (HABP) linked enzyme-linked immunosorbent assay (ELISA) and high-performance liquid chromatography.
Scientists at the Nordsjaellands Hospital, University of Copenhagen, (Denmark) and their colleagues measured HA concentrations in 39 samples of serum from 39 randomly selected intensive care unit (ICU) patients. The HA was measured by a particle-enhanced turbidimetric immunoassay (PETIA) and enzyme-linked immunosorbent assay (ELISA) in a 40-sample dilution series and the 39 ICU patients.
The HA was measured with the PETIA (Corgenix; Broomfield, CO, USA) in ICU samples on the Hitachi 917 (Roche Diagnostics, GmbH; Mannheim, Germany) and in the dilution series on Modular P (Roche Diagnostics GmbH) analyzers (test assay), and by Corgenix HA ELISA using double determination (reference method).
The scientists found that in the ICU patients, the median HA concentration was 159.0 ng/mL (interquartile range (IQR) 117.5–362.5 ng/mL) with ELISA and 157.5 ng/ml (IQR 92.5–359.6 ng/mL) with PETIA. The mean difference was 12.88 ng/mL which was statistically significant and the 95% limits of agreement were −91.17 to 116.9 ng/mL. In the dilution series, the mean difference was −59.26 ng/mL (95% CI, −74.68 to 43.84 ng/mL, and the 95% limits of agreement were 35.23 to −153.8 ng/mL.
The authors concluded that there was random variation between the PETIA and ELISA test that could affect performance in a clinical context. The new clinical biochemistry assay for HA determination will allow for large studies of the clinical utility of HA. The study was published online on December 14, 2015, in the Journal of Clinical Laboratory Analysis.
Related Links:
Nordsjaellands Hospital
Corgenix
Roche Diagnostics GmbH
Latest Immunology News
- Blood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
- Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
- Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
- Blood Test Could Identify Colon Cancer Patients to Benefit from NSAIDs
- Blood Test Could Detect Adverse Immunotherapy Effects
- Routine Blood Test Can Predict Who Benefits Most from CAR T-Cell Therapy
- New Test Distinguishes Vaccine-Induced False Positives from Active HIV Infection
- Gene Signature Test Predicts Response to Key Breast Cancer Treatment
- Chip Captures Cancer Cells from Blood to Help Select Right Breast Cancer Treatment
- Blood-Based Liquid Biopsy Model Analyzes Immunotherapy Effectiveness
- Signature Genes Predict T-Cell Expansion in Cancer Immunotherapy
- Molecular Microscope Diagnostic System Assesses Lung Transplant Rejection
- Blood Test Tracks Treatment Resistance in High-Grade Serous Ovarian Cancer
- Luminescent Probe Measures Immune Cell Activity in Real Time
- Blood-Based Immune Cell Signatures Could Guide Treatment Decisions for Critically Ill Patients
- Novel Tool Predicts Most Effective Multiple Sclerosis Medication for Patients
Channels
Molecular Diagnostics
view channel
POC Test Uses Fingerstick Blood, Serum, Or Plasma Sample to Detect Typhoid Fever
Typhoid fever is an acute febrile illness caused by Salmonella enterica serovar Typhi (S. Typhi) and affects an estimated 11–21 million people globally each year, resulting in approximately 128,000–161,000... Read more
Rapid Testing Panel Simultaneously Detects 15 Drugs of Abuse in Urine Within 21 Minutes
Illicit drug use and excessive use of prescription medicine is growing across the US amid a severe opioid crisis. Although overdose fatalities were reported to have declined by nearly 27% in 2024, many... Read moreHematology
view channel
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read more
Fast and Easy Test Could Revolutionize Blood Transfusions
Blood transfusions are a cornerstone of modern medicine, yet red blood cells can deteriorate quietly while sitting in cold storage for weeks. Although blood units have a fixed expiration date, cells from... Read more
Automated Hemostasis System Helps Labs of All Sizes Optimize Workflow
High-volume hemostasis sections must sustain rapid turnaround while managing reruns and reflex testing. Manual tube handling and preanalytical checks can strain staff time and increase opportunities for error.... Read more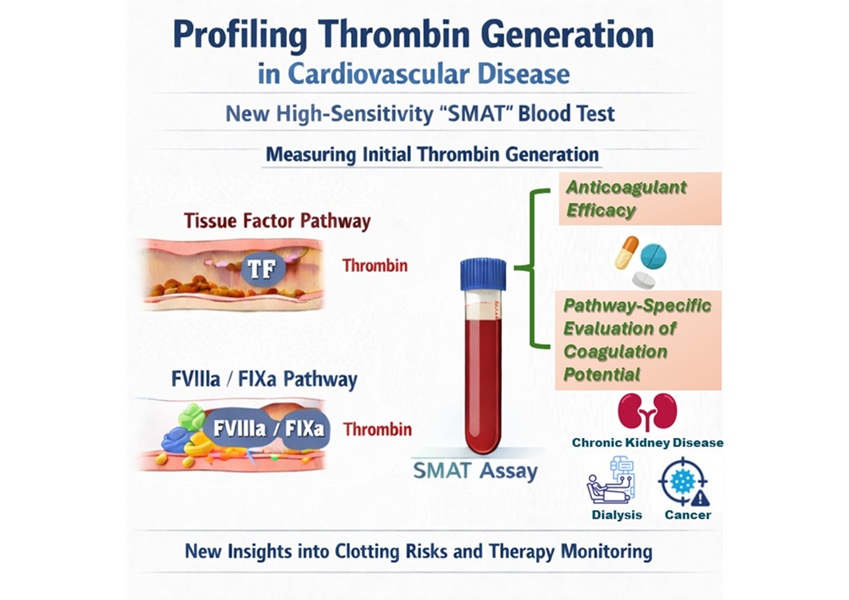
High-Sensitivity Blood Test Improves Assessment of Clotting Risk in Heart Disease Patients
Blood clotting is essential for preventing bleeding, but even small imbalances can lead to serious conditions such as thrombosis or dangerous hemorrhage. In cardiovascular disease, clinicians often struggle... Read moreImmunology
view channelBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read more
Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
Immunotherapy has transformed cancer treatment, but only a small proportion of patients experience lasting benefit, with response rates often remaining between 10% and 20%. Clinicians currently lack reliable... Read moreMicrobiology
view channel
Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
Alzheimer’s disease affects approximately 6.7 million people in the United States and nearly 50 million worldwide, yet early cognitive decline remains difficult to characterize. Increasing evidence suggests... Read moreAI-Powered Platform Enables Rapid Detection of Drug-Resistant C. Auris Pathogens
Infections caused by the pathogenic yeast Candida auris pose a significant threat to hospitalized patients, particularly those with weakened immune systems or those who have invasive medical devices.... Read morePathology
view channel
Engineered Yeast Cells Enable Rapid Testing of Cancer Immunotherapy
Developing new cancer immunotherapies is a slow, costly, and high-risk process, particularly for CAR T cell treatments that must precisely recognize cancer-specific antigens. Small differences in tumor... Read more
First-Of-Its-Kind Test Identifies Autism Risk at Birth
Autism spectrum disorder is treatable, and extensive research shows that early intervention can significantly improve cognitive, social, and behavioral outcomes. Yet in the United States, the average age... Read moreTechnology
view channel
Robotic Technology Unveiled for Automated Diagnostic Blood Draws
Routine diagnostic blood collection is a high‑volume task that can strain staffing and introduce human‑dependent variability, with downstream implications for sample quality and patient experience.... Read more
ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
Clinical laboratories generate billions of test results each year, creating a treasure trove of data with the potential to support more personalized testing, improve operational efficiency, and enhance patient care.... Read moreAptamer Biosensor Technology to Transform Virus Detection
Rapid and reliable virus detection is essential for controlling outbreaks, from seasonal influenza to global pandemics such as COVID-19. Conventional diagnostic methods, including cell culture, antigen... Read more
AI Models Could Predict Pre-Eclampsia and Anemia Earlier Using Routine Blood Tests
Pre-eclampsia and anemia are major contributors to maternal and child mortality worldwide, together accounting for more than half a million deaths each year and leaving millions with long-term health complications.... Read moreIndustry
view channel
WHX Labs in Dubai spotlights leadership skills shaping next-generation laboratories
WHX Labs in Dubai (formerly Medlab Middle East), held at Dubai World Trade Centre (DWTC) from 10–13 February, brings together international experts to discuss the factors redefining laboratory leadership,... Read moreNew Collaboration Brings Automated Mass Spectrometry to Routine Laboratory Testing
Mass spectrometry is a powerful analytical technique that identifies and quantifies molecules based on their mass and electrical charge. Its high selectivity, sensitivity, and accuracy make it indispensable... Read more
AI-Powered Cervical Cancer Test Set for Major Rollout in Latin America
Noul Co., a Korean company specializing in AI-based blood and cancer diagnostics, announced it will supply its intelligence (AI)-based miLab CER cervical cancer diagnostic solution to Mexico under a multi‑year... Read more









 Analyzer.jpg)