Bacteria-Mimicking Vaccine Kills Breast Cancer Cells
By Biotechdaily staff writers
Posted on 14 Feb 2007
With the aid of immune system-stimulating molecules that mimic bacterial components, researchers have used a type of cancer vaccine to both delay and prevent breast tumors in mice. The strategy has potential for the future use of peptide vaccines in women who are at high risk for developing breast cancer.Posted on 14 Feb 2007
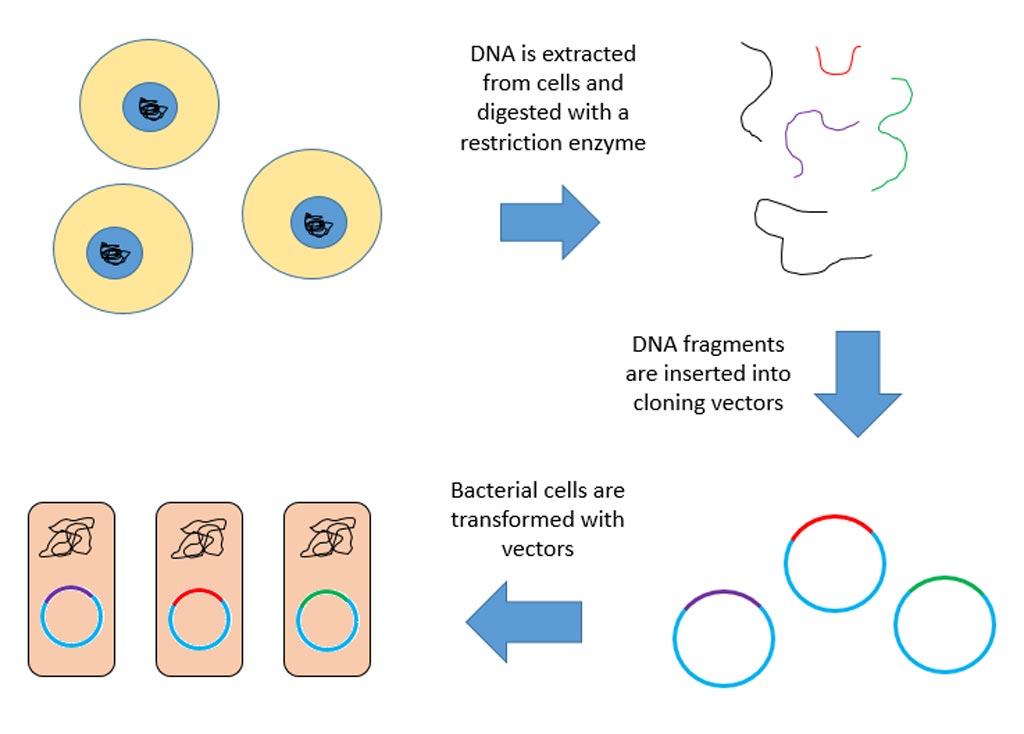
Researchers from the Mayo Clinic (Rochester, MN, USA), University of South Florida, and University of Torino (Italy) utilized compounds called toll-like receptor agonists to help a synthetic peptide vaccine increase the immune system response against breast cancer tumors. At the same time, they used antibodies to suppress other characteristics of the immune system that might interfere with a strong killer T cell response, improving the effectiveness of the vaccine.
In the February 1, 2007, issue of the journal Cancer Research, the researchers reported that their application was successful in preventing spontaneous tumors in transgenic mouse models for breast cancer, even when the vaccine was administered when the mice already had early stage cancer.
"The challenge is to get a foreign peptide recognized by the immune system as a threat so it can react and produce anti-tumor immune cells,” remarked Esteban Celis, M.D., Ph.D., professor in the department of interdisciplinary oncology at the H. Lee Moffitt Cancer Center and Research Institute at the University of South Florida (Tampa, FL, USA). "We've shown that stimulating the immune system using toll-like receptor agonists is very important to alerting it and producing lymphocytes that will have an anti-tumor effect.”
According to Dr. Celis, the immune system typically does not react as strongly to a synthetic peptide in a vaccine as it does against an infectious agent, which is why immune system enhances such as toll-like receptor agonists, which mimic bacterial DNA, help. They also used anti-CD25 antibodies to tie up immune system T regulatory cells, which often serve as suppressors that can reduce responses to the vaccine.
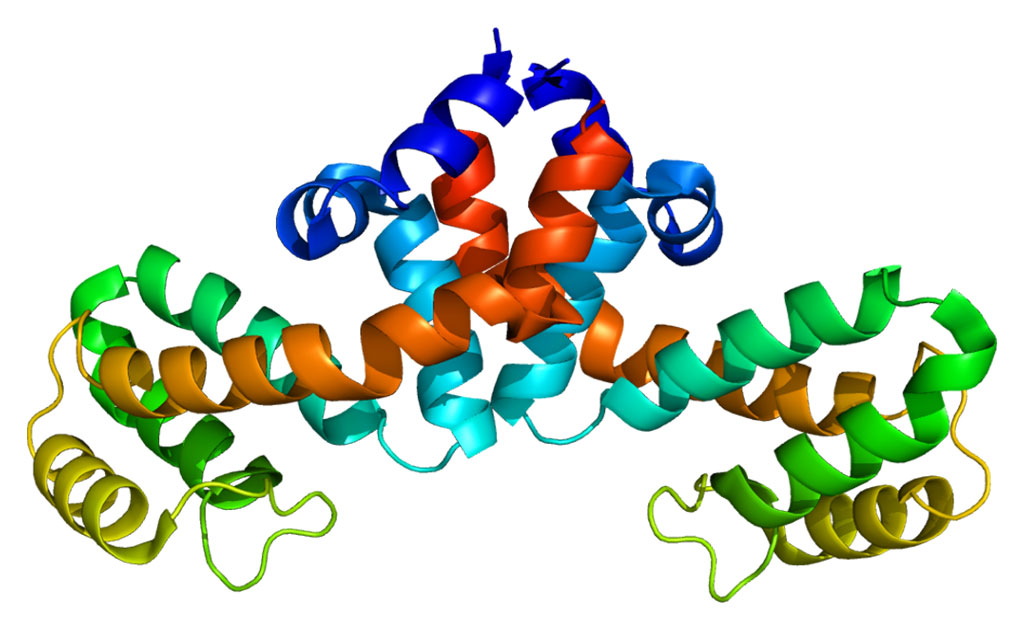
The researchers studied both normal mice and transgenic mice carrying an activated HER2/neu oncogene, which has been associated with breast cancer in humans. To elicit a protective immune response, the transgenic mice were repeatedly given vaccine in combination with the toll-like receptor agonist or were given antibodies that blocked their protective T regulatory cells. Dr. Celis and his colleagues discovered that the peptide vaccine administered this way could prevent or slow the growth of injected tumor cells, and demonstrated some benefit against early stage spontaneous breast tumors.
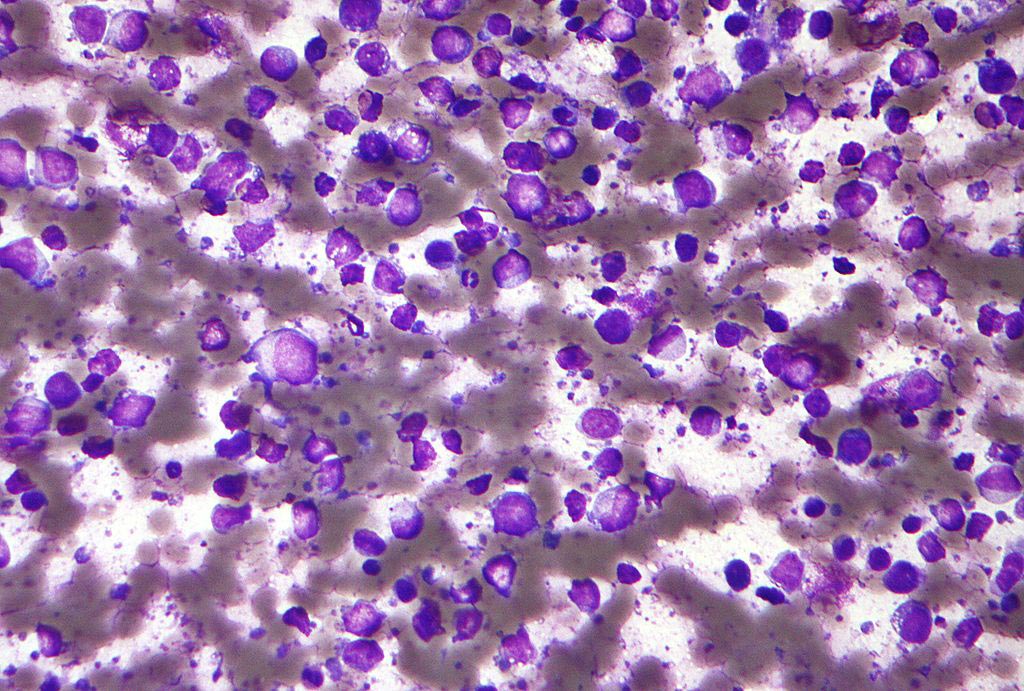
The vaccine was most effective in preventing spontaneous tumors when it was given once at week eight, along with anti-CD25 antibodies, when most mice have excessive and frequently precancerous breast tissue growth called hyperplasia. It completely prevented spontaneous tumors in HER2/neu mice up to 35 weeks of age. Even without the antibody, tumors took much longer to develop, and when they did, they grew more slowly.
"This kind of therapy could be applied to women who have a high likelihood of developing cancer--women with pre-malignant hyperplasia or who have a genetic predisposition or make-up that makes them at high risk,” Dr. Celis commented.
Although the peptide vaccine was successful in preventing spontaneous tumors in the HER2/neu mice, Dr. Celis cautioned that the mice had to be vaccinated prior to the appearance of measurable tumors and that the animals had to receive repeated immunizations. "Once tumors appear, only certain mice respond and there is only a delay in tumor growth,” he said. "It extends survival but does not cure the mice. We know that the immune response in these mice is much lower than in the animals that are younger, and it's likely that the tumor is making something that is inhibiting the immune response.”
Related Links:
University of South Florida










 (3) (1).png)