Second Protein Identified for Common Kidney Failure
|
By LabMedica International staff writers Posted on 01 Dec 2014 |
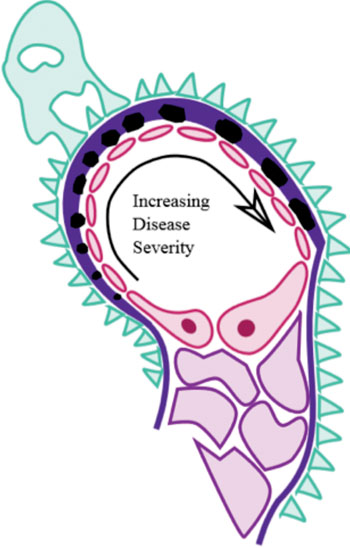
Image: Diagram of pathological changes in a glomerulus (visible via electron microscopy) in membranous nephropathy. Black - immune complex; Dark Purple - basement membrane; Pink – endothelium; Green - visceral epithelium; Light Purple - mesangial cells (Photo by M. Komorniczak and Huckfinne, courtesy of Wikimedia).
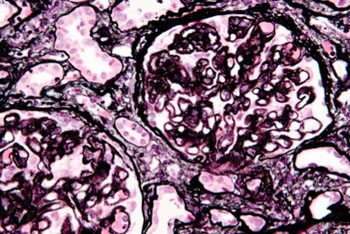
Image: Very high magnification micrograph of membranous nephropathy (also membranous glomerulonephritis). Jones stain of kidney biopsy. The characteristic feature on light microscopy is basement membrane thickening/spike formation (best seen with silver stains). On electron microscopy, subepithelial deposits are also seen (Photo by Nephron, courtesy of Wikimedia).
An international team of researchers has found a second protein, THSD7A, associated with a common form of kidney failure—the autoimmune “membranous nephropathy” (MN). The discovery is likely to provide an important new biomarker for the disease.
MN occurs when kidney small blood vessels that filter wastes from blood are damaged by circulating autoantibodies. Proteins leak from the damaged blood vessels into the urine. For many people, loss of these proteins eventually leads to nephrotic syndrome. Unchecked, MN can lead to kidney failure or end-stage renal disease (ESRD). Approximately 14% of ESRD is associated with glomerulonephritis, of which MN is a common form.
As the second protein associated with MN and autoimmune response, THSD7A can be used to develop a new blood test. The research team previously discovered phospholipase A2 receptor 1 (PLA2R1) as the protein target of autoantibodies in up to 70% of people suffering from MN. However, the target antigen in the remaining 30% of patients remained unknown. Senior author Gérard Lambeau, PhD, said that the discovery is of THSD7A “and the corresponding anti-THSD7A autoantibodies in a group of about 10% of MN patients who did not have anti-PLA2R1 autoantibodies.” This finding thus identifies a distinct subgroup of MN patients with anti-THSD7A as a likely biomarker.
“The discovery of this second antigen-antibody system in MN will allow clinicians to diagnose this new form of primary (autoimmune) MN and provides a new method to monitor the disease activity in this subgroup of patients,” said co-lead authors Nicola Tomas, MD, and Laurence Beck, MD, PhD. Coauthor Jon Klein, MD, PhD, said, “The team has now found another protein that impacts additional patients with MN. Once a blood test is available, we will have additional tools to follow the response to treatment and possibly reduce the number of kidney biopsies necessary for disease detection.”
“Our discovery of PLA2R1 as the target of autoantibodies energized research and accelerated the pace of discovery in this uncommon but serious cause of kidney disease,” said David Salant, MD, “Hopefully, our current findings will spur further research to identify the target antigen to benefit the remaining 20% of patients with MN.”
“This discovery also represents an excellent example of international collaboration, with the decision to combine the independent discoveries of this target antigen by groups on both sides of the Atlantic into a jointly authored manuscript,” emphasized Dr. Beck and Prof. Rolf Stahl. The team consisted of researchers from France, Germany, and the USA.
The study, by Tomas NM, Beck L, et al., was published online ahead of print November 13, 2014, in the New England Journal of Medicine. It was also presented at the American Society of Nephrology (ASN) (Washington DC, USA) Kidney Week 2014 (November 11–16, Philadelphia, PA, USA; Abstract TH-OR071).
Related Links:
American Society of Nephrology (ASN)
MN occurs when kidney small blood vessels that filter wastes from blood are damaged by circulating autoantibodies. Proteins leak from the damaged blood vessels into the urine. For many people, loss of these proteins eventually leads to nephrotic syndrome. Unchecked, MN can lead to kidney failure or end-stage renal disease (ESRD). Approximately 14% of ESRD is associated with glomerulonephritis, of which MN is a common form.
As the second protein associated with MN and autoimmune response, THSD7A can be used to develop a new blood test. The research team previously discovered phospholipase A2 receptor 1 (PLA2R1) as the protein target of autoantibodies in up to 70% of people suffering from MN. However, the target antigen in the remaining 30% of patients remained unknown. Senior author Gérard Lambeau, PhD, said that the discovery is of THSD7A “and the corresponding anti-THSD7A autoantibodies in a group of about 10% of MN patients who did not have anti-PLA2R1 autoantibodies.” This finding thus identifies a distinct subgroup of MN patients with anti-THSD7A as a likely biomarker.
“The discovery of this second antigen-antibody system in MN will allow clinicians to diagnose this new form of primary (autoimmune) MN and provides a new method to monitor the disease activity in this subgroup of patients,” said co-lead authors Nicola Tomas, MD, and Laurence Beck, MD, PhD. Coauthor Jon Klein, MD, PhD, said, “The team has now found another protein that impacts additional patients with MN. Once a blood test is available, we will have additional tools to follow the response to treatment and possibly reduce the number of kidney biopsies necessary for disease detection.”
“Our discovery of PLA2R1 as the target of autoantibodies energized research and accelerated the pace of discovery in this uncommon but serious cause of kidney disease,” said David Salant, MD, “Hopefully, our current findings will spur further research to identify the target antigen to benefit the remaining 20% of patients with MN.”
“This discovery also represents an excellent example of international collaboration, with the decision to combine the independent discoveries of this target antigen by groups on both sides of the Atlantic into a jointly authored manuscript,” emphasized Dr. Beck and Prof. Rolf Stahl. The team consisted of researchers from France, Germany, and the USA.
The study, by Tomas NM, Beck L, et al., was published online ahead of print November 13, 2014, in the New England Journal of Medicine. It was also presented at the American Society of Nephrology (ASN) (Washington DC, USA) Kidney Week 2014 (November 11–16, Philadelphia, PA, USA; Abstract TH-OR071).
Related Links:
American Society of Nephrology (ASN)
Latest Pathology News
- Urine Specimen Collection System Improves Diagnostic Accuracy and Efficiency
- AI-Powered 3D Scanning System Speeds Cancer Screening
- Single Sample Classifier Predicts Cancer-Associated Fibroblast Subtypes in Patient Samples
- New AI-Driven Platform Standardizes Tuberculosis Smear Microscopy Workflow
- AI Tool Uses Blood Biomarkers to Predict Transplant Complications Before Symptoms Appear
- High-Resolution Cancer Virus Imaging Uncovers Potential Therapeutic Targets
- Research Consortium Harnesses AI and Spatial Biology to Advance Cancer Discovery
- AI Tool Helps See How Cells Work Together Inside Diseased Tissue
- AI-Powered Microscope Diagnoses Malaria in Blood Smears Within Minutes
- Engineered Yeast Cells Enable Rapid Testing of Cancer Immunotherapy
- First-Of-Its-Kind Test Identifies Autism Risk at Birth
- AI Algorithms Improve Genetic Mutation Detection in Cancer Diagnostics
- Skin Biopsy Offers New Diagnostic Method for Neurodegenerative Diseases
- Fast Label-Free Method Identifies Aggressive Cancer Cells
- New X-Ray Method Promises Advances in Histology
- Single-Cell Profiling Technique Could Guide Early Cancer Detection
Channels
Clinical Chemistry
view channel
Electronic Nose Smells Early Signs of Ovarian Cancer in Blood
Ovarian cancer is often diagnosed at a late stage because its symptoms are vague and resemble those of more common conditions. Unlike breast cancer, there is currently no reliable screening method, and... Read more
Simple Blood Test Offers New Path to Alzheimer’s Assessment in Primary Care
Timely evaluation of cognitive symptoms in primary care is often limited by restricted access to specialized diagnostics and invasive confirmatory procedures. Clinicians need accessible tools to determine... Read moreMolecular Diagnostics
view channel
New Blood Test Score Detects Hidden Alcohol-Related Liver Disease
Fatty liver disease affects nearly one in three adults worldwide and can be driven by metabolic conditions such as obesity and diabetes or by excessive alcohol use. In routine care, it is often difficult... Read more
New Blood Test Predicts Who Will Most Likely Live Longer
As people age, it becomes increasingly difficult to determine who is likely to maintain stable health and who may face serious decline. Traditional indicators such as age, cholesterol, and physical activity... Read moreHematology
view channel
Rapid Cartridge-Based Test Aims to Expand Access to Hemoglobin Disorder Diagnosis
Sickle cell disease and beta thalassemia are hemoglobin disorders that often require referral to specialized laboratories for definitive diagnosis, delaying results for patients and clinicians.... Read more
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read moreMicrobiology
view channel
Hidden Gut Viruses Linked to Colorectal Cancer Risk
Colorectal cancer (CRC) remains a leading cause of cancer mortality in many Western countries, and existing risk-stratification approaches leave substantial room for improvement. Although age, diet, and... Read more
Three-Test Panel Launched for Detection of Liver Fluke Infections
Parasitic liver fluke infections remain endemic in parts of Asia, where transmission commonly occurs through consumption of raw freshwater fish or aquatic plants. Chronic infection is a well-established... Read morePathology
view channel
Urine Specimen Collection System Improves Diagnostic Accuracy and Efficiency
Urine testing is a critical, non-invasive diagnostic tool used to detect conditions such as pregnancy, urinary tract infections, metabolic disorders, cancer, and kidney disease. However, contaminated or... Read more
AI-Powered 3D Scanning System Speeds Cancer Screening
Cytology remains a cornerstone of cancer detection, requiring specialists to examine bodily fluids and cells under a microscope. This labor-intensive process involves inspecting up to one million cells... Read moreTechnology
view channel
Blood Test “Clocks” Predict Start of Alzheimer’s Symptoms
More than 7 million Americans live with Alzheimer’s disease, and related health and long-term care costs are projected to reach nearly USD 400 billion in 2025. The disease has no cure, and symptoms often... Read more
AI-Powered Biomarker Predicts Liver Cancer Risk
Liver cancer, or hepatocellular carcinoma, causes more than 800,000 deaths worldwide each year and often goes undetected until late stages. Even after treatment, recurrence rates reach 70% to 80%, contributing... Read more
Robotic Technology Unveiled for Automated Diagnostic Blood Draws
Routine diagnostic blood collection is a high‑volume task that can strain staffing and introduce human‑dependent variability, with downstream implications for sample quality and patient experience.... Read more
ADLM Launches First-of-Its-Kind Data Science Program for Laboratory Medicine Professionals
Clinical laboratories generate billions of test results each year, creating a treasure trove of data with the potential to support more personalized testing, improve operational efficiency, and enhance patient care.... Read moreIndustry
view channel
Cepheid Joins CDC Initiative to Strengthen U.S. Pandemic Testing Preparednesss
Cepheid (Sunnyvale, CA, USA) has been selected by the U.S. Centers for Disease Control and Prevention (CDC) as one of four national collaborators in a federal initiative to speed rapid diagnostic technologies... Read more
QuidelOrtho Collaborates with Lifotronic to Expand Global Immunoassay Portfolio
QuidelOrtho (San Diego, CA, USA) has entered a long-term strategic supply agreement with Lifotronic Technology (Shenzhen, China) to expand its global immunoassay portfolio and accelerate customer access... Read more







 Analyzer.jpg)