Alzheimer's Disease Subtypes Proposed from Brain Gene Expression Profiles
|
By LabMedica International staff writers Posted on 18 Jan 2021 |
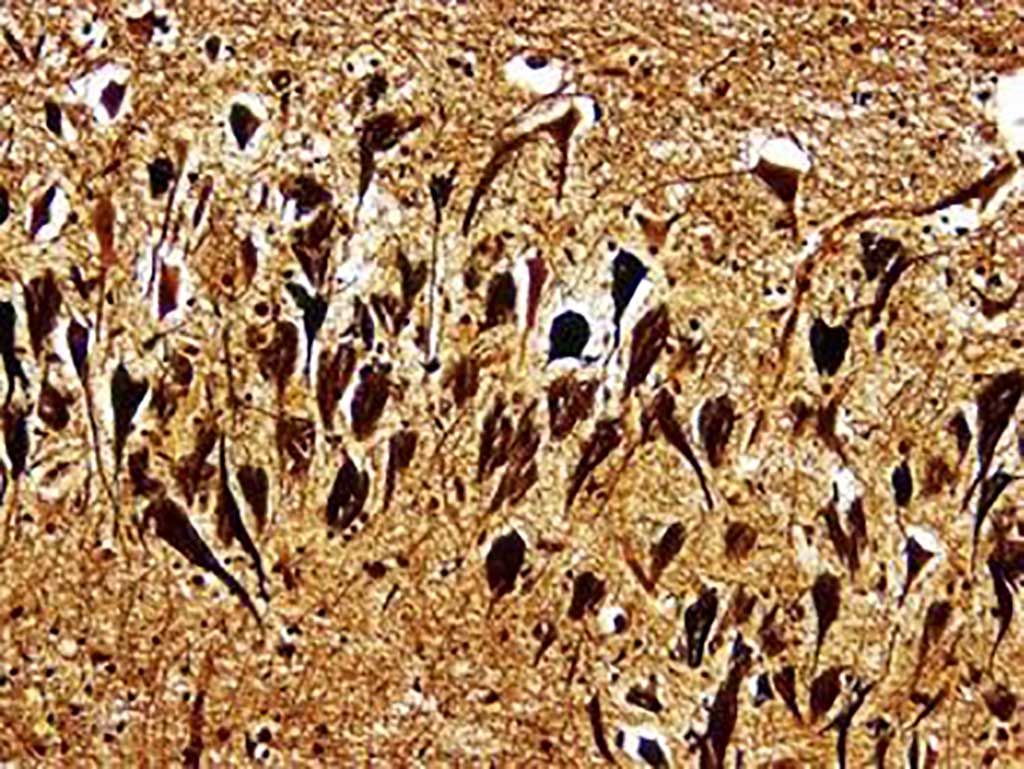
Image: Histopathology of neurofibrillary tangles in the brain of a patient with Alzheimer`s disease (Bielschowski silver stain) (Photo courtesy of Dimitri P. Agamanolis, MD).
Alzheimer’s disease (AD) is the most common form of dementia in the elderly, estimated to affect more than 5.8 million individuals in the USA and more than 50 million worldwide, with almost half of individuals aged over 75 years.
The neuropathological manifestations of AD traditionally include the accumulation of amyloid-beta (Aβ) peptide as extracellular plaques and hyperphosphorylated tau as intracellular neurofibrillary tangles (NFTs), typically identified on postmortem biopsy and used for definitive AD diagnosis.
A large team of scientists led by those at Icahn School of Medicine (New York, NY, USA) used transcriptome sequence data from more than 1,500 postmortem brain samples from individuals with or without AD to highlight several expression-based AD subtypes. They analyzed transcriptome data for more than 900 samples from the frontal pole (FP), superior temporal gyrus (STG), parahippocampal gyrus (PHG), and inferior frontal gyrus (IFG) brain regions in 364 Mount Sinai/JJ Peters VA Medical Center Brain Bank (MSBB-AD) participants with or without AD or related dementia.
The scientists focused in on differential gene expression patterns in the PHG, adjusting for AD stage and severity. Their results pointed to five PHG expression-based subtypes of AD, falling into three main clusters, along with related molecular signatures, clinical features, and potential driver genes. The team identified three major molecular subtypes of AD corresponding to different combinations of multiple dysregulated pathways, such as susceptibility to tau-mediated neurodegeneration, amyloid-β neuroinflammation, synaptic signaling, immune activity, mitochondria organization, and myelination. Multiscale network analysis reveals subtype-specific drivers such as GABRB2, LRP10, MSN, PLP1, and ATP6V1A. The team reported their results were shored up with data for postmortem brain samples from another 615 AD cases or controls in Religious Orders Study–Memory and Aging Project (ROSMAP).
Bin Zhang, PhD, a Professor of Genetics and genomic Science and senior author of the study, said, “Understanding the genetic and molecular differences between molecular subtypes of AD within these data will provide novel insights into disease pathogenesis and offer new avenues for developing effective therapeutics.” The study was published on January 6, 2021 in the journal Science Advances.
Related Links:
Icahn School of Medicine
The neuropathological manifestations of AD traditionally include the accumulation of amyloid-beta (Aβ) peptide as extracellular plaques and hyperphosphorylated tau as intracellular neurofibrillary tangles (NFTs), typically identified on postmortem biopsy and used for definitive AD diagnosis.
A large team of scientists led by those at Icahn School of Medicine (New York, NY, USA) used transcriptome sequence data from more than 1,500 postmortem brain samples from individuals with or without AD to highlight several expression-based AD subtypes. They analyzed transcriptome data for more than 900 samples from the frontal pole (FP), superior temporal gyrus (STG), parahippocampal gyrus (PHG), and inferior frontal gyrus (IFG) brain regions in 364 Mount Sinai/JJ Peters VA Medical Center Brain Bank (MSBB-AD) participants with or without AD or related dementia.
The scientists focused in on differential gene expression patterns in the PHG, adjusting for AD stage and severity. Their results pointed to five PHG expression-based subtypes of AD, falling into three main clusters, along with related molecular signatures, clinical features, and potential driver genes. The team identified three major molecular subtypes of AD corresponding to different combinations of multiple dysregulated pathways, such as susceptibility to tau-mediated neurodegeneration, amyloid-β neuroinflammation, synaptic signaling, immune activity, mitochondria organization, and myelination. Multiscale network analysis reveals subtype-specific drivers such as GABRB2, LRP10, MSN, PLP1, and ATP6V1A. The team reported their results were shored up with data for postmortem brain samples from another 615 AD cases or controls in Religious Orders Study–Memory and Aging Project (ROSMAP).
Bin Zhang, PhD, a Professor of Genetics and genomic Science and senior author of the study, said, “Understanding the genetic and molecular differences between molecular subtypes of AD within these data will provide novel insights into disease pathogenesis and offer new avenues for developing effective therapeutics.” The study was published on January 6, 2021 in the journal Science Advances.
Related Links:
Icahn School of Medicine
Latest Molecular Diagnostics News
- Blood Test Could Spot Common Post-Surgery Condition Early
- New Blood Test Can Help Predict Testicular Cancer Recurrence
- New Test Detects Alzheimer’s by Analyzing Altered Protein Shapes in Blood
- New Diagnostic Markers for Multiple Sclerosis Discovered in Cerebrospinal Fluid
- Cell-Free DNA Predicts Bloodstream Infections in Children with Leukemia
- Study Uses Blood Samples to Identify Diseases Years Before They Start
- MicroRNA-Based Method Predicts CKD and Cardiovascular Risk
- Swab Test Helps Transplant Patients Receive Right Anti-Rejection Medication Dose
- Blood Test Predicts Which Bladder Cancer Patients May Safely Skip Surgery
- Ultra-Sensitive DNA Test Identifies Relapse Risk in Aggressive Leukemia
- Blood Test Could Help Detect Gallbladder Cancer Earlier
- New Blood Test Score Detects Hidden Alcohol-Related Liver Disease
- New Blood Test Predicts Who Will Most Likely Live Longer
- Genetic Test Predicts Radiation Therapy Risk for Prostate Cancer Patients
- Genetic Test Aids Early Detection and Improved Treatment for Cancers
- New Genome Sequencing Technique Measures Epstein-Barr Virus in Blood
Channels
Clinical Chemistry
view channelNew Blood Test Index Offers Earlier Detection of Liver Scarring
Metabolic fatty liver disease is highly prevalent and often silent, yet it can progress to fibrosis, cirrhosis, and liver failure. Current first-line blood test scores frequently return indeterminate results,... Read more
Electronic Nose Smells Early Signs of Ovarian Cancer in Blood
Ovarian cancer is often diagnosed at a late stage because its symptoms are vague and resemble those of more common conditions. Unlike breast cancer, there is currently no reliable screening method, and... Read moreHematology
view channel
Rapid Cartridge-Based Test Aims to Expand Access to Hemoglobin Disorder Diagnosis
Sickle cell disease and beta thalassemia are hemoglobin disorders that often require referral to specialized laboratories for definitive diagnosis, delaying results for patients and clinicians.... Read more
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read moreImmunology
view channel
Cancer Mutation ‘Fingerprints’ to Improve Prediction of Immunotherapy Response
Cancer cells accumulate thousands of genetic mutations, but not all mutations affect tumors in the same way. Some make cancer cells more visible to the immune system, while others allow tumors to evade... Read more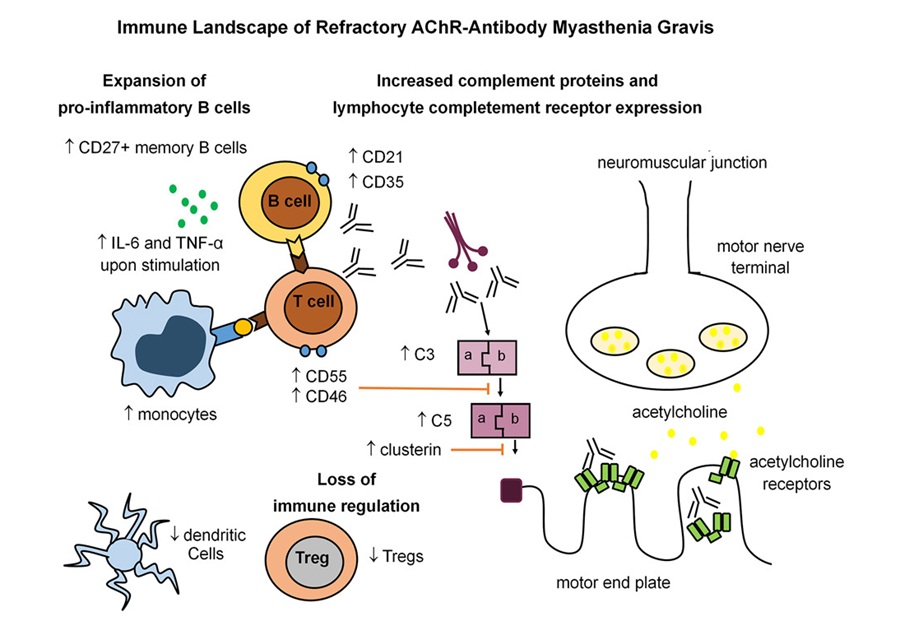
Immune Signature Identified in Treatment-Resistant Myasthenia Gravis
Myasthenia gravis is a rare autoimmune disorder in which immune attack at the neuromuscular junction causes fluctuating weakness that can impair vision, movement, speech, swallowing, and breathing.... Read more
New Biomarker Predicts Chemotherapy Response in Triple-Negative Breast Cancer
Triple-negative breast cancer is an aggressive form of breast cancer in which patients often show widely varying responses to chemotherapy. Predicting who will benefit from treatment remains challenging,... Read moreBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read moreMicrobiology
view channel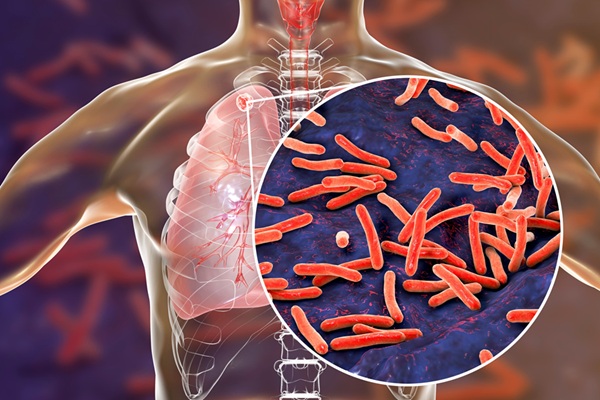
Rapid Sequencing Could Transform Tuberculosis Care
Tuberculosis remains the world’s leading cause of death from a single infectious agent, responsible for more than one million deaths each year. Diagnosing and monitoring the disease can be slow because... Read more
Blood-Based Viral Signature Identified in Crohn’s Disease
Crohn’s disease is a chronic inflammatory intestinal disorder affecting approximately 0.4% of the European population, with symptoms and progression that vary widely. Although viral components of the microbiome... Read morePathology
view channel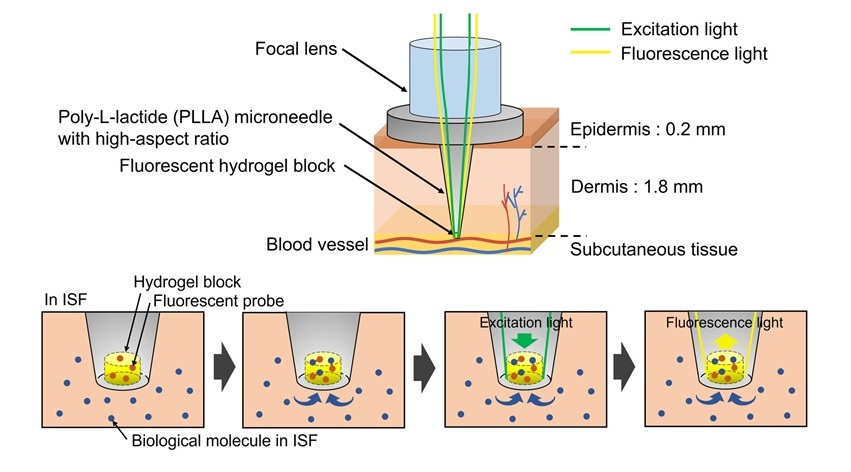
World’s First Optical Microneedle Device to Enable Blood-Sampling-Free Clinical Testing
Blood sampling is one of the most common clinical procedures, but it can be difficult or uncomfortable for many patients, especially older adults or individuals with certain medical conditions.... Read more
Pathogen-Agnostic Testing Reveals Hidden Respiratory Threats in Negative Samples
Polymerase Chain Reaction (PCR) testing became widely recognized during the COVID-19 pandemic as a powerful method for detecting viruses such as SARS-CoV-2. PCR belongs to a group of diagnostic methods... Read moreTechnology
view channel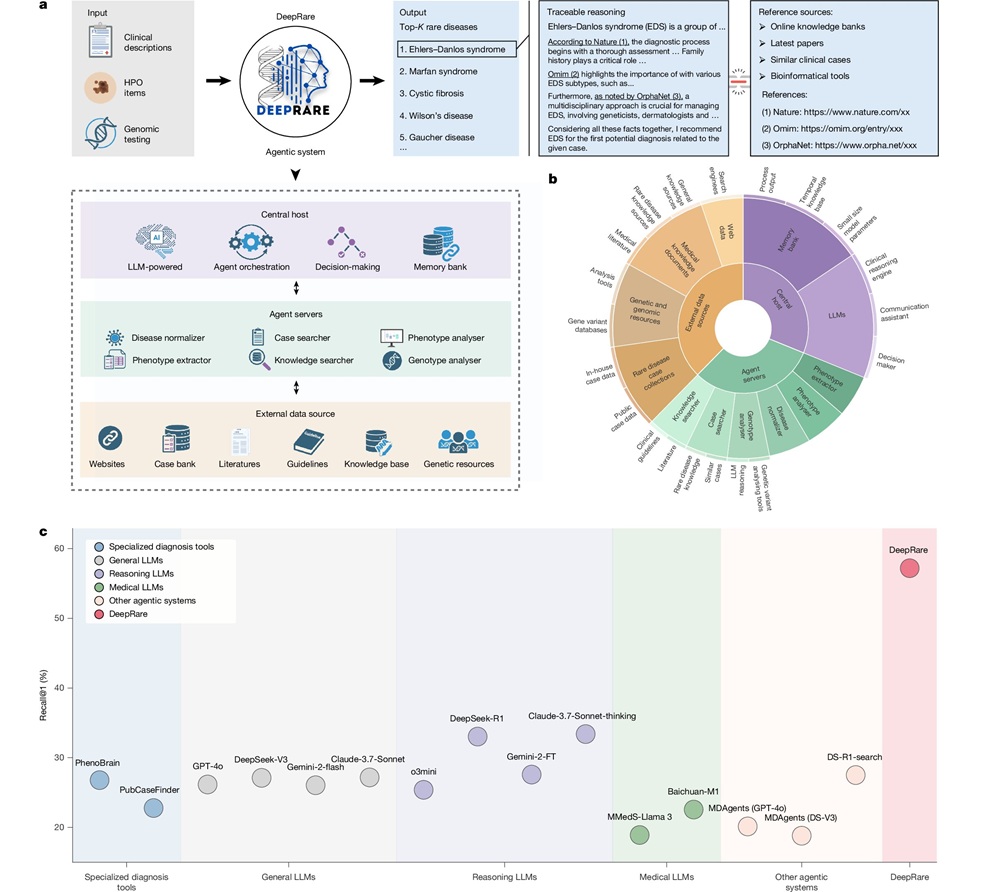
AI Model Outperforms Clinicians in Rare Disease Detection
Rare diseases affect an estimated 300 million people worldwide, yet diagnosis is often protracted and error-prone. Many conditions present with heterogeneous signs that overlap with common disorders, leading... Read more
AI-Driven Diagnostic Demonstrates High Accuracy in Detecting Periprosthetic Joint Infection
Periprosthetic joint infection (PJI) is a rare but serious complication affecting 1% to 2% of primary joint replacement surgeries. The condition occurs when bacteria or fungi infect tissues around an implanted... Read moreIndustry
view channel
Cepheid Joins CDC Initiative to Strengthen U.S. Pandemic Testing Preparednesss
Cepheid (Sunnyvale, CA, USA) has been selected by the U.S. Centers for Disease Control and Prevention (CDC) as one of four national collaborators in a federal initiative to speed rapid diagnostic technologies... Read more
QuidelOrtho Collaborates with Lifotronic to Expand Global Immunoassay Portfolio
QuidelOrtho (San Diego, CA, USA) has entered a long-term strategic supply agreement with Lifotronic Technology (Shenzhen, China) to expand its global immunoassay portfolio and accelerate customer access... Read more




















