Distinct Inflammatory Profiles Distinguish COVID-19 From Influenza
|
By LabMedica International staff writers Posted on 30 Nov 2020 |

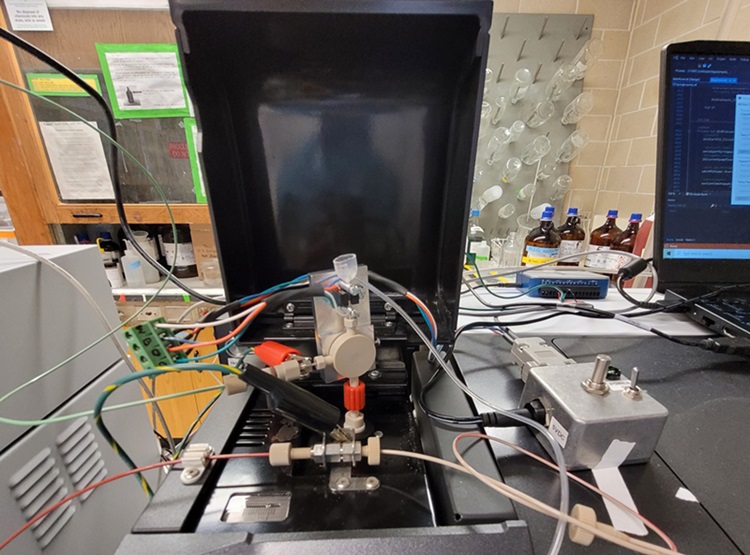
Image: The Cytek Aurora spectral flow cytometer (Photo courtesy of Cytek Bioscience).
Acute respiratory failure occurs in a subset of COVID-19 patients. Understanding the etiology of respiratory failure in COVID-19 patients is critical for determining the best management strategies and pharmacologic targets for treatment.
Cytokine storm syndrome (CSS) has been proposed as underlying the etiology of respiratory failure in patients with COVID-19. This model suggests that respiratory failure is related to significant pro-inflammatory cytokine expression that leads to inflammatory cell recruitment and tissue damage in the lung.
A team of medical scientists led by those at Washington University School of Medicine (Saint Louis, MO, USA) undertook a comparative investigation of inflammatory responses in a cohort of 79 COVID-19 patients, 26 influenza A or B patients and 16 healthy controls. Both the COVID-19 and influenza cohorts included patients with moderate disease, and severe disease, defined by individuals requiring mechanical ventilation for acute respiratory failure or who ultimately died due to their illness.
The team determined absolute counts of CD45+ cells in whole blood at the time of blood collection on fresh samples by flow cytometry with Precision Count Beads (BioLegend, San Diego, CA, USA). Peripheral blood mononuclear cells (PBMCs), prepared using Ficoll separation, were analyzed using a panel of antibodies directed against different antigens. Samples were run on a Cytek Aurora spectral flow cytometer using SpectroFlo software (Cytek Bioscience, Fremont, CA, USA).
Plasma obtained from subjects was frozen at -80 °C and subsequently analyzed using a human magnetic cytokine panel providing parallel measurement of 35 cytokines (Thermo Fisher Scientific, Waltham, MA, USA). The assay was performed with each subject sample performed in duplicate and then analyzed on a Luminex FLEXMAP 3D instrument (Luminex Corporation, Austin, TX, USA). Single-cell gene expression libraries were prepared using 5-prime (V2) kits and sequenced on the NovaSeq 6000 platform (Illumina, San Diego, CA, USA).
The scientists found that COVID-19 patients exhibited lower cytokine levels than influenza patients. Among the statistically significant reduced cytokines exhibited by COVID-19 patients compared to influenza patients were IFN-γ, MIG, IL-1RA, IL-2R, GCSF, IL-17a, IL-9, and MIP-1α. In addition, the team found that COVID-19 and influenza patients exhibited trends of decreased B cells and significant reductions in both T cell subsets, which generally constitute the majority of circulating peripheral blood mononuclear cells (PBMCs) in healthy controls. Circulating activated CD4+ and CD8+ cells were equivalent across all groups. However, when compared with either influenza patients or controls, COVID-19 patients exhibited significantly reduced numbers of circulating monocytes, including all three common classifications of human monocytes (classical, intermediate, and non-classical).
Further, COVID-19 patients were observed to have reduced abundances of HLA-DR on the surface of intermediate monocytes when compared with influenza patients or controls after controlling for covariate effects. Additionally, COVID-19 patients exhibited significantly less surface HLA-DR on CD8+ T cells than influenza patients, and trends toward less HLA-DR on CD4+ T cells in comparison to both influenza patients and healthy controls.
The authors concluded that the signatures of this common COVID-19 phenotype compared to influenza were equivalent levels of IL-6 and IL-8, paired with lower levels of cytokines in many other pathways and essentially the absence of any Type I or Type II IFN response. The study was published on November 13, 2020 in the journal Science Advances.
Related Links:
Washington University School of Medicine
BioLegend
Cytek Bioscience
Thermo Fisher Scientific
Luminex Corporation
Illumina
Cytokine storm syndrome (CSS) has been proposed as underlying the etiology of respiratory failure in patients with COVID-19. This model suggests that respiratory failure is related to significant pro-inflammatory cytokine expression that leads to inflammatory cell recruitment and tissue damage in the lung.
A team of medical scientists led by those at Washington University School of Medicine (Saint Louis, MO, USA) undertook a comparative investigation of inflammatory responses in a cohort of 79 COVID-19 patients, 26 influenza A or B patients and 16 healthy controls. Both the COVID-19 and influenza cohorts included patients with moderate disease, and severe disease, defined by individuals requiring mechanical ventilation for acute respiratory failure or who ultimately died due to their illness.
The team determined absolute counts of CD45+ cells in whole blood at the time of blood collection on fresh samples by flow cytometry with Precision Count Beads (BioLegend, San Diego, CA, USA). Peripheral blood mononuclear cells (PBMCs), prepared using Ficoll separation, were analyzed using a panel of antibodies directed against different antigens. Samples were run on a Cytek Aurora spectral flow cytometer using SpectroFlo software (Cytek Bioscience, Fremont, CA, USA).
Plasma obtained from subjects was frozen at -80 °C and subsequently analyzed using a human magnetic cytokine panel providing parallel measurement of 35 cytokines (Thermo Fisher Scientific, Waltham, MA, USA). The assay was performed with each subject sample performed in duplicate and then analyzed on a Luminex FLEXMAP 3D instrument (Luminex Corporation, Austin, TX, USA). Single-cell gene expression libraries were prepared using 5-prime (V2) kits and sequenced on the NovaSeq 6000 platform (Illumina, San Diego, CA, USA).
The scientists found that COVID-19 patients exhibited lower cytokine levels than influenza patients. Among the statistically significant reduced cytokines exhibited by COVID-19 patients compared to influenza patients were IFN-γ, MIG, IL-1RA, IL-2R, GCSF, IL-17a, IL-9, and MIP-1α. In addition, the team found that COVID-19 and influenza patients exhibited trends of decreased B cells and significant reductions in both T cell subsets, which generally constitute the majority of circulating peripheral blood mononuclear cells (PBMCs) in healthy controls. Circulating activated CD4+ and CD8+ cells were equivalent across all groups. However, when compared with either influenza patients or controls, COVID-19 patients exhibited significantly reduced numbers of circulating monocytes, including all three common classifications of human monocytes (classical, intermediate, and non-classical).
Further, COVID-19 patients were observed to have reduced abundances of HLA-DR on the surface of intermediate monocytes when compared with influenza patients or controls after controlling for covariate effects. Additionally, COVID-19 patients exhibited significantly less surface HLA-DR on CD8+ T cells than influenza patients, and trends toward less HLA-DR on CD4+ T cells in comparison to both influenza patients and healthy controls.
The authors concluded that the signatures of this common COVID-19 phenotype compared to influenza were equivalent levels of IL-6 and IL-8, paired with lower levels of cytokines in many other pathways and essentially the absence of any Type I or Type II IFN response. The study was published on November 13, 2020 in the journal Science Advances.
Related Links:
Washington University School of Medicine
BioLegend
Cytek Bioscience
Thermo Fisher Scientific
Luminex Corporation
Illumina
Latest Immunology News
- AI Predicts Tumor-Killing Cells with High Accuracy
- Diagnostic Blood Test for Cellular Rejection after Organ Transplant Could Replace Surgical Biopsies
- AI Tool Precisely Matches Cancer Drugs to Patients Using Information from Each Tumor Cell
- Genetic Testing Combined With Personalized Drug Screening On Tumor Samples to Revolutionize Cancer Treatment
- Testing Method Could Help More Patients Receive Right Cancer Treatment
- Groundbreaking Test Monitors Radiation Therapy Toxicity in Cancer Patients
- State-Of-The Art Techniques to Investigate Immune Response in Deadly Strep A Infections
- Novel Immunoassays Enable Early Diagnosis of Antiphospholipid Syndrome
- New Test Could Predict Immunotherapy Success for Broader Range Of Cancers
- Simple Blood Protein Tests Predict CAR T Outcomes for Lymphoma Patients
- Cell Sorter Chip Technology to Pave Way for Immune Profiling at POC
- Chip Monitors Cancer Cells in Blood Samples to Assess Treatment Effectiveness
- Automated Immunohematology Approaches Can Resolve Transplant Incompatibility
- AI Leverages Tumor Genetics to Predict Patient Response to Chemotherapy
- World’s First Portable, Non-Invasive WBC Monitoring Device to Eliminate Need for Blood Draw
- Predictive T-Cell Test Detects Immune Response to Viruses Even Before Antibodies Form
Channels
Clinical Chemistry
view channel
3D Printed Point-Of-Care Mass Spectrometer Outperforms State-Of-The-Art Models
Mass spectrometry is a precise technique for identifying the chemical components of a sample and has significant potential for monitoring chronic illness health states, such as measuring hormone levels... Read more.jpg)
POC Biomedical Test Spins Water Droplet Using Sound Waves for Cancer Detection
Exosomes, tiny cellular bioparticles carrying a specific set of proteins, lipids, and genetic materials, play a crucial role in cell communication and hold promise for non-invasive diagnostics.... Read more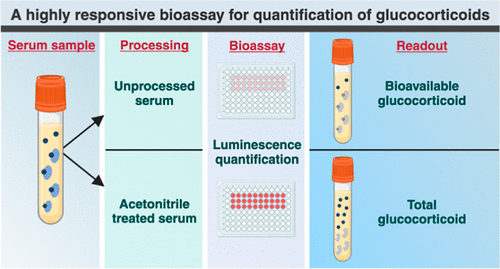
Highly Reliable Cell-Based Assay Enables Accurate Diagnosis of Endocrine Diseases
The conventional methods for measuring free cortisol, the body's stress hormone, from blood or saliva are quite demanding and require sample processing. The most common method, therefore, involves collecting... Read moreMolecular Diagnostics
view channelBlood Proteins Could Warn of Cancer Seven Years before Diagnosis
Two studies have identified proteins in the blood that could potentially alert individuals to the presence of cancer more than seven years before the disease is clinically diagnosed. Researchers found... Read moreUltrasound-Aided Blood Testing Detects Cancer Biomarkers from Cells
Ultrasound imaging serves as a noninvasive method to locate and monitor cancerous tumors effectively. However, crucial details about the cancer, such as the specific types of cells and genetic mutations... Read moreHematology
view channel
Next Generation Instrument Screens for Hemoglobin Disorders in Newborns
Hemoglobinopathies, the most widespread inherited conditions globally, affect about 7% of the population as carriers, with 2.7% of newborns being born with these conditions. The spectrum of clinical manifestations... Read more
First 4-in-1 Nucleic Acid Test for Arbovirus Screening to Reduce Risk of Transfusion-Transmitted Infections
Arboviruses represent an emerging global health threat, exacerbated by climate change and increased international travel that is facilitating their spread across new regions. Chikungunya, dengue, West... Read more
POC Finger-Prick Blood Test Determines Risk of Neutropenic Sepsis in Patients Undergoing Chemotherapy
Neutropenia, a decrease in neutrophils (a type of white blood cell crucial for fighting infections), is a frequent side effect of certain cancer treatments. This condition elevates the risk of infections,... Read more
First Affordable and Rapid Test for Beta Thalassemia Demonstrates 99% Diagnostic Accuracy
Hemoglobin disorders rank as some of the most prevalent monogenic diseases globally. Among various hemoglobin disorders, beta thalassemia, a hereditary blood disorder, affects about 1.5% of the world's... Read moreMicrobiology
view channel
Integrated Solution Ushers New Era of Automated Tuberculosis Testing
Tuberculosis (TB) is responsible for 1.3 million deaths every year, positioning it as one of the top killers globally due to a single infectious agent. In 2022, around 10.6 million people were diagnosed... Read more
Automated Sepsis Test System Enables Rapid Diagnosis for Patients with Severe Bloodstream Infections
Sepsis affects up to 50 million people globally each year, with bacteraemia, formerly known as blood poisoning, being a major cause. In the United States alone, approximately two million individuals are... Read moreEnhanced Rapid Syndromic Molecular Diagnostic Solution Detects Broad Range of Infectious Diseases
GenMark Diagnostics (Carlsbad, CA, USA), a member of the Roche Group (Basel, Switzerland), has rebranded its ePlex® system as the cobas eplex system. This rebranding under the globally renowned cobas name... Read more
Clinical Decision Support Software a Game-Changer in Antimicrobial Resistance Battle
Antimicrobial resistance (AMR) is a serious global public health concern that claims millions of lives every year. It primarily results from the inappropriate and excessive use of antibiotics, which reduces... Read morePathology
view channel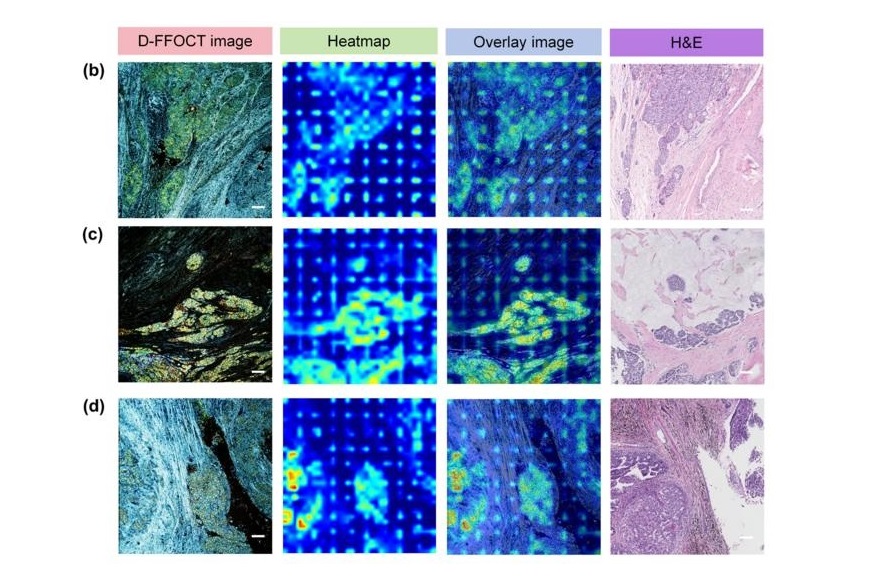
AI Integrated With Optical Imaging Technology Enables Rapid Intraoperative Diagnosis
Rapid and accurate intraoperative diagnosis is essential for tumor surgery as it guides surgical decisions with precision. Traditional intraoperative assessments, such as frozen sections based on H&E... Read more
HPV Self-Collection Solution Improves Access to Cervical Cancer Testing
Annually, over 604,000 women across the world are diagnosed with cervical cancer, and about 342,000 die from this disease, which is preventable and primarily caused by the Human Papillomavirus (HPV).... Read moreHyperspectral Dark-Field Microscopy Enables Rapid and Accurate Identification of Cancerous Tissues
Breast cancer remains a major cause of cancer-related mortality among women. Breast-conserving surgery (BCS), also known as lumpectomy, is the removal of the cancerous lump and a small margin of surrounding tissue.... Read moreTechnology
view channel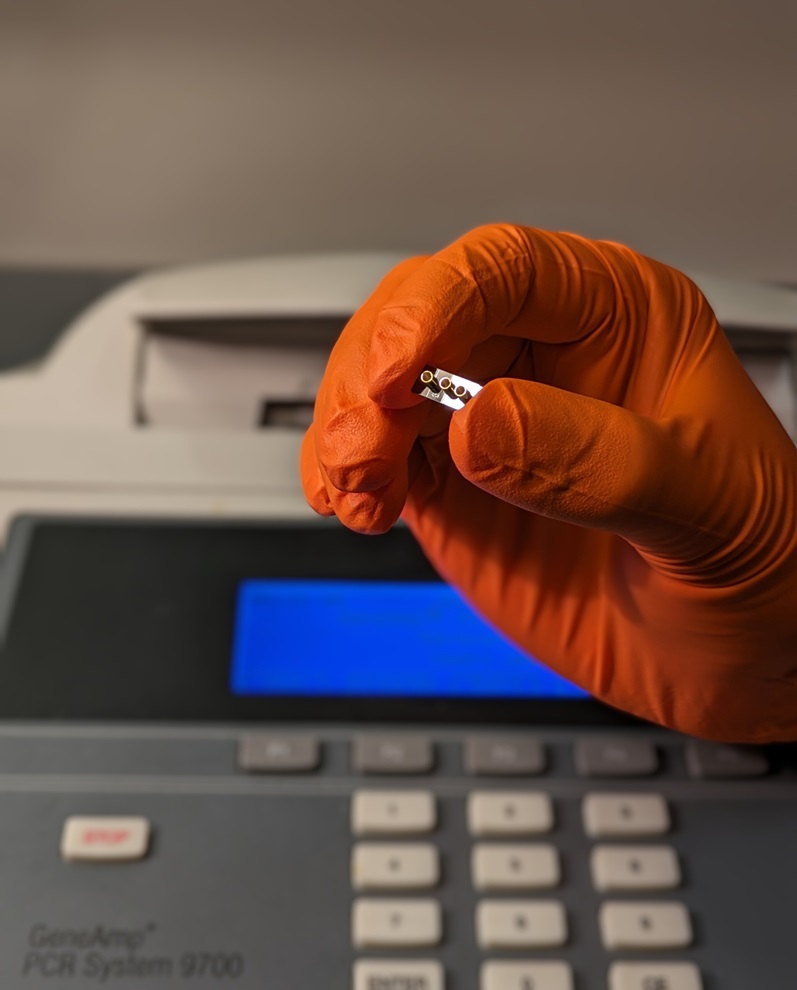
New Diagnostic System Achieves PCR Testing Accuracy
While PCR tests are the gold standard of accuracy for virology testing, they come with limitations such as complexity, the need for skilled lab operators, and longer result times. They also require complex... Read more
DNA Biosensor Enables Early Diagnosis of Cervical Cancer
Molybdenum disulfide (MoS2), recognized for its potential to form two-dimensional nanosheets like graphene, is a material that's increasingly catching the eye of the scientific community.... Read more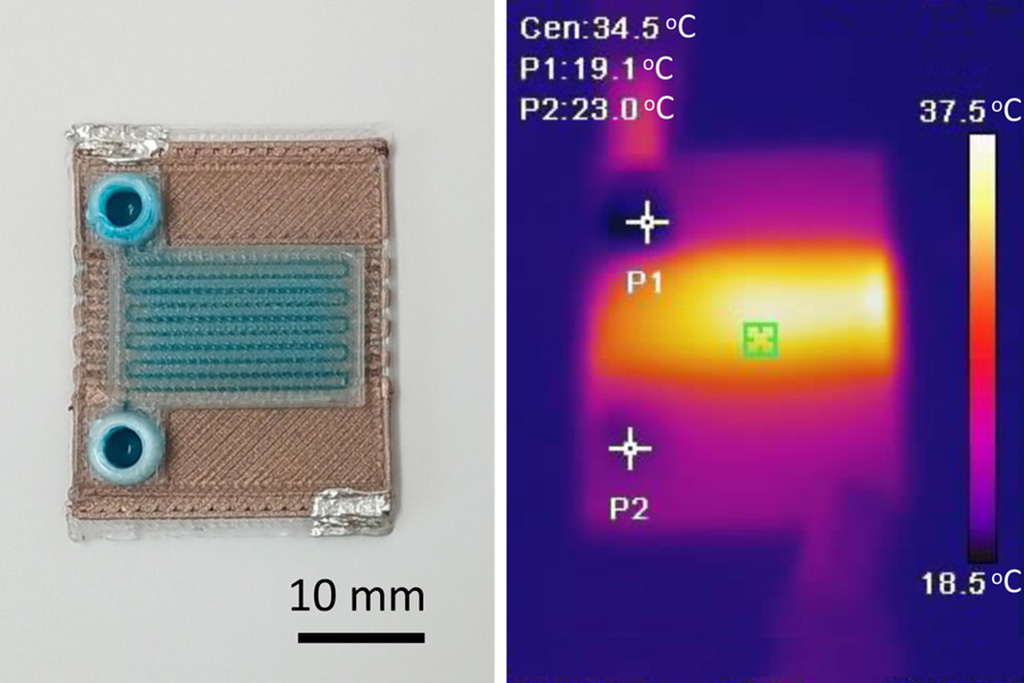
Self-Heating Microfluidic Devices Can Detect Diseases in Tiny Blood or Fluid Samples
Microfluidics, which are miniature devices that control the flow of liquids and facilitate chemical reactions, play a key role in disease detection from small samples of blood or other fluids.... Read more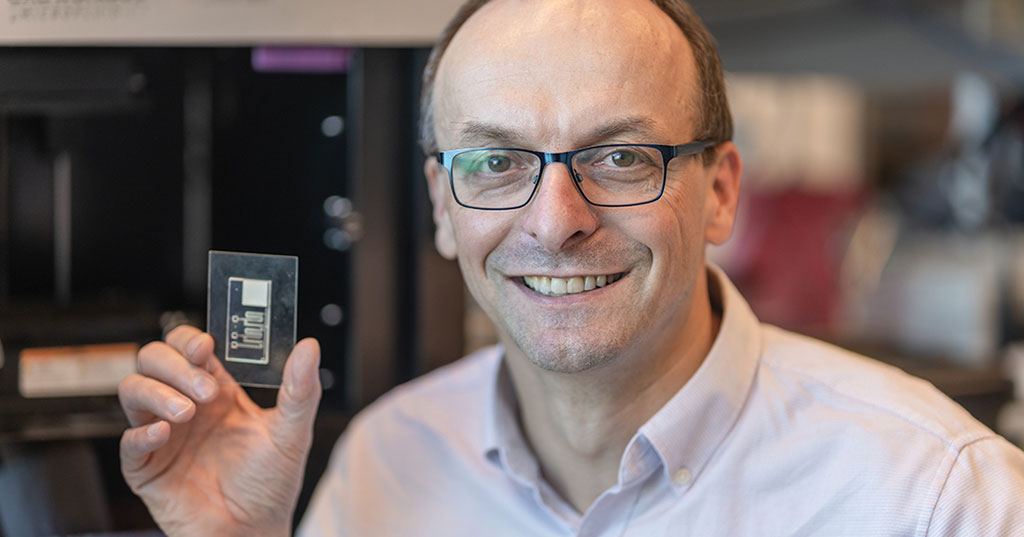
Breakthrough in Diagnostic Technology Could Make On-The-Spot Testing Widely Accessible
Home testing gained significant importance during the COVID-19 pandemic, yet the availability of rapid tests is limited, and most of them can only drive one liquid across the strip, leading to continued... Read moreIndustry
view channel
Danaher and Johns Hopkins University Collaborate to Improve Neurological Diagnosis
Unlike severe traumatic brain injury (TBI), mild TBI often does not show clear correlations with abnormalities detected through head computed tomography (CT) scans. Consequently, there is a pressing need... Read more
Beckman Coulter and MeMed Expand Host Immune Response Diagnostics Partnership
Beckman Coulter Diagnostics (Brea, CA, USA) and MeMed BV (Haifa, Israel) have expanded their host immune response diagnostics partnership. Beckman Coulter is now an authorized distributor of the MeMed... Read more_1.jpg)











_1.jpg)
.jpg)