Abnormal Liver Function Test Associated with Severe SARS-CoV-2 Infection
|
By LabMedica International staff writers Posted on 15 Feb 2021 |

Image: Liver function test abnormalities at hospital admission are associated with severe course of SARS-CoV-2 infection (Photo courtesy of Life Line Screening).
COVID-19 predominantly affects the pulmonary tract causing mainly respiratory symptoms, however, involvement of other organ systems has been described, including myocarditis, acute kidney injury, neurological abnormalities and acute liver injury.
During infection with SARS-CoV-2 liver injury occurs in a relevant proportion of patients. As yet, mainly elevation of aminotransferases has been described, while abnormalities of cholestatic parameters, that is, gamma-glutamyltransferase and alkaline phosphatase were reported less frequently. Liver function test (LFT) peak levels correlate with severity and/or outcome in COVID-19 patients.
Medical Scientists at the University Hospital Munich (Munich, Germany) analyzed liver function tests in a cohort of 217 patients (median age, 63 years) with SARS-CoV-2 infection and without pre-existing liver disease. Laboratory tests including liver enzymes were performed on admission and repeatedly until discharge. Values at admission as well as respective minimal and peak values were obtained via automated data extraction tools. LFT analysis included aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), gamma-glutamyltransferase (GGT), total bilirubin (TBIL) and albumin. Further analyses included C-reactive protein (CRP) and interleukin 6 (IL-6). In case the patient had been transferred from another hospital, laboratory values from the initial admission were extracted from the patients’ files.
The investigators reported that abnormal LFT at hospital admission was present in 125 (58%) patients, with a predominant elevation AST; 42%, GGT; 37% and ALT; 27%, while hypoalbuminemia was observed in 33% of the patients. Of the 217 patients, 36% required treatment in the intensive care unit (ICU) and 32% underwent mechanical ventilation, with a total fatality rate of 14.7%, mostly related to COVID-19. Elevated levels of AST, ALT, GGT as well as hypoalbuminemia were also associated with an increased risk for ICU admission with odds ratio ranging from 2.06 to 13.95. On the other hand, hyperbilirubinemia, although rare at admission, was an independent risk factor for COVID-19-related death (OR, 4.80). The team noted that when hypoalbuminemia was combined with elevation of any LFT abnormality, the risk of ICU admission was markedly increased with the highest risk observed for the combination of hypoalbuminemia and AST (OR, 46.22).
The authors concluded that there was a significant correlation of elevation of baseline LFT, including GGT, as well as hypoalbuminemia with more severe courses of SARS-CoV-2 infections. Thus, baseline hypoalbuminemia when combined with other abnormal LFT in particular with abnormal AST or GGT should be regarded as a red flag indicating a more severe course of the disease and could support clinical decisions regarding closer monitoring and intensive care of patients with COVID-19. With a cut-off of 3.55 mg/dL, which is the lower limit of normal in their laboratory institute, albumin could differentiate between less and more severe cases with a sensitivity and specificity of 80%, respectively. The study was published on January 29, 2021 in the journal GUT.
Related Links:
University Hospital Munich
During infection with SARS-CoV-2 liver injury occurs in a relevant proportion of patients. As yet, mainly elevation of aminotransferases has been described, while abnormalities of cholestatic parameters, that is, gamma-glutamyltransferase and alkaline phosphatase were reported less frequently. Liver function test (LFT) peak levels correlate with severity and/or outcome in COVID-19 patients.
Medical Scientists at the University Hospital Munich (Munich, Germany) analyzed liver function tests in a cohort of 217 patients (median age, 63 years) with SARS-CoV-2 infection and without pre-existing liver disease. Laboratory tests including liver enzymes were performed on admission and repeatedly until discharge. Values at admission as well as respective minimal and peak values were obtained via automated data extraction tools. LFT analysis included aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), gamma-glutamyltransferase (GGT), total bilirubin (TBIL) and albumin. Further analyses included C-reactive protein (CRP) and interleukin 6 (IL-6). In case the patient had been transferred from another hospital, laboratory values from the initial admission were extracted from the patients’ files.
The investigators reported that abnormal LFT at hospital admission was present in 125 (58%) patients, with a predominant elevation AST; 42%, GGT; 37% and ALT; 27%, while hypoalbuminemia was observed in 33% of the patients. Of the 217 patients, 36% required treatment in the intensive care unit (ICU) and 32% underwent mechanical ventilation, with a total fatality rate of 14.7%, mostly related to COVID-19. Elevated levels of AST, ALT, GGT as well as hypoalbuminemia were also associated with an increased risk for ICU admission with odds ratio ranging from 2.06 to 13.95. On the other hand, hyperbilirubinemia, although rare at admission, was an independent risk factor for COVID-19-related death (OR, 4.80). The team noted that when hypoalbuminemia was combined with elevation of any LFT abnormality, the risk of ICU admission was markedly increased with the highest risk observed for the combination of hypoalbuminemia and AST (OR, 46.22).
The authors concluded that there was a significant correlation of elevation of baseline LFT, including GGT, as well as hypoalbuminemia with more severe courses of SARS-CoV-2 infections. Thus, baseline hypoalbuminemia when combined with other abnormal LFT in particular with abnormal AST or GGT should be regarded as a red flag indicating a more severe course of the disease and could support clinical decisions regarding closer monitoring and intensive care of patients with COVID-19. With a cut-off of 3.55 mg/dL, which is the lower limit of normal in their laboratory institute, albumin could differentiate between less and more severe cases with a sensitivity and specificity of 80%, respectively. The study was published on January 29, 2021 in the journal GUT.
Related Links:
University Hospital Munich
Latest Clinical Chem. News
- New PSA-Based Prognostic Model Improves Prostate Cancer Risk Assessment
- Extracellular Vesicles Linked to Heart Failure Risk in CKD Patients
- Study Compares Analytical Performance of Quantitative Hepatitis B Surface Antigen Assays
- Blood Test Could Predict and Identify Early Relapses in Myeloma Patients
- Compact Raman Imaging System Detects Subtle Tumor Signals
- Noninvasive Blood-Glucose Monitoring to Replace Finger Pricks for Diabetics
- POC Breath Diagnostic System to Detect Pneumonia-Causing Pathogens
- Online Tool Detects Drug Exposure Directly from Patient Samples
- Chemical Imaging Probe Could Track and Treat Prostate Cancer
- Mismatch Between Two Common Kidney Function Tests Indicates Serious Health Problems
- VOCs Show Promise for Early Multi-Cancer Detection
- Portable Raman Spectroscopy Offers Cost-Effective Kidney Disease Diagnosis at POC
- Gold Nanoparticles to Improve Accuracy of Ovarian Cancer Diagnosis
- Simultaneous Cell Isolation Technology Improves Cancer Diagnostic Accuracy
- Simple Non-Invasive Hair-Based Test Could Speed ALS Diagnosis
- Paper Strip Saliva Test Detects Elevated Uric Acid Levels Without Blood Draws
Channels
Molecular Diagnostics
view channel
POC Test Uses Fingerstick Blood, Serum, Or Plasma Sample to Detect Typhoid Fever
Typhoid fever is an acute febrile illness caused by Salmonella enterica serovar Typhi (S. Typhi) and affects an estimated 11–21 million people globally each year, resulting in approximately 128,000–161,000... Read more
Rapid Testing Panel Simultaneously Detects 15 Drugs of Abuse in Urine Within 21 Minutes
Illicit drug use and excessive use of prescription medicine is growing across the US amid a severe opioid crisis. Although overdose fatalities were reported to have declined by nearly 27% in 2024, many... Read moreHematology
view channel
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read more
Fast and Easy Test Could Revolutionize Blood Transfusions
Blood transfusions are a cornerstone of modern medicine, yet red blood cells can deteriorate quietly while sitting in cold storage for weeks. Although blood units have a fixed expiration date, cells from... Read more
Automated Hemostasis System Helps Labs of All Sizes Optimize Workflow
High-volume hemostasis sections must sustain rapid turnaround while managing reruns and reflex testing. Manual tube handling and preanalytical checks can strain staff time and increase opportunities for error.... Read more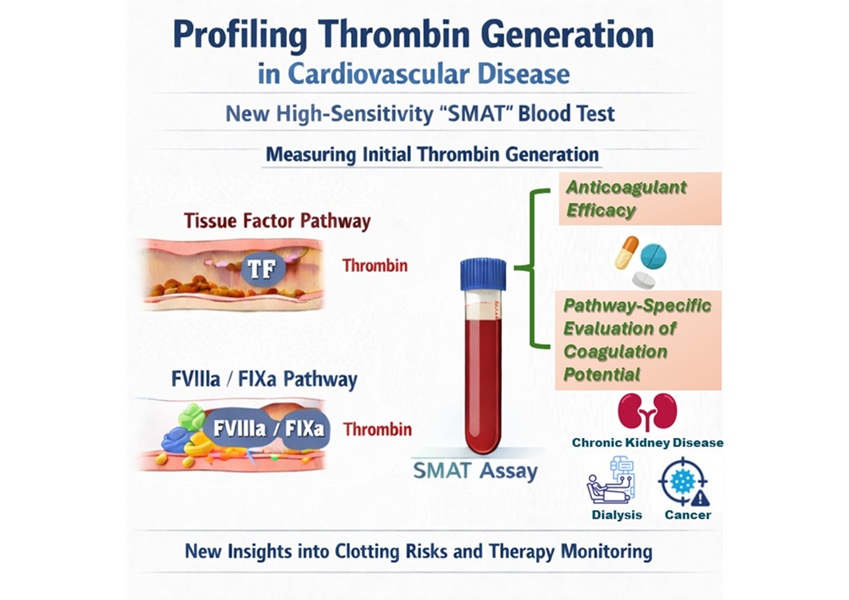
High-Sensitivity Blood Test Improves Assessment of Clotting Risk in Heart Disease Patients
Blood clotting is essential for preventing bleeding, but even small imbalances can lead to serious conditions such as thrombosis or dangerous hemorrhage. In cardiovascular disease, clinicians often struggle... Read moreImmunology
view channelBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read more
Whole-Genome Sequencing Approach Identifies Cancer Patients Benefitting From PARP-Inhibitor Treatment
Targeted cancer therapies such as PARP inhibitors can be highly effective, but only for patients whose tumors carry specific DNA repair defects. Identifying these patients accurately remains challenging,... Read more
Ultrasensitive Liquid Biopsy Demonstrates Efficacy in Predicting Immunotherapy Response
Immunotherapy has transformed cancer treatment, but only a small proportion of patients experience lasting benefit, with response rates often remaining between 10% and 20%. Clinicians currently lack reliable... Read moreMicrobiology
view channel
Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
Alzheimer’s disease affects approximately 6.7 million people in the United States and nearly 50 million worldwide, yet early cognitive decline remains difficult to characterize. Increasing evidence suggests... Read moreAI-Powered Platform Enables Rapid Detection of Drug-Resistant C. Auris Pathogens
Infections caused by the pathogenic yeast Candida auris pose a significant threat to hospitalized patients, particularly those with weakened immune systems or those who have invasive medical devices.... Read morePathology
view channel
Engineered Yeast Cells Enable Rapid Testing of Cancer Immunotherapy
Developing new cancer immunotherapies is a slow, costly, and high-risk process, particularly for CAR T cell treatments that must precisely recognize cancer-specific antigens. Small differences in tumor... Read more
First-Of-Its-Kind Test Identifies Autism Risk at Birth
Autism spectrum disorder is treatable, and extensive research shows that early intervention can significantly improve cognitive, social, and behavioral outcomes. Yet in the United States, the average age... Read moreTechnology
view channel
Robotic Technology Unveiled for Automated Diagnostic Blood Draws
Routine diagnostic blood collection is a high‑volume task that can strain staffing and introduce human‑dependent variability, with downstream implications for sample quality and patient experience.... Read more
ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
Clinical laboratories generate billions of test results each year, creating a treasure trove of data with the potential to support more personalized testing, improve operational efficiency, and enhance patient care.... Read moreAptamer Biosensor Technology to Transform Virus Detection
Rapid and reliable virus detection is essential for controlling outbreaks, from seasonal influenza to global pandemics such as COVID-19. Conventional diagnostic methods, including cell culture, antigen... Read more
AI Models Could Predict Pre-Eclampsia and Anemia Earlier Using Routine Blood Tests
Pre-eclampsia and anemia are major contributors to maternal and child mortality worldwide, together accounting for more than half a million deaths each year and leaving millions with long-term health complications.... Read moreIndustry
view channel
WHX Labs in Dubai spotlights leadership skills shaping next-generation laboratories
WHX Labs in Dubai (formerly Medlab Middle East), held at Dubai World Trade Centre (DWTC) from 10–13 February, brings together international experts to discuss the factors redefining laboratory leadership,... Read moreNew Collaboration Brings Automated Mass Spectrometry to Routine Laboratory Testing
Mass spectrometry is a powerful analytical technique that identifies and quantifies molecules based on their mass and electrical charge. Its high selectivity, sensitivity, and accuracy make it indispensable... Read more
AI-Powered Cervical Cancer Test Set for Major Rollout in Latin America
Noul Co., a Korean company specializing in AI-based blood and cancer diagnostics, announced it will supply its intelligence (AI)-based miLab CER cervical cancer diagnostic solution to Mexico under a multi‑year... Read more