Mutation Reducing Fatty Acid-Binding Protein Activity Lowers Heart Attack Risk
By LabMedica International staff writers
Posted on 09 Sep 2014
A team of Finnish cardiovascular disease researchers found that a mutation generating a low-expression variant of fatty acid-binding protein 4 (FABP4), reduced the risk of heart attack and stroke. Posted on 09 Sep 2014
The FABP4 gene encodes the fatty acid binding protein found in adipocytes. Fatty acid binding proteins are a family of small, highly conserved, cytoplasmic proteins that bind long-chain fatty acids and other hydrophobic ligands. It is thought that the roles of FABPs include fatty acid uptake, transport, and metabolism. Earlier studies detected a mutation (rs77878271) in the human FABP4 gene that caused reduced FABP4 protein transcription.
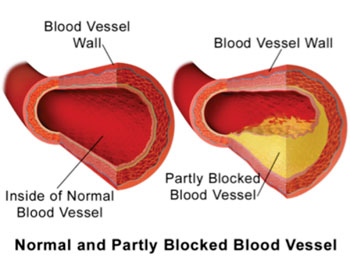
Image: Illustration comparing a normal blood vessel and partially blocked vessel due to atherosclerotic plaque build-up (Photo courtesy of Wikimedia Commons).
Investigators at the University of Helsinki (Finland) examined the effects of this low-expression variant of FABP4 on cardiovascular morbidity and carotid atherosclerosis in a random group of 7,491 individuals and in patient cohorts. The cohorts consisted of patients with advanced carotid atherosclerosis who had undergone surgical procedures (endarterectomy) to excise the inner lining of arteries clogged with atherosclerotic buildup (n = 92) and those having experienced myocardial infarction (MI, n = 3,432).
Results published in the August 13, 2014, online edition of the journal Circulation: Cardiovascular Genetics revealed that the low-expression variant was associated with decreased total cholesterol levels with the largest reduction being in individuals carrying two alleles for the variant. Obese variant allele carriers also showed reduced carotid intima-media thickness and lower prevalence of carotid plaques. Consistently, the variant allele homozygotes showed eight-fold lower odds for MI.
The variant allele was associated with a 3.8-fold reduction in FABP4 transcription and 2.7-fold reduction in apoptosis in the macrophages associated with carotid plaques. High FABP4 expression in carotid plaques was associated with lipid accumulation, intraplaque hemorrhages, plaque ulcerations and phosphoactivated ER (endoplasmic reticulum) stress markers.
"It could be that reduced cell stress in the stenosis, attenuated inflammation, as well as reduced accumulation of cholesterol and other lipids in the arteries help keep atherosclerosis asymptomatic among the gene carriers," said first author Dr. Jani Saksi, a researcher in molecular neurology at the University of Helsinki. "These findings suggest that FABP4 could be a new potential target for drug development aiming to prevent lethal and disabling myocardial and cerebral infarctions induced by atherosclerosis. The inhibition of FABP4 activity – especially among obese people in the risk group for atherosclerosis – may prove to be an important method for reducing these individuals' risk for cardiovascular diseases."
Related Links:
University of Helsinki