New Gene Variant Linked to Prostate Cancer
By LabMedica International staff writers
Posted on 30 Jan 2018
Prostate cancer (PCa) is the most commonly diagnosed malignancy and the second leading cause of cancer-related death in men in the USA. The growth and survival of PCa cells are driven by androgens through activation of the androgen receptor (AR) and its target genes.Posted on 30 Jan 2018
Androgen deprivation therapy (ADT), with medical or surgical castration, is the standard direct treatment for advanced PCa, but patients eventually relapse with progression to castration-resistant PCa (CRPC) and ultimately die of their disease.
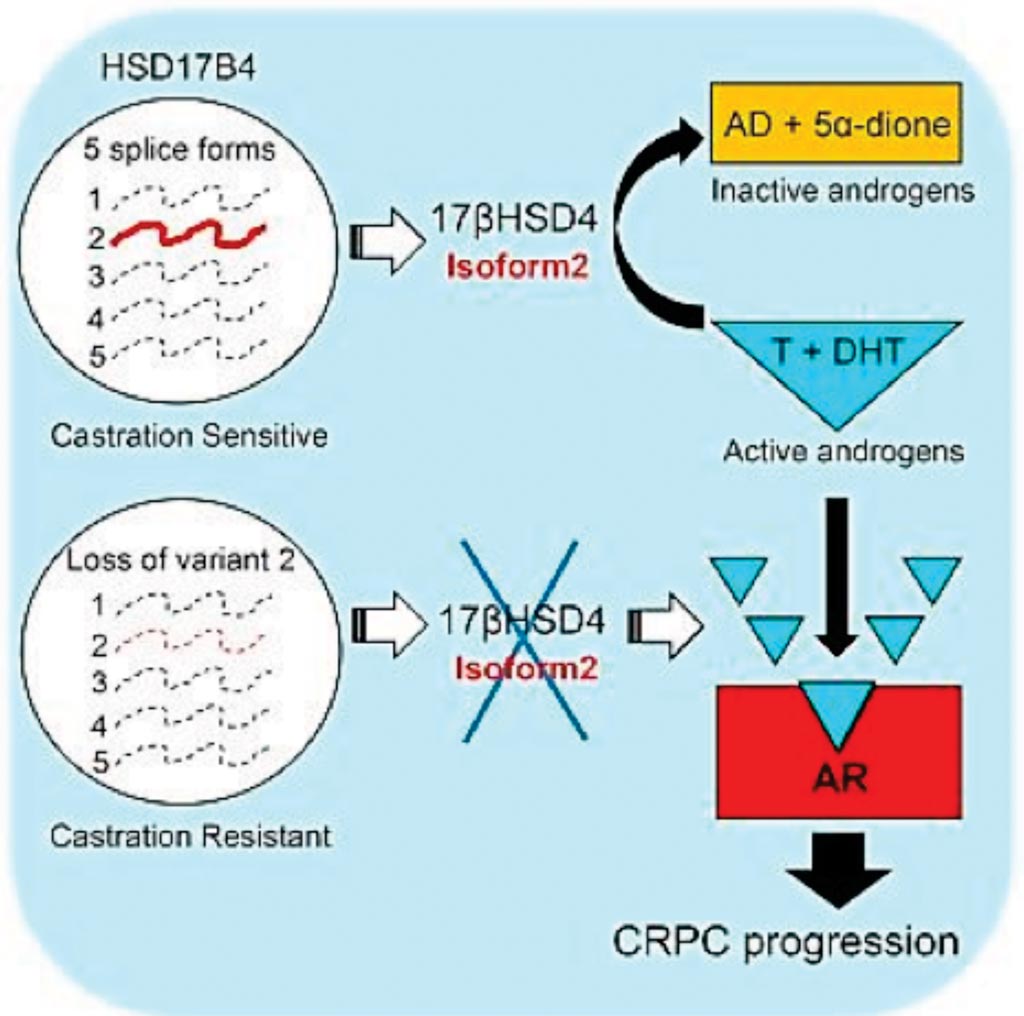
Image: A diagram of the loss of an androgen-inactivating and isoform-specific HSD17B4 splice form enables emergence of castration-resistant prostate cancer (Photo courtesy of the Lerner Research Institute).
Scientists at the Lerner Research Institute (Cleveland, OH, USA) have previously discovered that a gene called Hydroxy-Delta-5-Steroid Dehydrogenase, 3 Beta- And Steroid Delta-Isomerase 1(HSD3B1), when altered, enables prostate tumors to evade treatment and proliferate. They went on to show that the presence of this gene variant does in fact change treatment outcomes and overall survival in men. In a current study the team studied a related gene, called Hydroxysteroid 17-Beta Dehydrogenase 2, (HSD17B).
To determine HSD17B4's role in the transition to CRPC, the team analyzed its expression in tissue from patients with healthy prostates, localized prostate cancer and CRPC. Through a series of analyses including RNA Isolation and real-time polymerase chain reaction (qRT-PCR), the team used an ABI-7500 Real-Time PCR system, Western Blotting and Immunoprecipitation, Isoform Identification by LC-MS/MS Analysis using the Finnigan LTQ-Orbitrap Elite hybrid mass spectrometer system and other techniques were employed.
The scientists found that HSD17B4 expression levels were relatively the same in benign and local prostate cancer tissue, but significantly reduced in CRPC tissue, suggesting that HSD17B4 does play a role in preventing progression to CRPC. They found that only one specific isoform of HSD17B4, isoform 2, enzymatically inactivated androgens and prevented tumor growth. It is expressed during the early phases of prostate cancer, but is lost, or suppressed, in CRPC (advanced prostate cancer). Isoforms vary in amino acid sequence and physiological function, but not DNA code. The team also validated their findings in a preclinical model. Their findings suggest that lack of isoform 2 leads to advanced CRPC.
The authors concluded that their data bring clarity to what has generally been a perplexing link between HSD17B4 and the development of CRPC. When viewed through the lens of the enzymatic properties of a single specific isoform encoded by HSD17B4 variant 2, which is responsible for androgen inactivation, the functional expression of this variant transcript, its loss in the clinical development of CRPC, and its effects on in vivo CRPC growth, all concordantly point toward a causal role in the development of the lethal form of PCa. The study was published on January 16, 2018, in the journal Cell Reports.
Related Links:
Lerner Research Institute