Discarded Blood Tests May Offer Life-Saving Information
|
By LabMedica International staff writers Posted on 08 Sep 2014 |
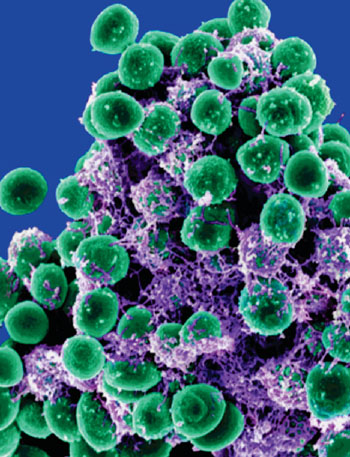
Image: Scanning electron micrograph of Staphylococcus epidermidis, the commonest coagulase-negative staphylococci found on the skin (Photo courtesy of the US National Institute of Allergy and Infectious Diseases).
Blood culture isolates are the cornerstone of adequate antibiotic treatment, but many blood cultures are contaminated with bacteria residing on the skin, and the most common contaminants are coagulase-negative staphylococci (CoNS).
Such contaminated cultures are mostly disregarded and discarded but in fact these contaminated cultures contain diagnostic information such as the antibiotic resistance profiles of CoNS contaminants and those of the actual infecting bacteria isolated subsequently from the same patient.
Clinical scientists at the Sackler Faculty of Medicine (Tel Aviv, Israel) conducted a retrospective study on patients with positive blood cultures from 2009 to 2012. Data included patient demographics, hospitalization records, comorbidities, blood culture results and date of death. The cohort consisted of 2,518 patients with 5,290 blood cultures, where 1,124 patients had 1,664 blood cultures with CoNS contaminants.
High overall CoNS resistance predicted high overall resistance of the subsequent bacterial isolates for Gram-positive and Gram-negative bacteria. The resistance of CoNS contaminants to a specific antibiotic predicted the resistance of the subsequent bacterial isolates to that antibiotic and highly resistant CoNS isolates were associated with higher short-term mortality.
The team noted that most hospital patients are treated at the outset with broad spectrum antibiotics. Days later, after initial test results are known, clinicians replace broad spectrum antibiotics with more precise narrow-spectrum antibiotics, which treat the specific bacteria identified by the blood sample. Narrow spectrum antibiotics are better for the body because they target specific bacteria as opposed to an entire microenvironment. Moreover, broad spectrum antibiotics might result in altered bacterial environments of the skin and gastro-intestinal tract, promoting inflammation and the emergence of resistant pathogens.
Gideon Y Stein, MD, PhD, a lead author of the study said, “Because we have found a direct correlation between resistance profiles of CoNS contaminants and those of the actual infecting bacteria isolated from the same patient, the results of these “junk” samples can be used to predict patient mortality and correct empirical antibiotic therapy. This should serve as an additional, noninvasive, diagnostic tool.” The study was published in the September issue of the Journal of Antimicrobial Chemotherapy.
Related Links:
Tel Aviv University Sackler Faculty of Medicine
Such contaminated cultures are mostly disregarded and discarded but in fact these contaminated cultures contain diagnostic information such as the antibiotic resistance profiles of CoNS contaminants and those of the actual infecting bacteria isolated subsequently from the same patient.
Clinical scientists at the Sackler Faculty of Medicine (Tel Aviv, Israel) conducted a retrospective study on patients with positive blood cultures from 2009 to 2012. Data included patient demographics, hospitalization records, comorbidities, blood culture results and date of death. The cohort consisted of 2,518 patients with 5,290 blood cultures, where 1,124 patients had 1,664 blood cultures with CoNS contaminants.
High overall CoNS resistance predicted high overall resistance of the subsequent bacterial isolates for Gram-positive and Gram-negative bacteria. The resistance of CoNS contaminants to a specific antibiotic predicted the resistance of the subsequent bacterial isolates to that antibiotic and highly resistant CoNS isolates were associated with higher short-term mortality.
The team noted that most hospital patients are treated at the outset with broad spectrum antibiotics. Days later, after initial test results are known, clinicians replace broad spectrum antibiotics with more precise narrow-spectrum antibiotics, which treat the specific bacteria identified by the blood sample. Narrow spectrum antibiotics are better for the body because they target specific bacteria as opposed to an entire microenvironment. Moreover, broad spectrum antibiotics might result in altered bacterial environments of the skin and gastro-intestinal tract, promoting inflammation and the emergence of resistant pathogens.
Gideon Y Stein, MD, PhD, a lead author of the study said, “Because we have found a direct correlation between resistance profiles of CoNS contaminants and those of the actual infecting bacteria isolated from the same patient, the results of these “junk” samples can be used to predict patient mortality and correct empirical antibiotic therapy. This should serve as an additional, noninvasive, diagnostic tool.” The study was published in the September issue of the Journal of Antimicrobial Chemotherapy.
Related Links:
Tel Aviv University Sackler Faculty of Medicine
Latest Microbiology News
- Rapid Sequencing Could Transform Tuberculosis Care
- Blood-Based Viral Signature Identified in Crohn’s Disease
- Hidden Gut Viruses Linked to Colorectal Cancer Risk
- Three-Test Panel Launched for Detection of Liver Fluke Infections
- Rapid Test Promises Faster Answers for Drug-Resistant Infections
- CRISPR-Based Technology Neutralizes Antibiotic-Resistant Bacteria
- Comprehensive Review Identifies Gut Microbiome Signatures Associated With Alzheimer’s Disease
- AI-Powered Platform Enables Rapid Detection of Drug-Resistant C. Auris Pathogens
- New Test Measures How Effectively Antibiotics Kill Bacteria
- New Antimicrobial Stewardship Standards for TB Care to Optimize Diagnostics
- New UTI Diagnosis Method Delivers Antibiotic Resistance Results 24 Hours Earlier
- Breakthroughs in Microbial Analysis to Enhance Disease Prediction
- Blood-Based Diagnostic Method Could Identify Pediatric LRTIs
- Rapid Diagnostic Test Matches Gold Standard for Sepsis Detection
- Rapid POC Tuberculosis Test Provides Results Within 15 Minutes
- Rapid Assay Identifies Bloodstream Infection Pathogens Directly from Patient Samples
Channels
Clinical Chemistry
view channelNew Blood Test Index Offers Earlier Detection of Liver Scarring
Metabolic fatty liver disease is highly prevalent and often silent, yet it can progress to fibrosis, cirrhosis, and liver failure. Current first-line blood test scores frequently return indeterminate results,... Read more
Electronic Nose Smells Early Signs of Ovarian Cancer in Blood
Ovarian cancer is often diagnosed at a late stage because its symptoms are vague and resemble those of more common conditions. Unlike breast cancer, there is currently no reliable screening method, and... Read moreMolecular Diagnostics
view channel
Blood Test Could Spot Common Post-Surgery Condition Early
Heterotopic ossification (HO), the abnormal formation of bone in soft tissue, is a common complication following hip replacement surgery. The condition affects nearly one in three patients and can lead... Read more
New Blood Test Can Help Predict Testicular Cancer Recurrence
Stage 1 testicular germ cell tumor is typically treated with surgery followed by active surveillance. Although most patients experience strong long-term outcomes, about one in four will see their cancer... Read more
New Test Detects Alzheimer’s by Analyzing Altered Protein Shapes in Blood
Alzheimer’s disease begins developing years before memory loss or other symptoms become visible. Misfolded proteins gradually accumulate in the brain, disrupting normal cellular processes.... Read more
New Diagnostic Markers for Multiple Sclerosis Discovered in Cerebrospinal Fluid
Multiple sclerosis (MS) affects nearly three million people worldwide and can cause symptoms such as numbness, visual disturbances, fatigue, and neurological disability. Diagnosing the disease can be challenging... Read moreHematology
view channel
Rapid Cartridge-Based Test Aims to Expand Access to Hemoglobin Disorder Diagnosis
Sickle cell disease and beta thalassemia are hemoglobin disorders that often require referral to specialized laboratories for definitive diagnosis, delaying results for patients and clinicians.... Read more
New Guidelines Aim to Improve AL Amyloidosis Diagnosis
Light chain (AL) amyloidosis is a rare, life-threatening bone marrow disorder in which abnormal amyloid proteins accumulate in organs. Approximately 3,260 people in the United States are diagnosed... Read moreImmunology
view channel
Cancer Mutation ‘Fingerprints’ to Improve Prediction of Immunotherapy Response
Cancer cells accumulate thousands of genetic mutations, but not all mutations affect tumors in the same way. Some make cancer cells more visible to the immune system, while others allow tumors to evade... Read more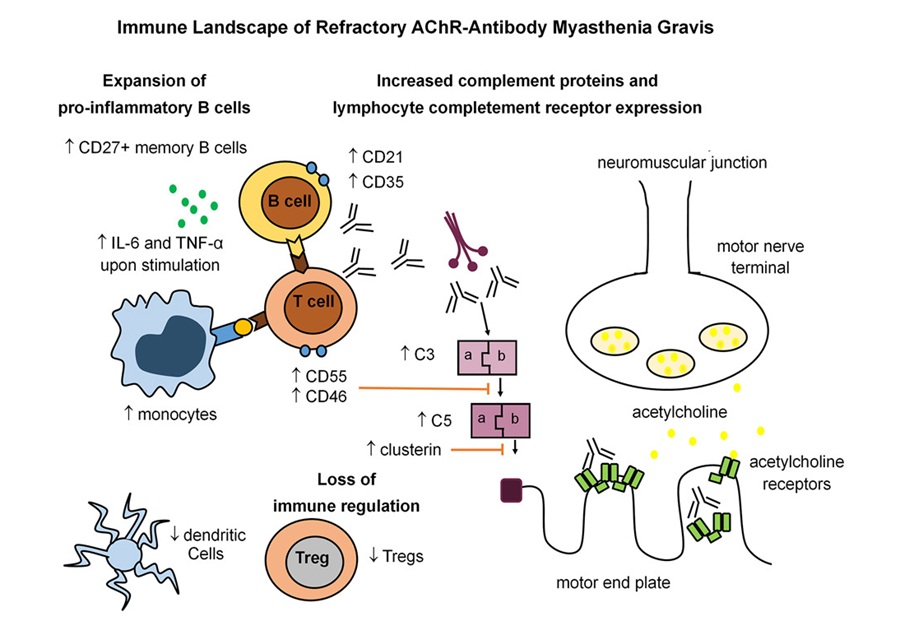
Immune Signature Identified in Treatment-Resistant Myasthenia Gravis
Myasthenia gravis is a rare autoimmune disorder in which immune attack at the neuromuscular junction causes fluctuating weakness that can impair vision, movement, speech, swallowing, and breathing.... Read more
New Biomarker Predicts Chemotherapy Response in Triple-Negative Breast Cancer
Triple-negative breast cancer is an aggressive form of breast cancer in which patients often show widely varying responses to chemotherapy. Predicting who will benefit from treatment remains challenging,... Read moreBlood Test Identifies Lung Cancer Patients Who Can Benefit from Immunotherapy Drug
Small cell lung cancer (SCLC) is an aggressive disease with limited treatment options, and even newly approved immunotherapies do not benefit all patients. While immunotherapy can extend survival for some,... Read morePathology
view channel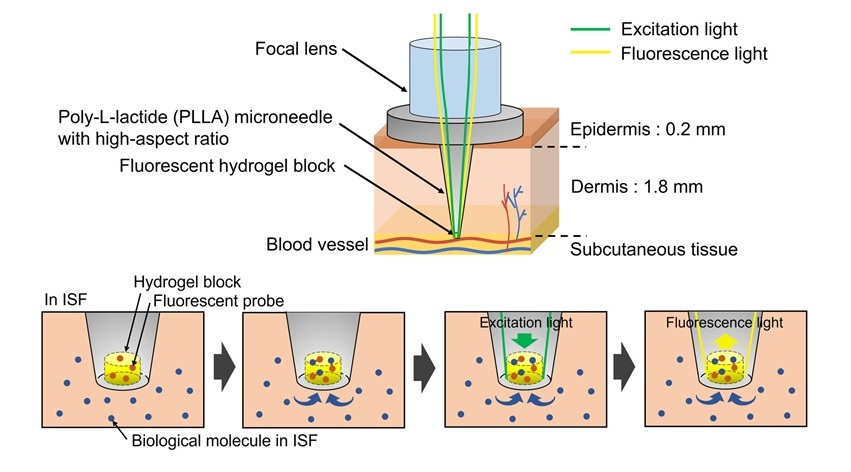
World’s First Optical Microneedle Device to Enable Blood-Sampling-Free Clinical Testing
Blood sampling is one of the most common clinical procedures, but it can be difficult or uncomfortable for many patients, especially older adults or individuals with certain medical conditions.... Read more
Pathogen-Agnostic Testing Reveals Hidden Respiratory Threats in Negative Samples
Polymerase Chain Reaction (PCR) testing became widely recognized during the COVID-19 pandemic as a powerful method for detecting viruses such as SARS-CoV-2. PCR belongs to a group of diagnostic methods... Read moreTechnology
view channel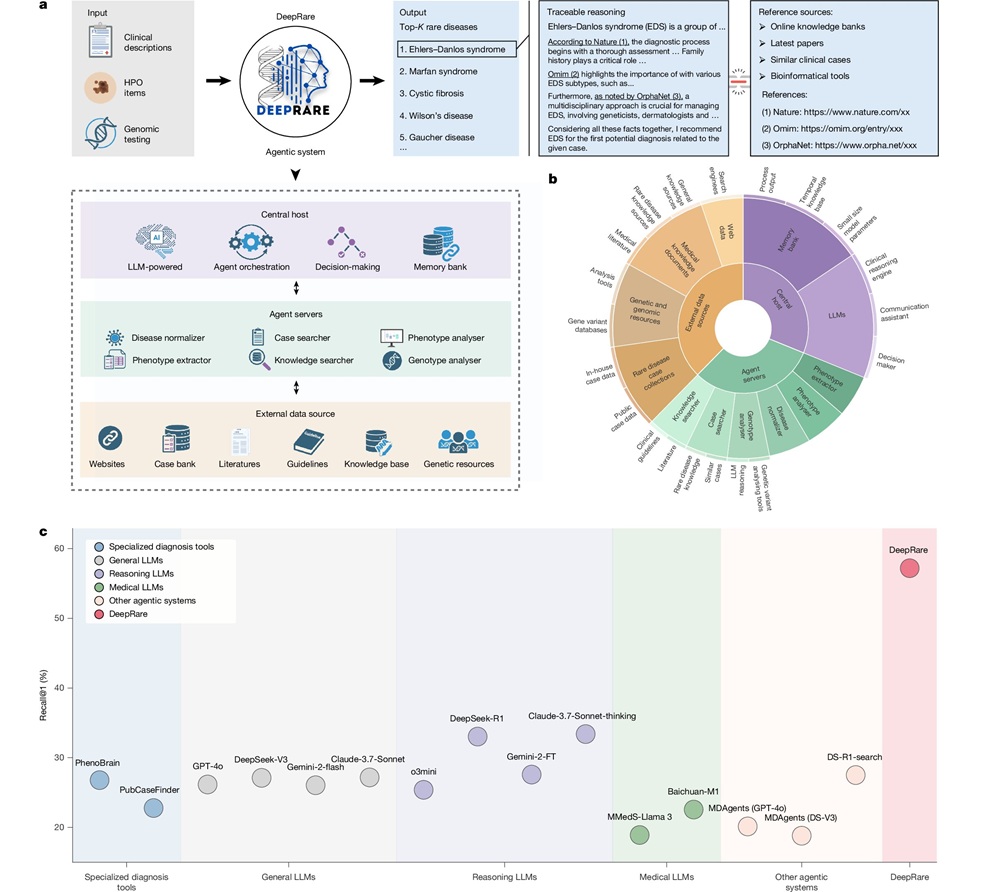
AI Model Outperforms Clinicians in Rare Disease Detection
Rare diseases affect an estimated 300 million people worldwide, yet diagnosis is often protracted and error-prone. Many conditions present with heterogeneous signs that overlap with common disorders, leading... Read more
AI-Driven Diagnostic Demonstrates High Accuracy in Detecting Periprosthetic Joint Infection
Periprosthetic joint infection (PJI) is a rare but serious complication affecting 1% to 2% of primary joint replacement surgeries. The condition occurs when bacteria or fungi infect tissues around an implanted... Read moreIndustry
view channel
Cepheid Joins CDC Initiative to Strengthen U.S. Pandemic Testing Preparednesss
Cepheid (Sunnyvale, CA, USA) has been selected by the U.S. Centers for Disease Control and Prevention (CDC) as one of four national collaborators in a federal initiative to speed rapid diagnostic technologies... Read more
QuidelOrtho Collaborates with Lifotronic to Expand Global Immunoassay Portfolio
QuidelOrtho (San Diego, CA, USA) has entered a long-term strategic supply agreement with Lifotronic Technology (Shenzhen, China) to expand its global immunoassay portfolio and accelerate customer access... Read more


















