Saliva Specimens Diagnose Respiratory Virus by POC Assay
|
By LabMedica International staff writers Posted on 05 Jul 2018 |

Image: The Xpert Xpress Flu/RSV Assay Cassette (Photo courtesy of Cepheid).
The use of saliva as a specimen for the detection of respiratory viruses has been proposed as an alternative to nasopharyngeal aspirate or nasopharyngeal swab: saliva may have the advantage to cause less discomfort in patients and less risk for healthcare workers.
Automated point-of-care molecular assays have greatly shortened the turnaround time of respiratory virus testing. One of the major bottlenecks now lies at the step of the specimen collection especially in a busy clinical setting. Saliva is a convenient specimen type, which can be provided easily from adult patients.
Scientists from the University of Hong Kong (Pokfulam, Hong Kong) recruited between July and October 2017, 214 patients and carried out a prospective diagnostic validity study comparing the detection rate of respiratory viruses between saliva and nasopharyngeal aspirate (NPA) among adult hospitalized patients using Xpert Xpress Flu/RSV. The cost and time associated with the collection of saliva and nasopharyngeal specimens were also estimated.
The team found that the overall agreement between saliva and NPA were 93.3% (196/210). There was no significant difference in the detection rate of respiratory viruses between saliva and NPA; (69/210 (32.9%) versus 75/210 (35.7%). The overall sensitivity and specificity were 90.8% (81.9-96.2%) and 100% (97.3-100%), respectively, for saliva, and were 96.1% (88.9-99.2%) and 98.5% (94.7-99.8%), respectively, for NPA. The time and cost associated with the collection of saliva were 2.3-fold and 2.6-fold lower, respectively, than those of NPA.
The authors concluded that saliva specimen had high sensitivity and specificity in the detection of respiratory viruses by an automated multiplex Clinical Laboratory Improvement Amendments (CLIA)-waived point-of-care molecular assay when compared with that of NPA. The use of saliva also reduces the time and cost associated with specimen collection. The study was published on June 12, 2018, in the journal Clinical Microbiology and Infection.
Related Links:
University of Hong Kong
Automated point-of-care molecular assays have greatly shortened the turnaround time of respiratory virus testing. One of the major bottlenecks now lies at the step of the specimen collection especially in a busy clinical setting. Saliva is a convenient specimen type, which can be provided easily from adult patients.
Scientists from the University of Hong Kong (Pokfulam, Hong Kong) recruited between July and October 2017, 214 patients and carried out a prospective diagnostic validity study comparing the detection rate of respiratory viruses between saliva and nasopharyngeal aspirate (NPA) among adult hospitalized patients using Xpert Xpress Flu/RSV. The cost and time associated with the collection of saliva and nasopharyngeal specimens were also estimated.
The team found that the overall agreement between saliva and NPA were 93.3% (196/210). There was no significant difference in the detection rate of respiratory viruses between saliva and NPA; (69/210 (32.9%) versus 75/210 (35.7%). The overall sensitivity and specificity were 90.8% (81.9-96.2%) and 100% (97.3-100%), respectively, for saliva, and were 96.1% (88.9-99.2%) and 98.5% (94.7-99.8%), respectively, for NPA. The time and cost associated with the collection of saliva were 2.3-fold and 2.6-fold lower, respectively, than those of NPA.
The authors concluded that saliva specimen had high sensitivity and specificity in the detection of respiratory viruses by an automated multiplex Clinical Laboratory Improvement Amendments (CLIA)-waived point-of-care molecular assay when compared with that of NPA. The use of saliva also reduces the time and cost associated with specimen collection. The study was published on June 12, 2018, in the journal Clinical Microbiology and Infection.
Related Links:
University of Hong Kong
Latest Technology News
- New Diagnostic System Achieves PCR Testing Accuracy
- DNA Biosensor Enables Early Diagnosis of Cervical Cancer
- Self-Heating Microfluidic Devices Can Detect Diseases in Tiny Blood or Fluid Samples
- Breakthrough in Diagnostic Technology Could Make On-The-Spot Testing Widely Accessible
- First of Its Kind Technology Detects Glucose in Human Saliva
- Electrochemical Device Identifies People at Higher Risk for Osteoporosis Using Single Blood Drop
- Novel Noninvasive Test Detects Malaria Infection without Blood Sample
- Portable Optofluidic Sensing Devices Could Simultaneously Perform Variety of Medical Tests
- Point-of-Care Software Solution Helps Manage Disparate POCT Scenarios across Patient Testing Locations
- Electronic Biosensor Detects Biomarkers in Whole Blood Samples without Addition of Reagents
- Breakthrough Test Detects Biological Markers Related to Wider Variety of Cancers
- Rapid POC Sensing Kit to Determine Gut Health from Blood Serum and Stool Samples
- Device Converts Smartphone into Fluorescence Microscope for Just USD 50
- Wi-Fi Enabled Handheld Tube Reader Designed for Easy Portability
Channels
Clinical Chemistry
view channel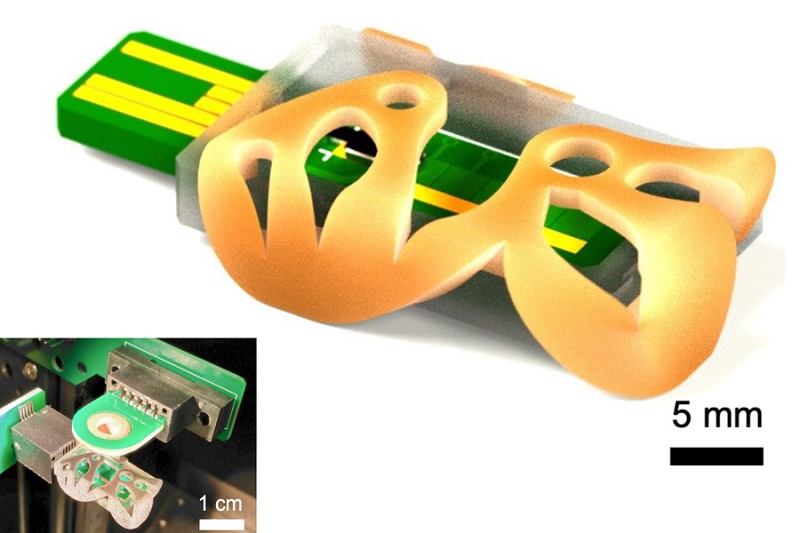
3D Printed Point-Of-Care Mass Spectrometer Outperforms State-Of-The-Art Models
Mass spectrometry is a precise technique for identifying the chemical components of a sample and has significant potential for monitoring chronic illness health states, such as measuring hormone levels... Read more.jpg)
POC Biomedical Test Spins Water Droplet Using Sound Waves for Cancer Detection
Exosomes, tiny cellular bioparticles carrying a specific set of proteins, lipids, and genetic materials, play a crucial role in cell communication and hold promise for non-invasive diagnostics.... Read more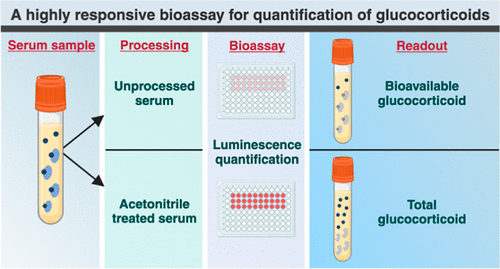
Highly Reliable Cell-Based Assay Enables Accurate Diagnosis of Endocrine Diseases
The conventional methods for measuring free cortisol, the body's stress hormone, from blood or saliva are quite demanding and require sample processing. The most common method, therefore, involves collecting... Read moreMolecular Diagnostics
view channelBlood Proteins Could Warn of Cancer Seven Years before Diagnosis
Two studies have identified proteins in the blood that could potentially alert individuals to the presence of cancer more than seven years before the disease is clinically diagnosed. Researchers found... Read moreUltrasound-Aided Blood Testing Detects Cancer Biomarkers from Cells
Ultrasound imaging serves as a noninvasive method to locate and monitor cancerous tumors effectively. However, crucial details about the cancer, such as the specific types of cells and genetic mutations... Read moreHematology
view channel
Next Generation Instrument Screens for Hemoglobin Disorders in Newborns
Hemoglobinopathies, the most widespread inherited conditions globally, affect about 7% of the population as carriers, with 2.7% of newborns being born with these conditions. The spectrum of clinical manifestations... Read more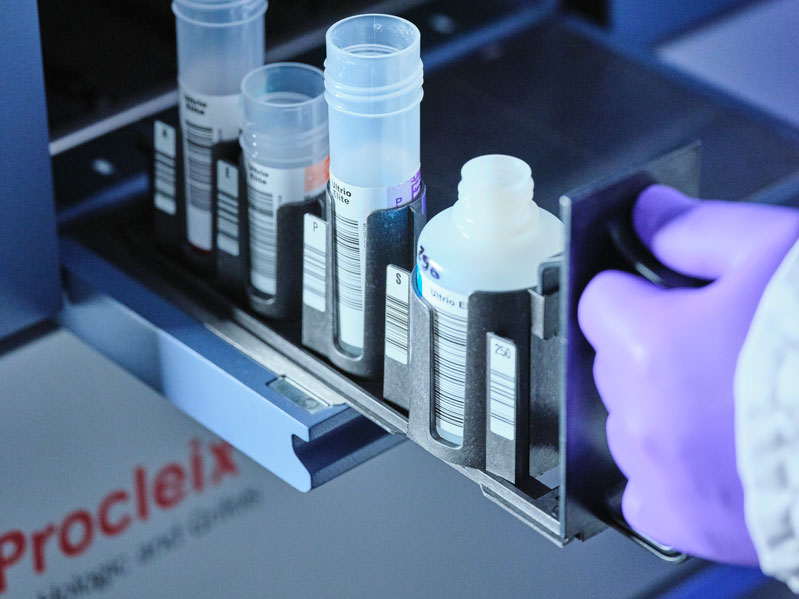
First 4-in-1 Nucleic Acid Test for Arbovirus Screening to Reduce Risk of Transfusion-Transmitted Infections
Arboviruses represent an emerging global health threat, exacerbated by climate change and increased international travel that is facilitating their spread across new regions. Chikungunya, dengue, West... Read more
POC Finger-Prick Blood Test Determines Risk of Neutropenic Sepsis in Patients Undergoing Chemotherapy
Neutropenia, a decrease in neutrophils (a type of white blood cell crucial for fighting infections), is a frequent side effect of certain cancer treatments. This condition elevates the risk of infections,... Read more
First Affordable and Rapid Test for Beta Thalassemia Demonstrates 99% Diagnostic Accuracy
Hemoglobin disorders rank as some of the most prevalent monogenic diseases globally. Among various hemoglobin disorders, beta thalassemia, a hereditary blood disorder, affects about 1.5% of the world's... Read moreImmunology
view channel.jpg)
AI Predicts Tumor-Killing Cells with High Accuracy
Cellular immunotherapy involves extracting immune cells from a patient's tumor, potentially enhancing their cancer-fighting capabilities through engineering, and then expanding and reintroducing them into the body.... Read more
Diagnostic Blood Test for Cellular Rejection after Organ Transplant Could Replace Surgical Biopsies
Transplanted organs constantly face the risk of being rejected by the recipient's immune system which differentiates self from non-self using T cells and B cells. T cells are commonly associated with acute... Read more
AI Tool Precisely Matches Cancer Drugs to Patients Using Information from Each Tumor Cell
Current strategies for matching cancer patients with specific treatments often depend on bulk sequencing of tumor DNA and RNA, which provides an average profile from all cells within a tumor sample.... Read more
Genetic Testing Combined With Personalized Drug Screening On Tumor Samples to Revolutionize Cancer Treatment
Cancer treatment typically adheres to a standard of care—established, statistically validated regimens that are effective for the majority of patients. However, the disease’s inherent variability means... Read morePathology
view channel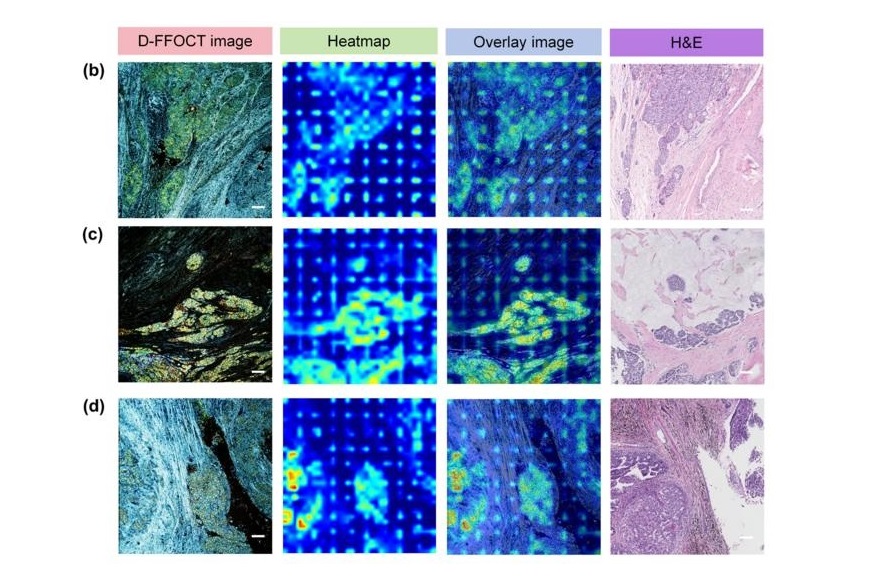
AI Integrated With Optical Imaging Technology Enables Rapid Intraoperative Diagnosis
Rapid and accurate intraoperative diagnosis is essential for tumor surgery as it guides surgical decisions with precision. Traditional intraoperative assessments, such as frozen sections based on H&E... Read more
HPV Self-Collection Solution Improves Access to Cervical Cancer Testing
Annually, over 604,000 women across the world are diagnosed with cervical cancer, and about 342,000 die from this disease, which is preventable and primarily caused by the Human Papillomavirus (HPV).... Read moreHyperspectral Dark-Field Microscopy Enables Rapid and Accurate Identification of Cancerous Tissues
Breast cancer remains a major cause of cancer-related mortality among women. Breast-conserving surgery (BCS), also known as lumpectomy, is the removal of the cancerous lump and a small margin of surrounding tissue.... Read moreTechnology
view channel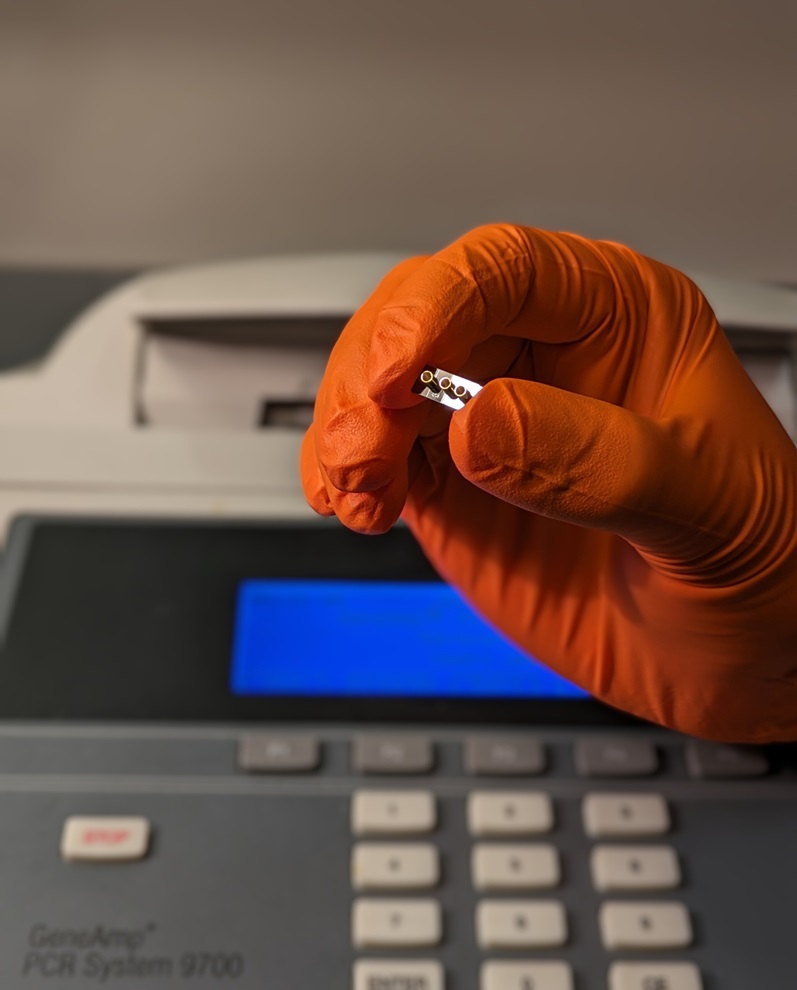
New Diagnostic System Achieves PCR Testing Accuracy
While PCR tests are the gold standard of accuracy for virology testing, they come with limitations such as complexity, the need for skilled lab operators, and longer result times. They also require complex... Read more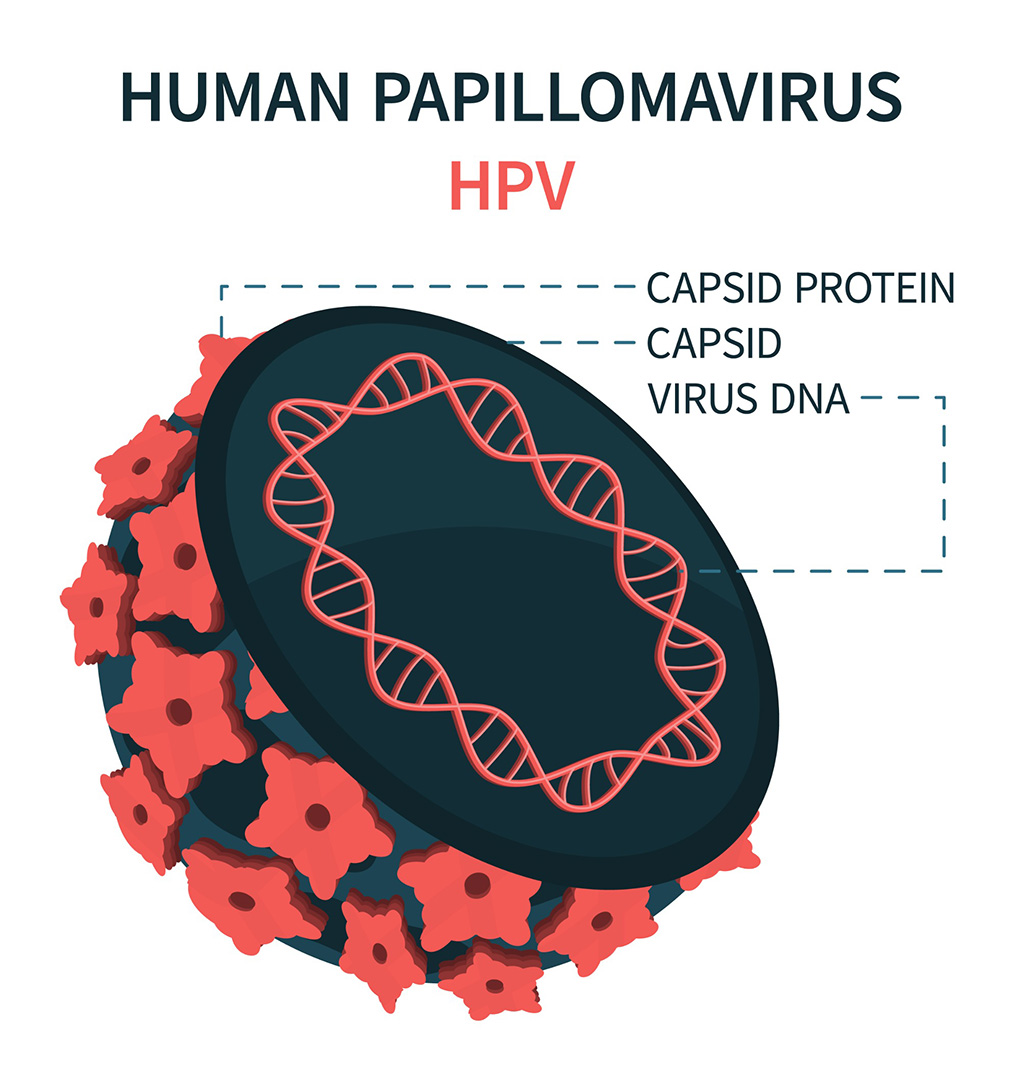
DNA Biosensor Enables Early Diagnosis of Cervical Cancer
Molybdenum disulfide (MoS2), recognized for its potential to form two-dimensional nanosheets like graphene, is a material that's increasingly catching the eye of the scientific community.... Read more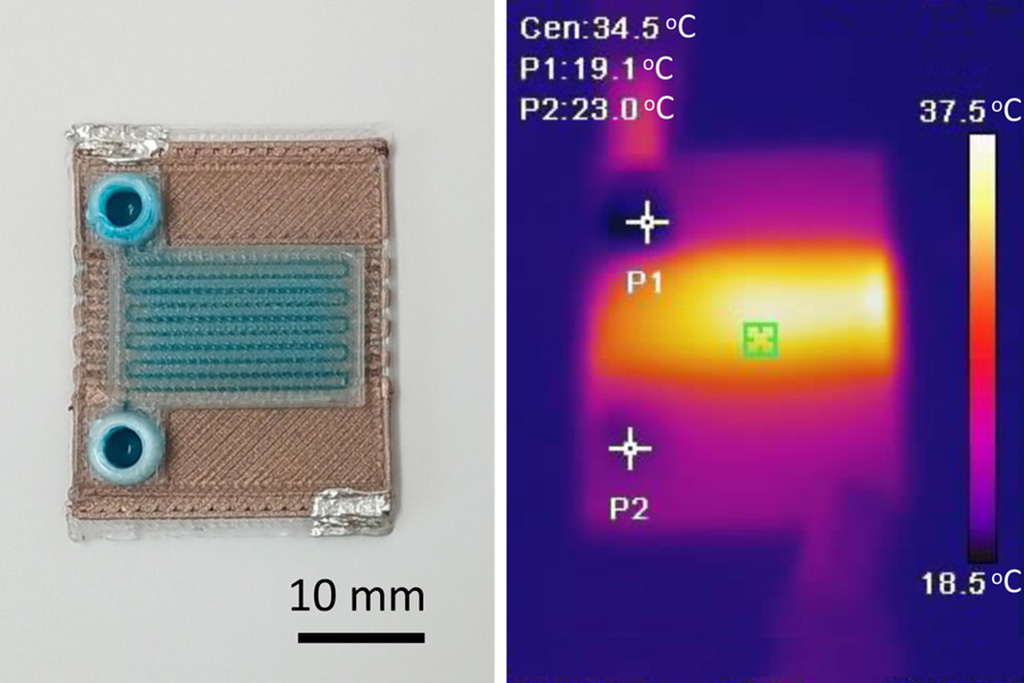
Self-Heating Microfluidic Devices Can Detect Diseases in Tiny Blood or Fluid Samples
Microfluidics, which are miniature devices that control the flow of liquids and facilitate chemical reactions, play a key role in disease detection from small samples of blood or other fluids.... Read more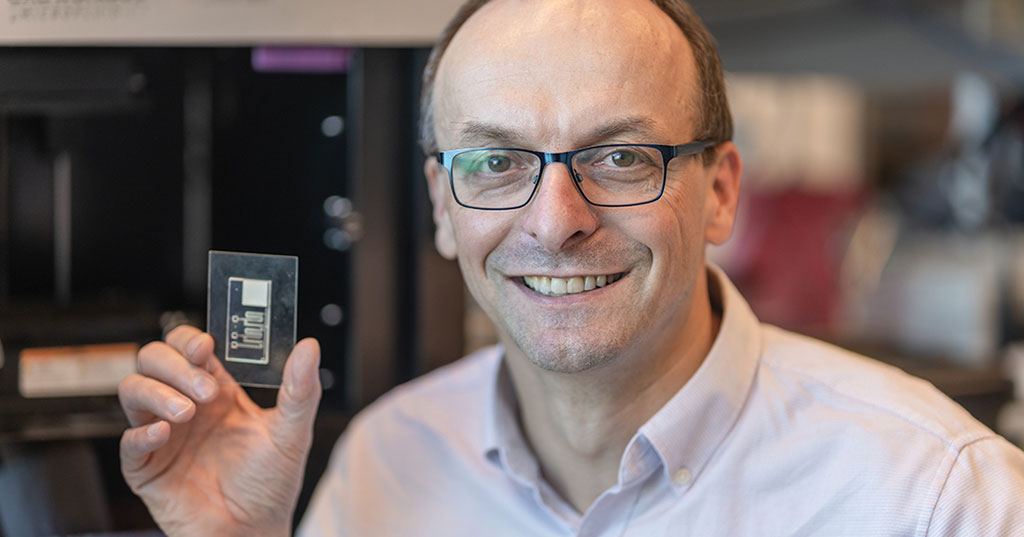
Breakthrough in Diagnostic Technology Could Make On-The-Spot Testing Widely Accessible
Home testing gained significant importance during the COVID-19 pandemic, yet the availability of rapid tests is limited, and most of them can only drive one liquid across the strip, leading to continued... Read moreIndustry
view channel
Danaher and Johns Hopkins University Collaborate to Improve Neurological Diagnosis
Unlike severe traumatic brain injury (TBI), mild TBI often does not show clear correlations with abnormalities detected through head computed tomography (CT) scans. Consequently, there is a pressing need... Read more
Beckman Coulter and MeMed Expand Host Immune Response Diagnostics Partnership
Beckman Coulter Diagnostics (Brea, CA, USA) and MeMed BV (Haifa, Israel) have expanded their host immune response diagnostics partnership. Beckman Coulter is now an authorized distributor of the MeMed... Read more_1.jpg)











_1.jpg)
.jpg)