Blood-Based Markers Tied to Brain Cell and Memory Loss
|
By LabMedica International staff writers Posted on 27 Apr 2021 |
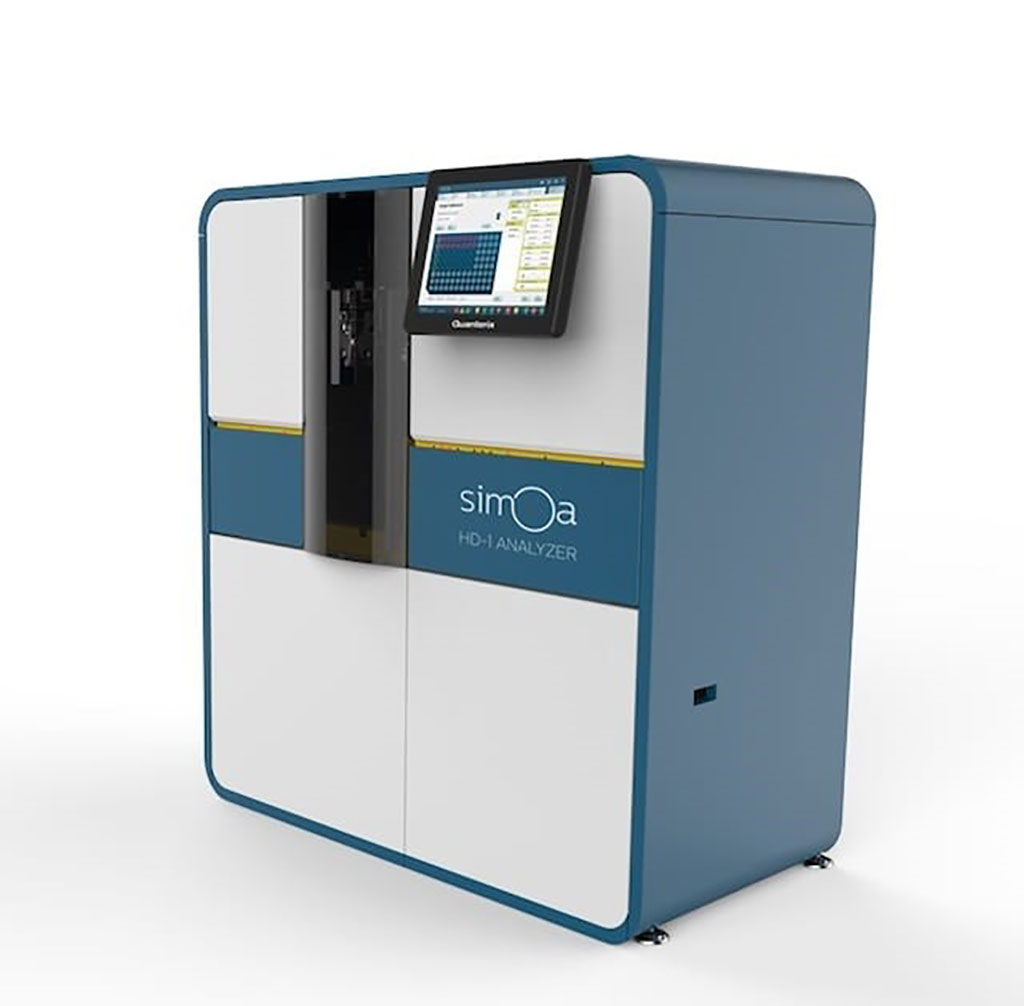
Image: The Simoa HD-1 Analyzer (Photo courtesy of Quanterix)
Previous studies have linked elevated levels of plasma total tau and neurofilament light chain (NfL) with worse cognition and neuroimaging measures of cortical thickness, cortical atrophy, white matter hyperintensity, or white matter integrity.
Neurodegeneration, or brain cell loss, is characteristic of many disorders including Alzheimer's disease, vascular dementia, and Lewy body dementia. Causes and location of neurodegeneration in the brain vary with disease. In Alzheimer's disease, amyloid plaques and neurofibrillary tangles contribute to neurodegeneration and there tends to initially be more brain cell loss in the temporal lobe. In vascular-related cognitive impairment, infarct, white matter hyperintensities, and microbleeds can contribute to cognitive changes.
Neurologists at the Mayo Clinic (Rochester, MN) and their colleagues included 995 participants without dementia who were enrolled in the Mayo Clinic Study on Aging. All had concurrent plasma NfL and Total-tau, cognitive status, and neuroimaging data. Follow-up was repeated approximately every 15 months for a median of 6.2 years. Plasma NfL and T-tau were measured on the Simoa HD-1 Platform (Quanterix, Billerica, MA, USA).
The scientists reported that baseline plasma NfL, compared to T-tau, was more strongly associated with cognitive and neuroimaging outcomes in all analyses. The combination of having both elevated NfL and T-tau at baseline, however, was more strongly associated at cross-section with worse global cognition and memory and with neuroimaging measures including temporal cortex thickness and increased number of infarcts. Longitudinally, T-tau did not add to the prognostic value of NfL. Analyses using Alzheimer's Disease Neuroimaging Initiative (ADNI) had similar result.
Michelle M. Mielke, PhD, a Professor and a senior author of the study, said, “For prognosis purposes, neurofilament light better predicted the rate of neurodegeneration and cognitive decline, regardless of what the cause of neurodegeneration might be. NfL also may help determine how fast someone declines and how effective future therapies might be in slowing this decline.”
The authors concluded that overall, plasma NfL had better utility as a prognostic marker of cognitive decline and neuroimaging changes. Plasma T-tau adds cross-sectional value to NfL in specific contexts. The study was presented on April 18, 2021 at the American Academy of Neurology annual meeting.
Related Links:
Mayo Clinic
Quanterix
Neurodegeneration, or brain cell loss, is characteristic of many disorders including Alzheimer's disease, vascular dementia, and Lewy body dementia. Causes and location of neurodegeneration in the brain vary with disease. In Alzheimer's disease, amyloid plaques and neurofibrillary tangles contribute to neurodegeneration and there tends to initially be more brain cell loss in the temporal lobe. In vascular-related cognitive impairment, infarct, white matter hyperintensities, and microbleeds can contribute to cognitive changes.
Neurologists at the Mayo Clinic (Rochester, MN) and their colleagues included 995 participants without dementia who were enrolled in the Mayo Clinic Study on Aging. All had concurrent plasma NfL and Total-tau, cognitive status, and neuroimaging data. Follow-up was repeated approximately every 15 months for a median of 6.2 years. Plasma NfL and T-tau were measured on the Simoa HD-1 Platform (Quanterix, Billerica, MA, USA).
The scientists reported that baseline plasma NfL, compared to T-tau, was more strongly associated with cognitive and neuroimaging outcomes in all analyses. The combination of having both elevated NfL and T-tau at baseline, however, was more strongly associated at cross-section with worse global cognition and memory and with neuroimaging measures including temporal cortex thickness and increased number of infarcts. Longitudinally, T-tau did not add to the prognostic value of NfL. Analyses using Alzheimer's Disease Neuroimaging Initiative (ADNI) had similar result.
Michelle M. Mielke, PhD, a Professor and a senior author of the study, said, “For prognosis purposes, neurofilament light better predicted the rate of neurodegeneration and cognitive decline, regardless of what the cause of neurodegeneration might be. NfL also may help determine how fast someone declines and how effective future therapies might be in slowing this decline.”
The authors concluded that overall, plasma NfL had better utility as a prognostic marker of cognitive decline and neuroimaging changes. Plasma T-tau adds cross-sectional value to NfL in specific contexts. The study was presented on April 18, 2021 at the American Academy of Neurology annual meeting.
Related Links:
Mayo Clinic
Quanterix
Latest Clinical Chem. News
- New PSA-Based Prognostic Model Improves Prostate Cancer Risk Assessment
- Extracellular Vesicles Linked to Heart Failure Risk in CKD Patients
- Study Compares Analytical Performance of Quantitative Hepatitis B Surface Antigen Assays
- Blood Test Could Predict and Identify Early Relapses in Myeloma Patients
- Compact Raman Imaging System Detects Subtle Tumor Signals
- Noninvasive Blood-Glucose Monitoring to Replace Finger Pricks for Diabetics
- POC Breath Diagnostic System to Detect Pneumonia-Causing Pathogens
- Online Tool Detects Drug Exposure Directly from Patient Samples
- Chemical Imaging Probe Could Track and Treat Prostate Cancer
- Mismatch Between Two Common Kidney Function Tests Indicates Serious Health Problems
- VOCs Show Promise for Early Multi-Cancer Detection
- Portable Raman Spectroscopy Offers Cost-Effective Kidney Disease Diagnosis at POC
- Gold Nanoparticles to Improve Accuracy of Ovarian Cancer Diagnosis
- Simultaneous Cell Isolation Technology Improves Cancer Diagnostic Accuracy
- Simple Non-Invasive Hair-Based Test Could Speed ALS Diagnosis
- Paper Strip Saliva Test Detects Elevated Uric Acid Levels Without Blood Draws
Channels
Molecular Diagnostics
view channel
Diagnostic Device Predicts Treatment Response for Brain Tumors Via Blood Test
Glioblastoma is one of the deadliest forms of brain cancer, largely because doctors have no reliable way to determine whether treatments are working in real time. Assessing therapeutic response currently... Read more
Blood Test Detects Early-Stage Cancers by Measuring Epigenetic Instability
Early-stage cancers are notoriously difficult to detect because molecular changes are subtle and often missed by existing screening tools. Many liquid biopsies rely on measuring absolute DNA methylation... Read more
“Lab-On-A-Disc” Device Paves Way for More Automated Liquid Biopsies
Extracellular vesicles (EVs) are tiny particles released by cells into the bloodstream that carry molecular information about a cell’s condition, including whether it is cancerous. However, EVs are highly... Read more
Blood Test Identifies Inflammatory Breast Cancer Patients at Increased Risk of Brain Metastasis
Brain metastasis is a frequent and devastating complication in patients with inflammatory breast cancer, an aggressive subtype with limited treatment options. Despite its high incidence, the biological... Read moreHematology
view channel
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read more
Fast and Easy Test Could Revolutionize Blood Transfusions
Blood transfusions are a cornerstone of modern medicine, yet red blood cells can deteriorate quietly while sitting in cold storage for weeks. Although blood units have a fixed expiration date, cells from... Read more
Automated Hemostasis System Helps Labs of All Sizes Optimize Workflow
High-volume hemostasis sections must sustain rapid turnaround while managing reruns and reflex testing. Manual tube handling and preanalytical checks can strain staff time and increase opportunities for error.... Read more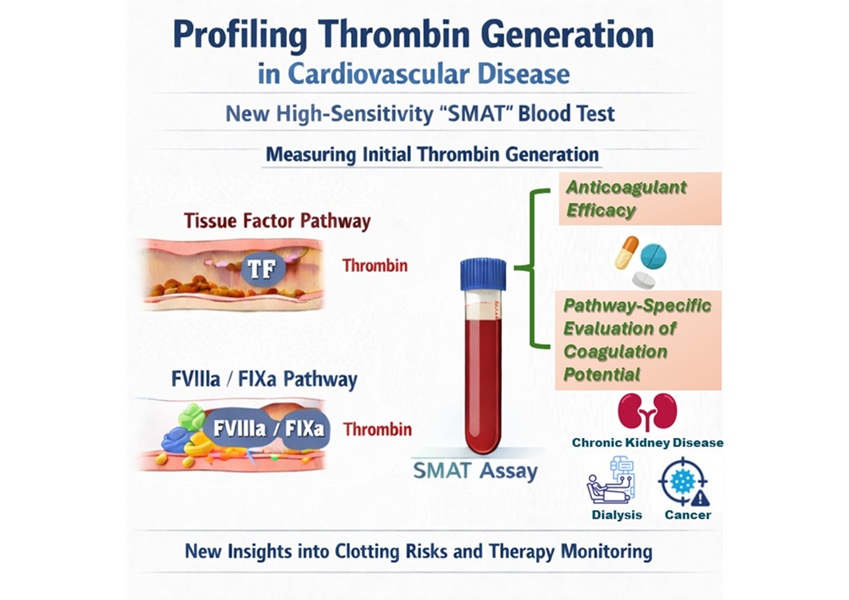
High-Sensitivity Blood Test Improves Assessment of Clotting Risk in Heart Disease Patients
Blood clotting is essential for preventing bleeding, but even small imbalances can lead to serious conditions such as thrombosis or dangerous hemorrhage. In cardiovascular disease, clinicians often struggle... Read moreImmunology
view channelBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read more
Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
Immunotherapy has transformed cancer treatment, but only a small proportion of patients experience lasting benefit, with response rates often remaining between 10% and 20%. Clinicians currently lack reliable... Read moreMicrobiology
view channel
Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
Alzheimer’s disease affects approximately 6.7 million people in the United States and nearly 50 million worldwide, yet early cognitive decline remains difficult to characterize. Increasing evidence suggests... Read moreAI-Powered Platform Enables Rapid Detection of Drug-Resistant C. Auris Pathogens
Infections caused by the pathogenic yeast Candida auris pose a significant threat to hospitalized patients, particularly those with weakened immune systems or those who have invasive medical devices.... Read morePathology
view channel
Engineered Yeast Cells Enable Rapid Testing of Cancer Immunotherapy
Developing new cancer immunotherapies is a slow, costly, and high-risk process, particularly for CAR T cell treatments that must precisely recognize cancer-specific antigens. Small differences in tumor... Read more
First-Of-Its-Kind Test Identifies Autism Risk at Birth
Autism spectrum disorder is treatable, and extensive research shows that early intervention can significantly improve cognitive, social, and behavioral outcomes. Yet in the United States, the average age... Read moreTechnology
view channel
Robotic Technology Unveiled for Automated Diagnostic Blood Draws
Routine diagnostic blood collection is a high‑volume task that can strain staffing and introduce human‑dependent variability, with downstream implications for sample quality and patient experience.... Read more
ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
Clinical laboratories generate billions of test results each year, creating a treasure trove of data with the potential to support more personalized testing, improve operational efficiency, and enhance patient care.... Read moreAptamer Biosensor Technology to Transform Virus Detection
Rapid and reliable virus detection is essential for controlling outbreaks, from seasonal influenza to global pandemics such as COVID-19. Conventional diagnostic methods, including cell culture, antigen... Read more
AI Models Could Predict Pre-Eclampsia and Anemia Earlier Using Routine Blood Tests
Pre-eclampsia and anemia are major contributors to maternal and child mortality worldwide, together accounting for more than half a million deaths each year and leaving millions with long-term health complications.... Read moreIndustry
view channelNew Collaboration Brings Automated Mass Spectrometry to Routine Laboratory Testing
Mass spectrometry is a powerful analytical technique that identifies and quantifies molecules based on their mass and electrical charge. Its high selectivity, sensitivity, and accuracy make it indispensable... Read more
AI-Powered Cervical Cancer Test Set for Major Rollout in Latin America
Noul Co., a Korean company specializing in AI-based blood and cancer diagnostics, announced it will supply its intelligence (AI)-based miLab CER cervical cancer diagnostic solution to Mexico under a multi‑year... Read more
Diasorin and Fisher Scientific Enter into US Distribution Agreement for Molecular POC Platform
Diasorin (Saluggia, Italy) has entered into an exclusive distribution agreement with Fisher Scientific, part of Thermo Fisher Scientific (Waltham, MA, USA), for the LIAISON NES molecular point-of-care... Read more