Hemostatic Profile Associated with Migraine with Aura
|
By LabMedica International staff writers Posted on 31 May 2021 |

Image: Appearance of a common form of typical migraine visual aura (Photo courtesy of Poojitha Mamindla, PharmD)
Nearly 15% of the population in the USA experiences migraine. One subtype of migraine that is not well understood is migraine with aura (MA). Individuals who experience MA often see flashing lights, blind spots, or jagged lines in their visual field prior to onset of their migraine headaches.
Individuals who experience MA also face a heightened risk of stroke and cardiovascular disease, although scientists continue to explore why this correlation exists. Based on prior studies, it is controversial whether enhanced atherosclerosis among individuals with MA is likely to explain the migraine association with stroke, suggesting the existence of alternative mechanisms including endothelial activation or a potential role of hypercoagulability and microemboli.
An international team of Medical Scientists led by Brigham and Women's Hospital (Boston, MA, USA) investigated potential causal relationships between hemostatic profiles and migraine by leveraging largescale genome-wide association study (GWAS) summary statistics for migraine and migraine subtypes (MA and migraine without aura [MO]), and for eight hemostatic factors (including plasma levels or activities of fibrinogen, D-dimer, coagulation factor VII [FVII], coagulation factor VIII [FVIII], coagulation factor XI [FXI], von Willebrand factor [vWF], tissue plasminogen activator [tPA], and plasminogen activator inhibitor-1 [PAI-1] among up to 120,246 individuals), two hemostasis clinical tests (activated partial thromboplastin time [aPTT] and prothrombin time/international normalized ratio [PT/INR], which are commonly used to screen for coagulation-factor deficiencies), as well as serum concentrations of two forms of fibrinopeptide A (fibrinopeptide A [ADSGEGDFXAEGGGVR*] and phosphorylated fibrinopeptide A [ADpSGEGDFXAEGGGVR*]).
The investigators found a strong association between four coagulation factors and migraine susceptibility. They observed that genetically increased levels of three blood clotting factors: coagulation factor VIII, von Willebrand factor, and phosphorylated fibrinopeptide A, and genetically decreased levels of fibrinogen (a protein important in the late stages of the blood clotting process) were all associated, in part, with migraine susceptibility. Interestingly, scientists did not find this association among individuals who experience migraine without aura (MO), indicating a specific relationship between these hemostatic factors and MA.
Yanjun Guo, MD, PhD, of the Division of Preventative Medicine at the Brigham and the first author of the study, said, “It is very exciting that by using Mendelian randomization we were able to show that hemostatic factors are associated with MA. And because in the observational studies we saw that MA patients have a higher risk of stroke, these findings may reveal a potential connection between MA and stroke.”
The authors concluded that their findings suggest potential causal roles of genetically determined elevated FVIII, vWF, phosphorylated fibrinopeptide A, and decreased fibrinogen in migraine susceptibility, especially for MA, but the effects of FVIII and vWF on migraine are not independent from each other. The study was originally published online on April 1, 2021 in the journal Neurology.
Related Links:
Brigham and Women's Hospital
Individuals who experience MA also face a heightened risk of stroke and cardiovascular disease, although scientists continue to explore why this correlation exists. Based on prior studies, it is controversial whether enhanced atherosclerosis among individuals with MA is likely to explain the migraine association with stroke, suggesting the existence of alternative mechanisms including endothelial activation or a potential role of hypercoagulability and microemboli.
An international team of Medical Scientists led by Brigham and Women's Hospital (Boston, MA, USA) investigated potential causal relationships between hemostatic profiles and migraine by leveraging largescale genome-wide association study (GWAS) summary statistics for migraine and migraine subtypes (MA and migraine without aura [MO]), and for eight hemostatic factors (including plasma levels or activities of fibrinogen, D-dimer, coagulation factor VII [FVII], coagulation factor VIII [FVIII], coagulation factor XI [FXI], von Willebrand factor [vWF], tissue plasminogen activator [tPA], and plasminogen activator inhibitor-1 [PAI-1] among up to 120,246 individuals), two hemostasis clinical tests (activated partial thromboplastin time [aPTT] and prothrombin time/international normalized ratio [PT/INR], which are commonly used to screen for coagulation-factor deficiencies), as well as serum concentrations of two forms of fibrinopeptide A (fibrinopeptide A [ADSGEGDFXAEGGGVR*] and phosphorylated fibrinopeptide A [ADpSGEGDFXAEGGGVR*]).
The investigators found a strong association between four coagulation factors and migraine susceptibility. They observed that genetically increased levels of three blood clotting factors: coagulation factor VIII, von Willebrand factor, and phosphorylated fibrinopeptide A, and genetically decreased levels of fibrinogen (a protein important in the late stages of the blood clotting process) were all associated, in part, with migraine susceptibility. Interestingly, scientists did not find this association among individuals who experience migraine without aura (MO), indicating a specific relationship between these hemostatic factors and MA.
Yanjun Guo, MD, PhD, of the Division of Preventative Medicine at the Brigham and the first author of the study, said, “It is very exciting that by using Mendelian randomization we were able to show that hemostatic factors are associated with MA. And because in the observational studies we saw that MA patients have a higher risk of stroke, these findings may reveal a potential connection between MA and stroke.”
The authors concluded that their findings suggest potential causal roles of genetically determined elevated FVIII, vWF, phosphorylated fibrinopeptide A, and decreased fibrinogen in migraine susceptibility, especially for MA, but the effects of FVIII and vWF on migraine are not independent from each other. The study was originally published online on April 1, 2021 in the journal Neurology.
Related Links:
Brigham and Women's Hospital
Latest Hematology News
- Next Generation Instrument Screens for Hemoglobin Disorders in Newborns
- First 4-in-1 Nucleic Acid Test for Arbovirus Screening to Reduce Risk of Transfusion-Transmitted Infections
- POC Finger-Prick Blood Test Determines Risk of Neutropenic Sepsis in Patients Undergoing Chemotherapy
- First Affordable and Rapid Test for Beta Thalassemia Demonstrates 99% Diagnostic Accuracy
- Handheld White Blood Cell Tracker to Enable Rapid Testing For Infections
- Smart Palm-size Optofluidic Hematology Analyzer Enables POCT of Patients’ Blood Cells
- Automated Hematology Platform Offers High Throughput Analytical Performance
- New Tool Analyzes Blood Platelets Faster, Easily and Accurately
- First Rapid-Result Hematology Analyzer Reports Measures of Infection and Severity at POC
- Bleeding Risk Diagnostic Test to Reduce Preventable Complications in Hospitals
- True POC Hematology Analyzer with Direct Capillary Sampling Enhances Ease-of-Use and Testing Throughput
- Point of Care CBC Analyzer with Direct Capillary Sampling Enhances Ease-of-Use and Testing Throughput
- Blood Test Could Predict Outcomes in Emergency Department and Hospital Admissions
- Novel Technology Diagnoses Immunothrombosis Using Breath Gas Analysis
- Advanced Hematology System Allows Labs to Process Up To 119 Complete Blood Count Results per Hour
- Unique AI-Based Approach Automates Clinical Analysis of Blood Data
Channels
Clinical Chemistry
view channel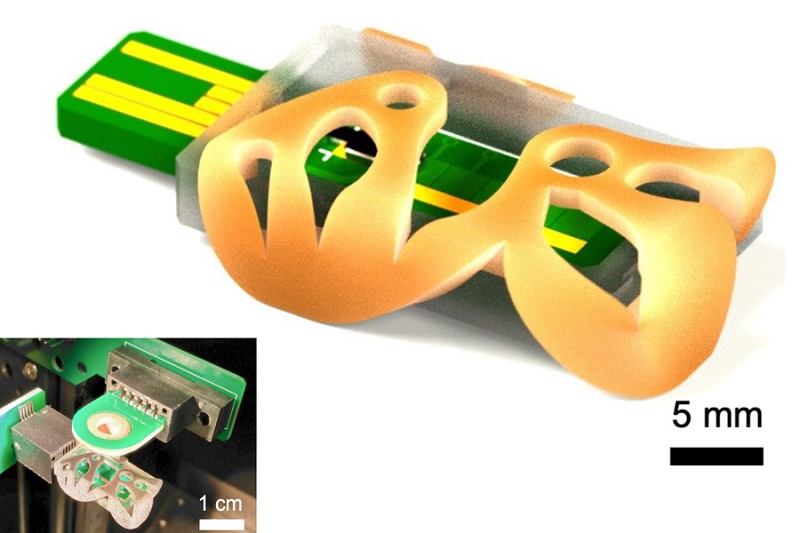
3D Printed Point-Of-Care Mass Spectrometer Outperforms State-Of-The-Art Models
Mass spectrometry is a precise technique for identifying the chemical components of a sample and has significant potential for monitoring chronic illness health states, such as measuring hormone levels... Read more.jpg)
POC Biomedical Test Spins Water Droplet Using Sound Waves for Cancer Detection
Exosomes, tiny cellular bioparticles carrying a specific set of proteins, lipids, and genetic materials, play a crucial role in cell communication and hold promise for non-invasive diagnostics.... Read more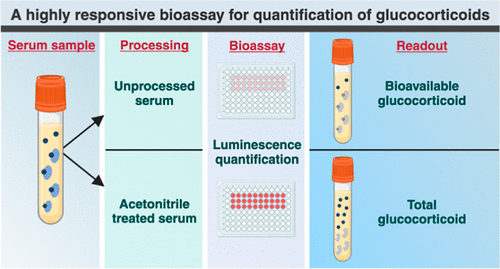
Highly Reliable Cell-Based Assay Enables Accurate Diagnosis of Endocrine Diseases
The conventional methods for measuring free cortisol, the body's stress hormone, from blood or saliva are quite demanding and require sample processing. The most common method, therefore, involves collecting... Read moreMolecular Diagnostics
view channel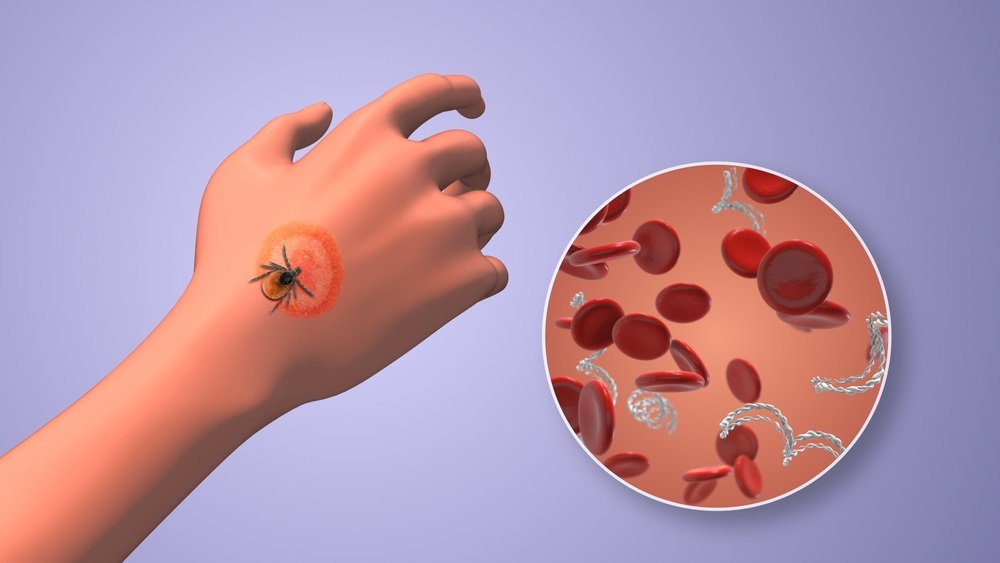
Urine Test to Revolutionize Lyme Disease Testing
Lyme disease is the most common animal-to-human transmitted disease in the United States, with around 476,000 people diagnosed and treated annually, and its incidence has been increasing.... Read more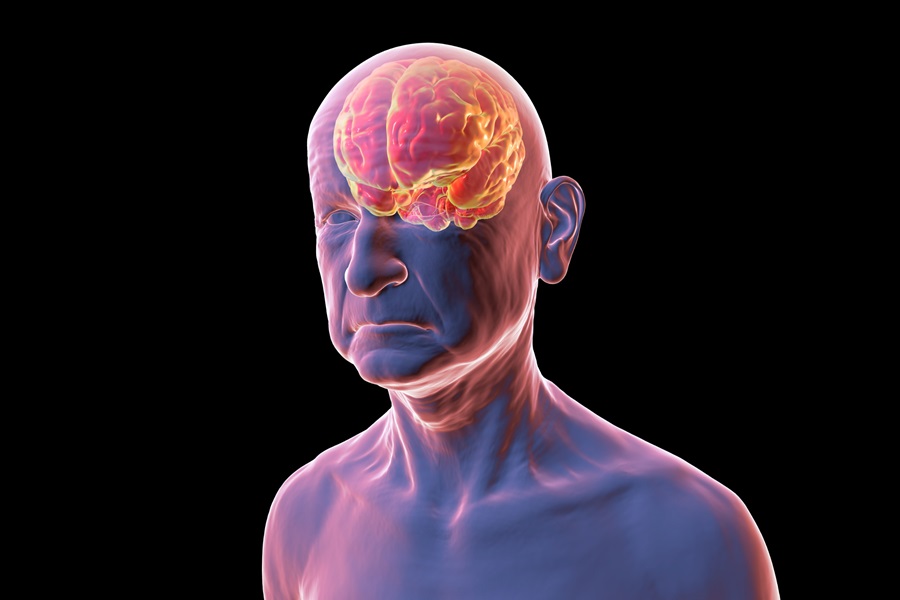
Simple Blood Test Could Enable First Quantitative Assessments for Future Cerebrovascular Disease
Cerebral small vessel disease is a common cause of stroke and cognitive decline, particularly in the elderly. Presently, assessing the risk for cerebral vascular diseases involves using a mix of diagnostic... Read more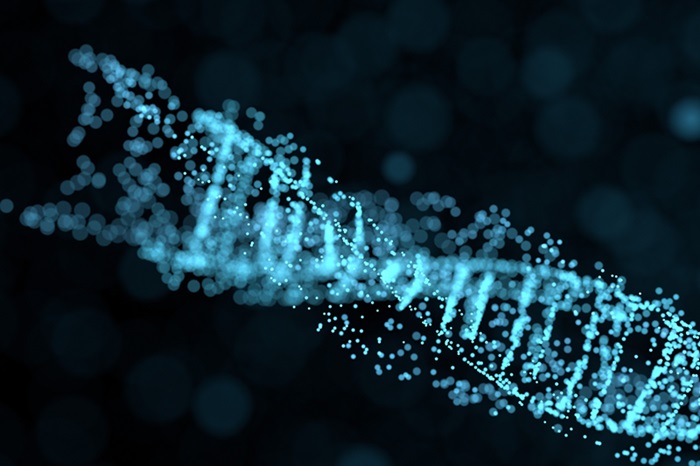
New Genetic Testing Procedure Combined With Ultrasound Detects High Cardiovascular Risk
A key interest area in cardiovascular research today is the impact of clonal hematopoiesis on cardiovascular diseases. Clonal hematopoiesis results from mutations in hematopoietic stem cells and may lead... Read moreImmunology
view channel
Diagnostic Blood Test for Cellular Rejection after Organ Transplant Could Replace Surgical Biopsies
Transplanted organs constantly face the risk of being rejected by the recipient's immune system which differentiates self from non-self using T cells and B cells. T cells are commonly associated with acute... Read more
AI Tool Precisely Matches Cancer Drugs to Patients Using Information from Each Tumor Cell
Current strategies for matching cancer patients with specific treatments often depend on bulk sequencing of tumor DNA and RNA, which provides an average profile from all cells within a tumor sample.... Read more
Genetic Testing Combined With Personalized Drug Screening On Tumor Samples to Revolutionize Cancer Treatment
Cancer treatment typically adheres to a standard of care—established, statistically validated regimens that are effective for the majority of patients. However, the disease’s inherent variability means... Read moreMicrobiology
view channelEnhanced Rapid Syndromic Molecular Diagnostic Solution Detects Broad Range of Infectious Diseases
GenMark Diagnostics (Carlsbad, CA, USA), a member of the Roche Group (Basel, Switzerland), has rebranded its ePlex® system as the cobas eplex system. This rebranding under the globally renowned cobas name... Read more
Clinical Decision Support Software a Game-Changer in Antimicrobial Resistance Battle
Antimicrobial resistance (AMR) is a serious global public health concern that claims millions of lives every year. It primarily results from the inappropriate and excessive use of antibiotics, which reduces... Read more
New CE-Marked Hepatitis Assays to Help Diagnose Infections Earlier
According to the World Health Organization (WHO), an estimated 354 million individuals globally are afflicted with chronic hepatitis B or C. These viruses are the leading causes of liver cirrhosis, liver... Read more
1 Hour, Direct-From-Blood Multiplex PCR Test Identifies 95% of Sepsis-Causing Pathogens
Sepsis contributes to one in every three hospital deaths in the US, and globally, septic shock carries a mortality rate of 30-40%. Diagnosing sepsis early is challenging due to its non-specific symptoms... Read morePathology
view channel
Robotic Blood Drawing Device to Revolutionize Sample Collection for Diagnostic Testing
Blood drawing is performed billions of times each year worldwide, playing a critical role in diagnostic procedures. Despite its importance, clinical laboratories are dealing with significant staff shortages,... Read more.jpg)
Use of DICOM Images for Pathology Diagnostics Marks Significant Step towards Standardization
Digital pathology is rapidly becoming a key aspect of modern healthcare, transforming the practice of pathology as laboratories worldwide adopt this advanced technology. Digital pathology systems allow... Read more
First of Its Kind Universal Tool to Revolutionize Sample Collection for Diagnostic Tests
The COVID pandemic has dramatically reshaped the perception of diagnostics. Post the pandemic, a groundbreaking device that combines sample collection and processing into a single, easy-to-use disposable... Read moreTechnology
view channel
New Diagnostic System Achieves PCR Testing Accuracy
While PCR tests are the gold standard of accuracy for virology testing, they come with limitations such as complexity, the need for skilled lab operators, and longer result times. They also require complex... Read more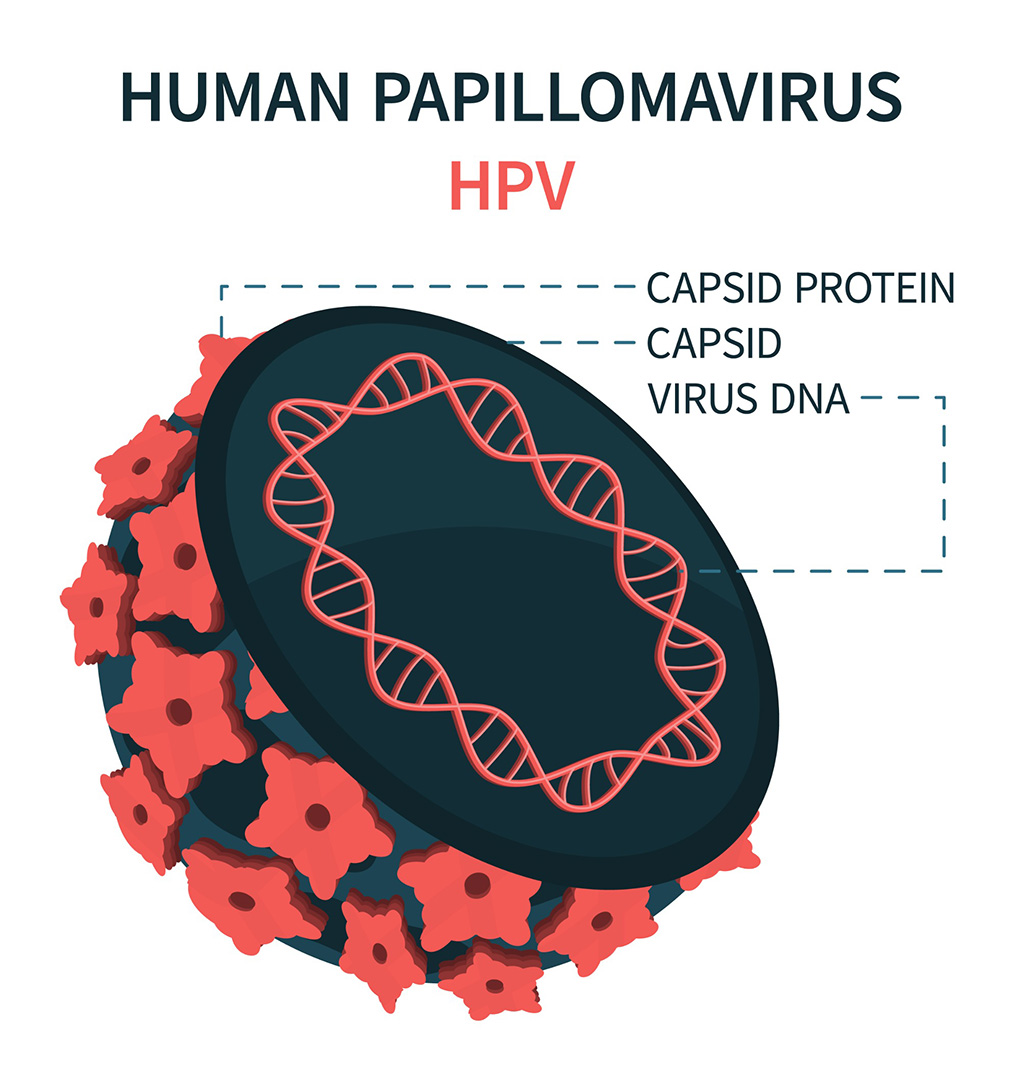
DNA Biosensor Enables Early Diagnosis of Cervical Cancer
Molybdenum disulfide (MoS2), recognized for its potential to form two-dimensional nanosheets like graphene, is a material that's increasingly catching the eye of the scientific community.... Read more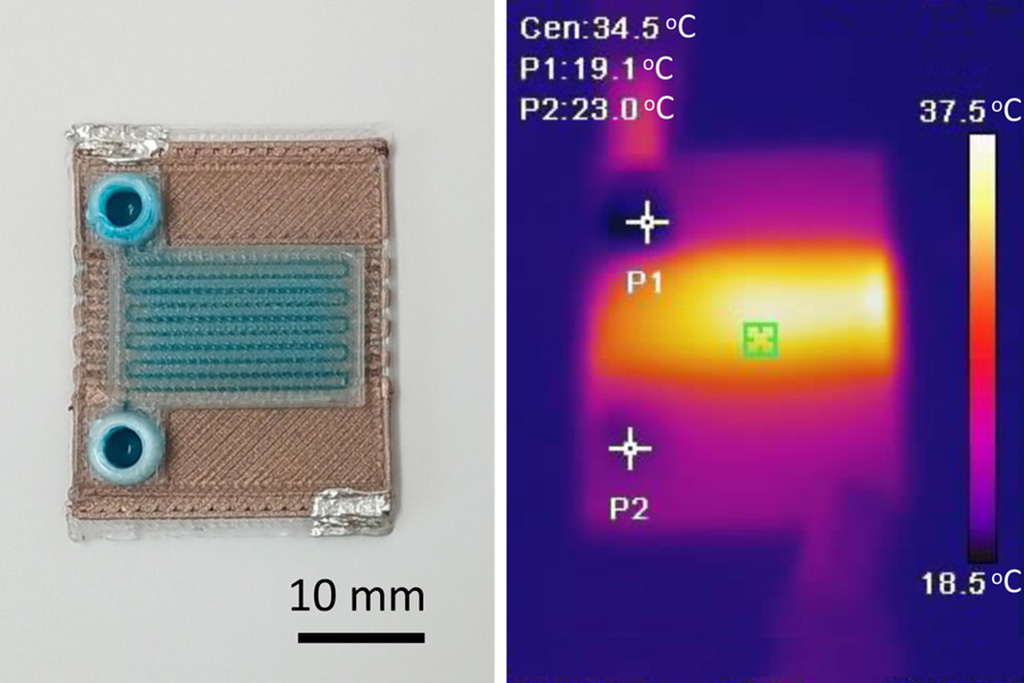
Self-Heating Microfluidic Devices Can Detect Diseases in Tiny Blood or Fluid Samples
Microfluidics, which are miniature devices that control the flow of liquids and facilitate chemical reactions, play a key role in disease detection from small samples of blood or other fluids.... Read more
Breakthrough in Diagnostic Technology Could Make On-The-Spot Testing Widely Accessible
Home testing gained significant importance during the COVID-19 pandemic, yet the availability of rapid tests is limited, and most of them can only drive one liquid across the strip, leading to continued... Read moreIndustry
view channel_1.jpg)
Thermo Fisher and Bio-Techne Enter Into Strategic Distribution Agreement for Europe
Thermo Fisher Scientific (Waltham, MA USA) has entered into a strategic distribution agreement with Bio-Techne Corporation (Minneapolis, MN, USA), resulting in a significant collaboration between two industry... Read more
ECCMID Congress Name Changes to ESCMID Global
Over the last few years, the European Society of Clinical Microbiology and Infectious Diseases (ESCMID, Basel, Switzerland) has evolved remarkably. The society is now stronger and broader than ever before... Read more