MRD in AML Detected by Deep Sequencing CD34+ Cells
|
By LabMedica International staff writers Posted on 09 Jun 2022 |

Monitoring of measurable residual disease (MRD) in patients with acute myeloid leukemia (AML) is predictive of disease recurrence and may identify patients who benefit from treatment intensification.
For patients with hematological malignancies such as AML or high-risk myelodysplastic syndrome (MDS), allogeneic hematopoietic stem cell transplantation (allo-HSCT) often remains the only curative treatment option. Nevertheless, relapse after allo-HSCT occurs in 30% to 70% of patients with AML and is the major cause of treatment failure, with dismal prognosis and a 2-year survival of less than 20%.
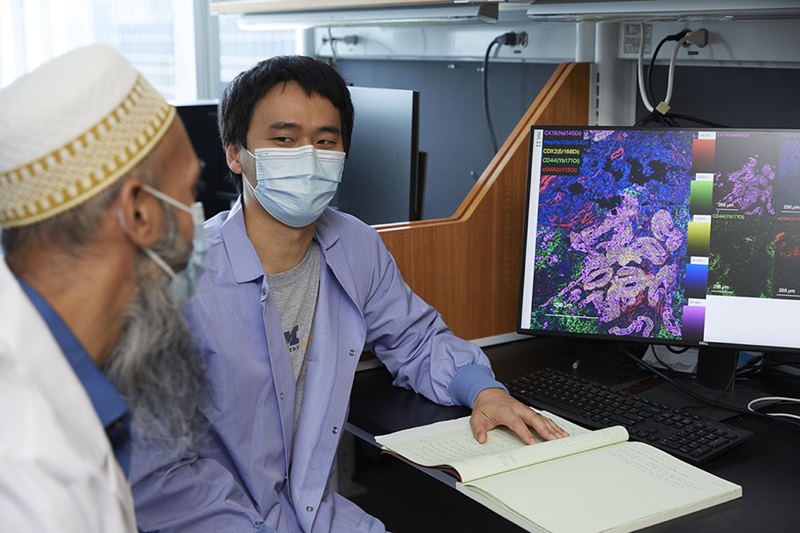
Medical Scientists at the University Hospital Carl Gustav Carus (Dresden, Germany) evaluated the feasibility of a novel approach for MRD detection in peripheral blood (PB), which combines immunomagnetic pre-enrichment and fluorescence-activated cell sorting (FACS) for isolation of CD34+ cells with error-reduced targeted next-generation sequencing (NGS). For clinical validation, they retrospectively analyzed 429 PB and 55 bone marrow (BM) samples of 40 patients with AML or high-risk MDS, with/without molecular relapse based on CD34+ donor chimerism (DC), in complete remission after allogeneic stem cell transplantation.
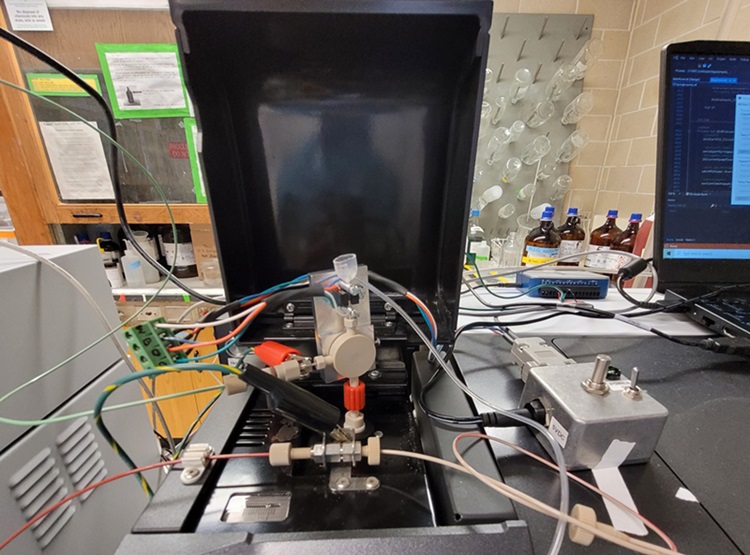
The scientists ensured consistent enrichment of CD34+/CD117+ cell populations to high purity (i.e. >90%). CD34+/CD117+ cells were enriched by using a combination of magnetic cell separation (MACS) and FACS for all samples. Mononuclear cells (MNCs) were extracted by density gradient centrifugation and CD34+/CD117+ cells were isolated from MNCs using MACS by positive selection with the CD34+ or CD117+ Microbead Kit (Miltenyi Biotec, Bergisch-Gladbach, Germany). Sorting of the CD34+/CD117+ cells was then conducted on a BD FACS Aria II cell sorter (BD Biosciences, San Jose, CA, USA), aiming for 5,000 to 10,000 CD34+/CD117+ cells and a purity of >90%. Sequencing of genomic DNA from sorted CD34+/CD117+ cells and unsorted material was performed according to an optimized protocol for error-reduced NGS-based detection of low-level, single-nucleotide variants.
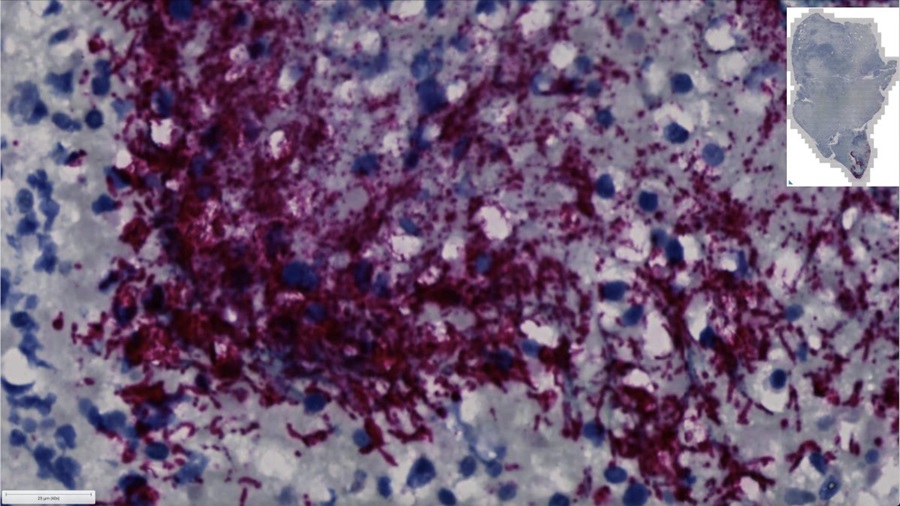
The investigators reported that enrichment of CD34+ cells for NGS increased the detection of mutant alleles in PB ∼1,000-fold (median variant allele frequency, 1.27% versus 0.0046% in unsorted PB). Although a strong correlation was observed for the parallel analysis of CD34+ PB cells with NGS and DC the combination of FACS and NGS improved sensitivity for MRD detection in dilution experiments ∼10-fold to levels of 10−6. In both assays, MRD detection was superior using PB versus BM for CD34+ enrichment. Importantly, next-generation sequencing (NGS) on CD34+ PB cells enabled prediction of molecular relapse with high sensitivity (100%) and specificity (91%), and significantly earlier (median, 48 days; range, 0-281) than by CD34+ DC or NGS of unsorted PB, providing additional time for therapeutic intervention. Moreover, panel sequencing in CD34+ cells allowed for the early assessment of clonal trajectories in hematological complete remission.
The authors proposed a novel, easily accessible, robust method for ultrasensitive MRD detection in PB that is applicable to most patients with AML. Initial results demonstrated the feasibility of targeted deep sequencing of CD34+ cells for early relapse prediction in clinical settings, with superior sensitivity and specificity, as compared with chimerism-based MRD assessment or the use of unsorted PB for NGS. The study was published on June 2, 2022 in the journal Blood Advances.
Related Links:
University Hospital Carl Gustav Carus
Miltenyi Biotec
BD Biosciences
Latest Immunology News
- Diagnostic Blood Test for Cellular Rejection after Organ Transplant Could Replace Surgical Biopsies
- AI Tool Precisely Matches Cancer Drugs to Patients Using Information from Each Tumor Cell
- Genetic Testing Combined With Personalized Drug Screening On Tumor Samples to Revolutionize Cancer Treatment
- Testing Method Could Help More Patients Receive Right Cancer Treatment
- Groundbreaking Test Monitors Radiation Therapy Toxicity in Cancer Patients
- State-Of-The Art Techniques to Investigate Immune Response in Deadly Strep A Infections
- Novel Immunoassays Enable Early Diagnosis of Antiphospholipid Syndrome
- New Test Could Predict Immunotherapy Success for Broader Range Of Cancers
- Simple Blood Protein Tests Predict CAR T Outcomes for Lymphoma Patients
- Cell Sorter Chip Technology to Pave Way for Immune Profiling at POC
- Chip Monitors Cancer Cells in Blood Samples to Assess Treatment Effectiveness
- Automated Immunohematology Approaches Can Resolve Transplant Incompatibility
- AI Leverages Tumor Genetics to Predict Patient Response to Chemotherapy
- World’s First Portable, Non-Invasive WBC Monitoring Device to Eliminate Need for Blood Draw
- Predictive T-Cell Test Detects Immune Response to Viruses Even Before Antibodies Form
- Single Blood Draw to Detect Immune Cells Present Months before Flu Infection Can Predict Symptoms
Channels
Clinical Chemistry
view channel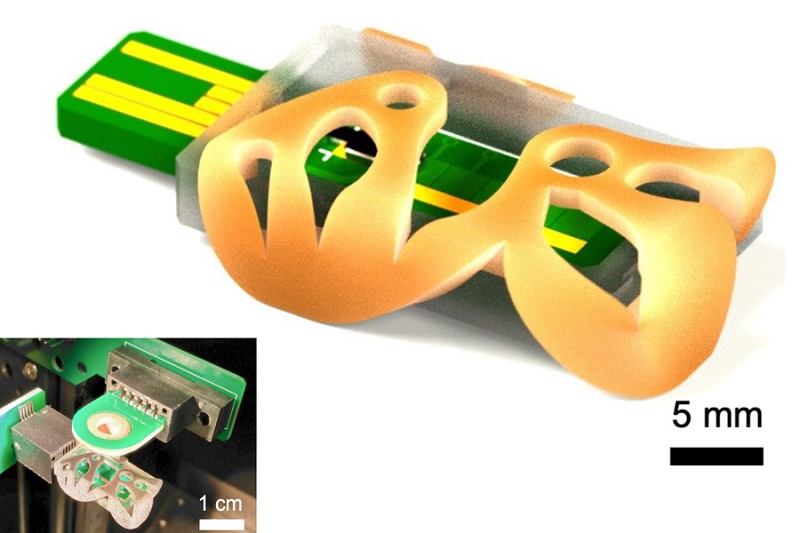
3D Printed Point-Of-Care Mass Spectrometer Outperforms State-Of-The-Art Models
Mass spectrometry is a precise technique for identifying the chemical components of a sample and has significant potential for monitoring chronic illness health states, such as measuring hormone levels... Read more.jpg)
POC Biomedical Test Spins Water Droplet Using Sound Waves for Cancer Detection
Exosomes, tiny cellular bioparticles carrying a specific set of proteins, lipids, and genetic materials, play a crucial role in cell communication and hold promise for non-invasive diagnostics.... Read more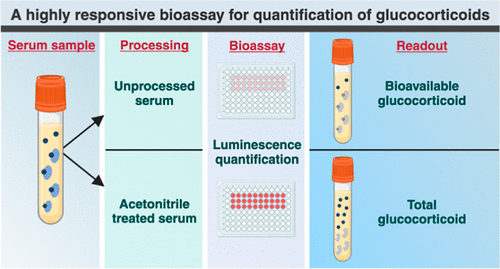
Highly Reliable Cell-Based Assay Enables Accurate Diagnosis of Endocrine Diseases
The conventional methods for measuring free cortisol, the body's stress hormone, from blood or saliva are quite demanding and require sample processing. The most common method, therefore, involves collecting... Read moreMolecular Diagnostics
view channel
Blood Test Accurately Predicts Lung Cancer Risk and Reduces Need for Scans
Lung cancer is extremely hard to detect early due to the limitations of current screening technologies, which are costly, sometimes inaccurate, and less commonly endorsed by healthcare professionals compared... Read more
Unique Autoantibody Signature to Help Diagnose Multiple Sclerosis Years before Symptom Onset
Autoimmune diseases such as multiple sclerosis (MS) are thought to occur partly due to unusual immune responses to common infections. Early MS symptoms, including dizziness, spasms, and fatigue, often... Read more
Blood Test Could Detect HPV-Associated Cancers 10 Years before Clinical Diagnosis
Human papilloma virus (HPV) is known to cause various cancers, including those of the genitals, anus, mouth, throat, and cervix. HPV-associated oropharyngeal cancer (HPV+OPSCC) is the most common HPV-associated... Read moreImmunology
view channel
Diagnostic Blood Test for Cellular Rejection after Organ Transplant Could Replace Surgical Biopsies
Transplanted organs constantly face the risk of being rejected by the recipient's immune system which differentiates self from non-self using T cells and B cells. T cells are commonly associated with acute... Read more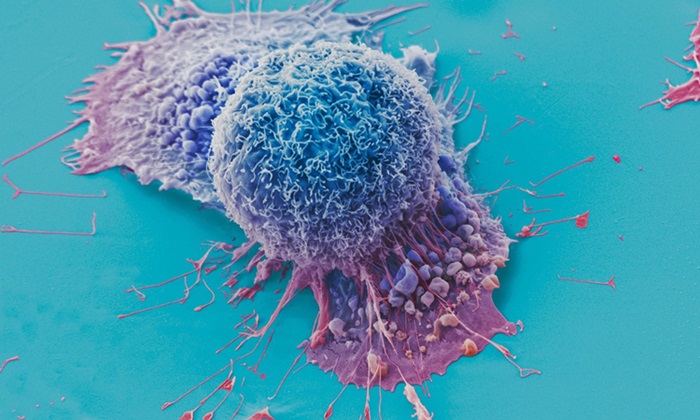
AI Tool Precisely Matches Cancer Drugs to Patients Using Information from Each Tumor Cell
Current strategies for matching cancer patients with specific treatments often depend on bulk sequencing of tumor DNA and RNA, which provides an average profile from all cells within a tumor sample.... Read more
Genetic Testing Combined With Personalized Drug Screening On Tumor Samples to Revolutionize Cancer Treatment
Cancer treatment typically adheres to a standard of care—established, statistically validated regimens that are effective for the majority of patients. However, the disease’s inherent variability means... Read moreMicrobiology
view channel
New CE-Marked Hepatitis Assays to Help Diagnose Infections Earlier
According to the World Health Organization (WHO), an estimated 354 million individuals globally are afflicted with chronic hepatitis B or C. These viruses are the leading causes of liver cirrhosis, liver... Read more
1 Hour, Direct-From-Blood Multiplex PCR Test Identifies 95% of Sepsis-Causing Pathogens
Sepsis contributes to one in every three hospital deaths in the US, and globally, septic shock carries a mortality rate of 30-40%. Diagnosing sepsis early is challenging due to its non-specific symptoms... Read morePathology
view channelAI-Powered Digital Imaging System to Revolutionize Cancer Diagnosis
The process of biopsy is important for confirming the presence of cancer. In the conventional histopathology technique, tissue is excised, sliced, stained, mounted on slides, and examined under a microscope... Read more
New Mycobacterium Tuberculosis Panel to Support Real-Time Surveillance and Combat Antimicrobial Resistance
Tuberculosis (TB), the leading cause of death from an infectious disease globally, is a contagious bacterial infection that primarily spreads through the coughing of patients with active pulmonary TB.... Read moreTechnology
view channel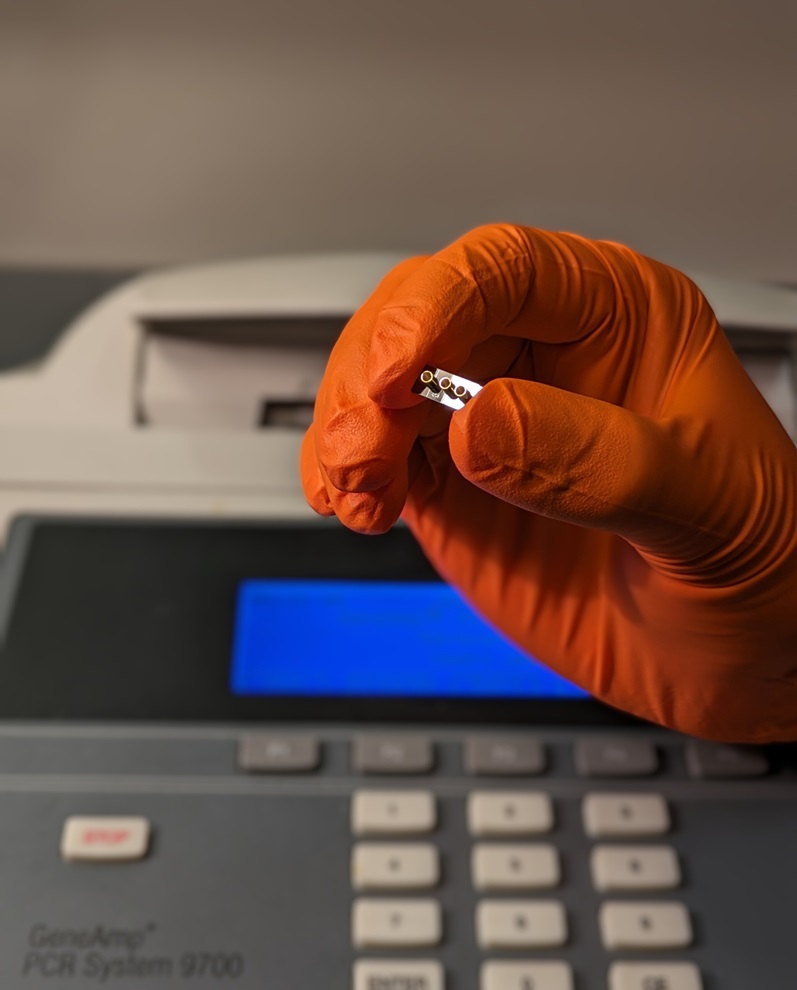
New Diagnostic System Achieves PCR Testing Accuracy
While PCR tests are the gold standard of accuracy for virology testing, they come with limitations such as complexity, the need for skilled lab operators, and longer result times. They also require complex... Read more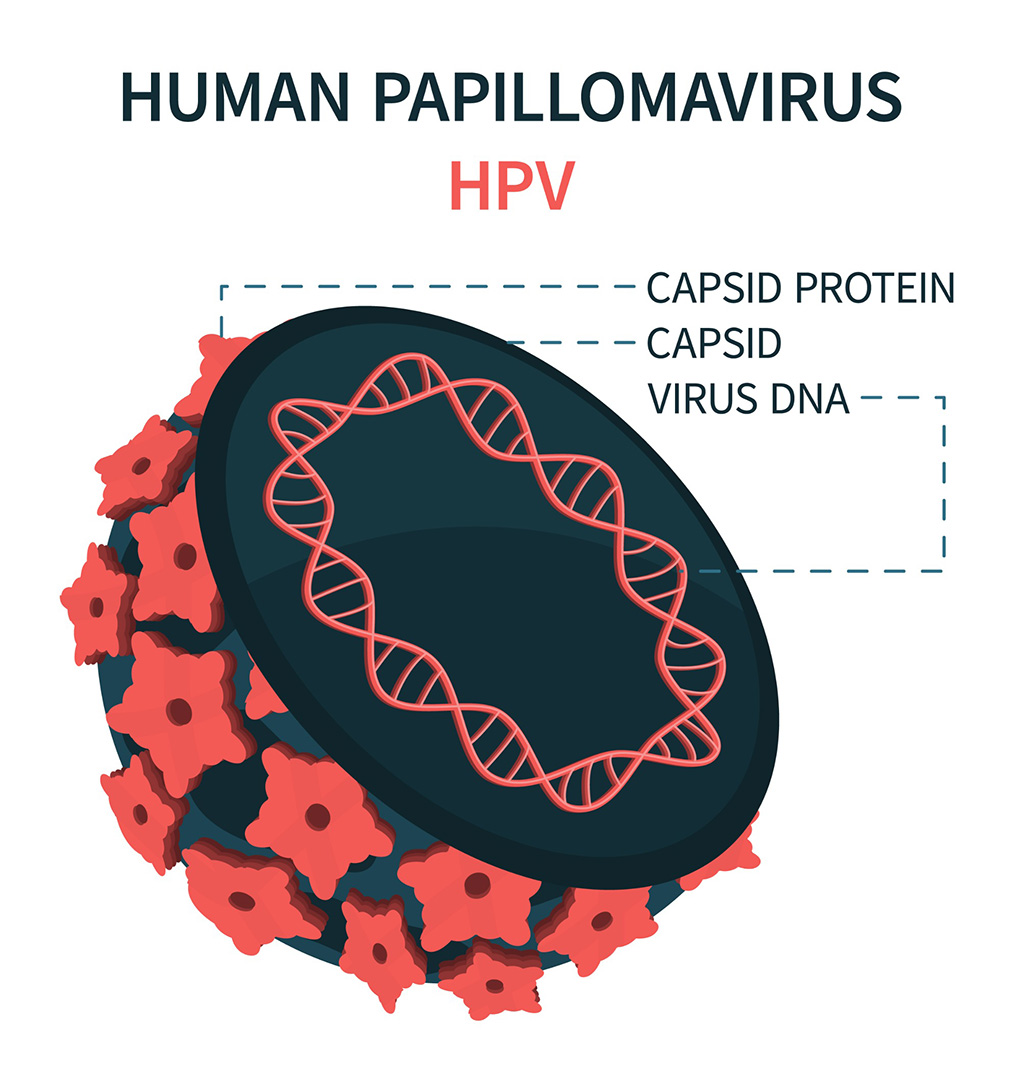
DNA Biosensor Enables Early Diagnosis of Cervical Cancer
Molybdenum disulfide (MoS2), recognized for its potential to form two-dimensional nanosheets like graphene, is a material that's increasingly catching the eye of the scientific community.... Read more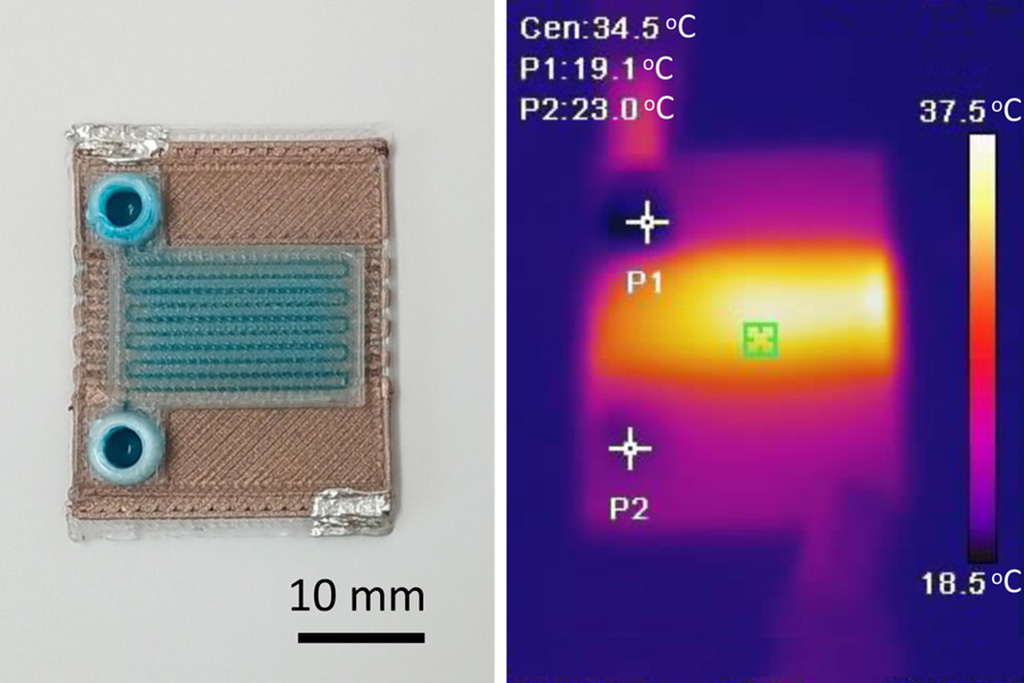
Self-Heating Microfluidic Devices Can Detect Diseases in Tiny Blood or Fluid Samples
Microfluidics, which are miniature devices that control the flow of liquids and facilitate chemical reactions, play a key role in disease detection from small samples of blood or other fluids.... Read more
Breakthrough in Diagnostic Technology Could Make On-The-Spot Testing Widely Accessible
Home testing gained significant importance during the COVID-19 pandemic, yet the availability of rapid tests is limited, and most of them can only drive one liquid across the strip, leading to continued... Read moreIndustry
view channel
ECCMID Congress Name Changes to ESCMID Global
Over the last few years, the European Society of Clinical Microbiology and Infectious Diseases (ESCMID, Basel, Switzerland) has evolved remarkably. The society is now stronger and broader than ever before... Read more
Bosch and Randox Partner to Make Strategic Investment in Vivalytic Analysis Platform
Given the presence of so many diseases, determining whether a patient is presenting the symptoms of a simple cold, the flu, or something as severe as life-threatening meningitis is usually only possible... Read more
Siemens to Close Fast Track Diagnostics Business
Siemens Healthineers (Erlangen, Germany) has announced its intention to close its Fast Track Diagnostics unit, a small collection of polymerase chain reaction (PCR) testing products that is part of the... Read more












.jpg)