Urinary KIM-1 Concentration Interpreted in Detecting AKI
|
By LabMedica International staff writers Posted on 25 Mar 2019 |

Image: The Urisys 2400 urine analyzer (Photo courtesy of Roche Diagnostics).
Kidney injury molecule-1 (KIM-1) has been identified as a biomarker for the assessment of nephropathy in various chronic kidney diseases (CKD). Extensive KIM-1 expression occurs in proximal tubule cells in patients with confirmed acute tubular necrosis.
Urinary KIM-1 concentrations were also significantly correlated with the expression of tissue KIM-1 in systemic lupus erythematosus patients. Such findings increase the potential use of urinary KIM-1 in the diagnosis or prognosis of CKD, but also results in the difficulties in the interpretation of urinary KIM-1 when it is used in the early detection of acute kidney injury (AKI).
Scientists collaborating with those at Queen’s University (Kingston, ON, Canada) obtained 188 urine samples were obtained from adults with normal kidney filtration. Of which 83 of the 188 showed negative urine protein, erythrocytes and leucocytes were used as normal controls. The remaining 105 samples showed at least one abnormal result suggesting possible pre-existing nephropathy.
Routine urine analysis was performed on an Urysis 2400 analyzer of the hospital core laboratory, using a multi-parameter test cassette that measures pH, protein (albumin), glucose, ketones, bilirubin, urobilinogen, nitrite, erythrocyte, leukocyte esterase, and specific gravity. The urinary KIM-1 concentrations were measured in duplicate for each sample using the Quantikine enzyme-linked immunosorbent assay (ELISA) kit. The limit of detection was 0.009μg/L.
The investigators reported that the results showed significantly increased urinary KIM-1 concentration in protein positive (protein +, erythrocyte +/-, leucocyte+/-) samples compared to controls that were negative for protein, erythrocytes, and leucocytes. Urinary KIM-1 concentrations were significantly higher when proteinuria was at trace concentration (0.25g/L) and correlated with the severity of proteinuria. The creatinine normalized urinary KIM-1 was significantly higher when urine protein was 0.75g/L to 5g/L. The reference interval for urinary KIM-1 was 0 to 4.19 μg/L, and for creatinine normalized urinary KIM-1 0 to 0.58 μg/mmol.
The authors concluded that baseline urinary KIM-1 concentrations were increased when there was detectable urine protein and correlated with its severity. The urinary KIM-1 concentrations should be interpreted with consideration of urine protein levels in individual patients. The study was published on March 7, 2019, in the journal Practical Laboratory Medicine.
Related Links:
Queen’s University
Urinary KIM-1 concentrations were also significantly correlated with the expression of tissue KIM-1 in systemic lupus erythematosus patients. Such findings increase the potential use of urinary KIM-1 in the diagnosis or prognosis of CKD, but also results in the difficulties in the interpretation of urinary KIM-1 when it is used in the early detection of acute kidney injury (AKI).
Scientists collaborating with those at Queen’s University (Kingston, ON, Canada) obtained 188 urine samples were obtained from adults with normal kidney filtration. Of which 83 of the 188 showed negative urine protein, erythrocytes and leucocytes were used as normal controls. The remaining 105 samples showed at least one abnormal result suggesting possible pre-existing nephropathy.
Routine urine analysis was performed on an Urysis 2400 analyzer of the hospital core laboratory, using a multi-parameter test cassette that measures pH, protein (albumin), glucose, ketones, bilirubin, urobilinogen, nitrite, erythrocyte, leukocyte esterase, and specific gravity. The urinary KIM-1 concentrations were measured in duplicate for each sample using the Quantikine enzyme-linked immunosorbent assay (ELISA) kit. The limit of detection was 0.009μg/L.
The investigators reported that the results showed significantly increased urinary KIM-1 concentration in protein positive (protein +, erythrocyte +/-, leucocyte+/-) samples compared to controls that were negative for protein, erythrocytes, and leucocytes. Urinary KIM-1 concentrations were significantly higher when proteinuria was at trace concentration (0.25g/L) and correlated with the severity of proteinuria. The creatinine normalized urinary KIM-1 was significantly higher when urine protein was 0.75g/L to 5g/L. The reference interval for urinary KIM-1 was 0 to 4.19 μg/L, and for creatinine normalized urinary KIM-1 0 to 0.58 μg/mmol.
The authors concluded that baseline urinary KIM-1 concentrations were increased when there was detectable urine protein and correlated with its severity. The urinary KIM-1 concentrations should be interpreted with consideration of urine protein levels in individual patients. The study was published on March 7, 2019, in the journal Practical Laboratory Medicine.
Related Links:
Queen’s University
Latest Immunology News
- Diagnostic Blood Test for Cellular Rejection after Organ Transplant Could Replace Surgical Biopsies
- AI Tool Precisely Matches Cancer Drugs to Patients Using Information from Each Tumor Cell
- Genetic Testing Combined With Personalized Drug Screening On Tumor Samples to Revolutionize Cancer Treatment
- Testing Method Could Help More Patients Receive Right Cancer Treatment
- Groundbreaking Test Monitors Radiation Therapy Toxicity in Cancer Patients
- State-Of-The Art Techniques to Investigate Immune Response in Deadly Strep A Infections
- Novel Immunoassays Enable Early Diagnosis of Antiphospholipid Syndrome
- New Test Could Predict Immunotherapy Success for Broader Range Of Cancers
- Simple Blood Protein Tests Predict CAR T Outcomes for Lymphoma Patients
- Cell Sorter Chip Technology to Pave Way for Immune Profiling at POC
- Chip Monitors Cancer Cells in Blood Samples to Assess Treatment Effectiveness
- Automated Immunohematology Approaches Can Resolve Transplant Incompatibility
- AI Leverages Tumor Genetics to Predict Patient Response to Chemotherapy
- World’s First Portable, Non-Invasive WBC Monitoring Device to Eliminate Need for Blood Draw
- Predictive T-Cell Test Detects Immune Response to Viruses Even Before Antibodies Form
- Single Blood Draw to Detect Immune Cells Present Months before Flu Infection Can Predict Symptoms
Channels
Molecular Diagnostics
view channel
Urine Test to Revolutionize Lyme Disease Testing
Lyme disease is the most common animal-to-human transmitted disease in the United States, with around 476,000 people diagnosed and treated annually, and its incidence has been increasing.... Read more
Simple Blood Test Could Enable First Quantitative Assessments for Future Cerebrovascular Disease
Cerebral small vessel disease is a common cause of stroke and cognitive decline, particularly in the elderly. Presently, assessing the risk for cerebral vascular diseases involves using a mix of diagnostic... Read more
New Genetic Testing Procedure Combined With Ultrasound Detects High Cardiovascular Risk
A key interest area in cardiovascular research today is the impact of clonal hematopoiesis on cardiovascular diseases. Clonal hematopoiesis results from mutations in hematopoietic stem cells and may lead... Read moreHematology
view channel
Next Generation Instrument Screens for Hemoglobin Disorders in Newborns
Hemoglobinopathies, the most widespread inherited conditions globally, affect about 7% of the population as carriers, with 2.7% of newborns being born with these conditions. The spectrum of clinical manifestations... Read more
First 4-in-1 Nucleic Acid Test for Arbovirus Screening to Reduce Risk of Transfusion-Transmitted Infections
Arboviruses represent an emerging global health threat, exacerbated by climate change and increased international travel that is facilitating their spread across new regions. Chikungunya, dengue, West... Read more
POC Finger-Prick Blood Test Determines Risk of Neutropenic Sepsis in Patients Undergoing Chemotherapy
Neutropenia, a decrease in neutrophils (a type of white blood cell crucial for fighting infections), is a frequent side effect of certain cancer treatments. This condition elevates the risk of infections,... Read more
First Affordable and Rapid Test for Beta Thalassemia Demonstrates 99% Diagnostic Accuracy
Hemoglobin disorders rank as some of the most prevalent monogenic diseases globally. Among various hemoglobin disorders, beta thalassemia, a hereditary blood disorder, affects about 1.5% of the world's... Read moreImmunology
view channel
Diagnostic Blood Test for Cellular Rejection after Organ Transplant Could Replace Surgical Biopsies
Transplanted organs constantly face the risk of being rejected by the recipient's immune system which differentiates self from non-self using T cells and B cells. T cells are commonly associated with acute... Read more
AI Tool Precisely Matches Cancer Drugs to Patients Using Information from Each Tumor Cell
Current strategies for matching cancer patients with specific treatments often depend on bulk sequencing of tumor DNA and RNA, which provides an average profile from all cells within a tumor sample.... Read more
Genetic Testing Combined With Personalized Drug Screening On Tumor Samples to Revolutionize Cancer Treatment
Cancer treatment typically adheres to a standard of care—established, statistically validated regimens that are effective for the majority of patients. However, the disease’s inherent variability means... Read moreMicrobiology
view channelEnhanced Rapid Syndromic Molecular Diagnostic Solution Detects Broad Range of Infectious Diseases
GenMark Diagnostics (Carlsbad, CA, USA), a member of the Roche Group (Basel, Switzerland), has rebranded its ePlex® system as the cobas eplex system. This rebranding under the globally renowned cobas name... Read more
Clinical Decision Support Software a Game-Changer in Antimicrobial Resistance Battle
Antimicrobial resistance (AMR) is a serious global public health concern that claims millions of lives every year. It primarily results from the inappropriate and excessive use of antibiotics, which reduces... Read more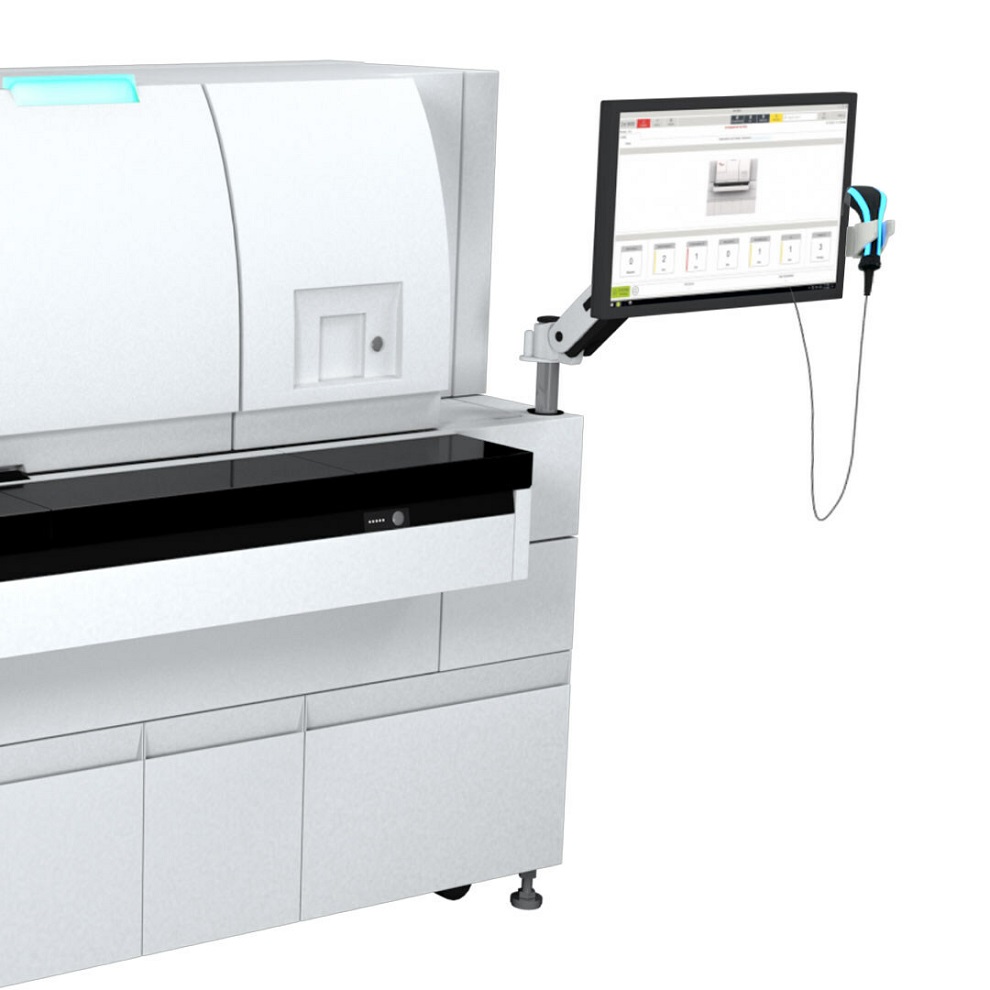
New CE-Marked Hepatitis Assays to Help Diagnose Infections Earlier
According to the World Health Organization (WHO), an estimated 354 million individuals globally are afflicted with chronic hepatitis B or C. These viruses are the leading causes of liver cirrhosis, liver... Read more
1 Hour, Direct-From-Blood Multiplex PCR Test Identifies 95% of Sepsis-Causing Pathogens
Sepsis contributes to one in every three hospital deaths in the US, and globally, septic shock carries a mortality rate of 30-40%. Diagnosing sepsis early is challenging due to its non-specific symptoms... Read morePathology
view channel
Robotic Blood Drawing Device to Revolutionize Sample Collection for Diagnostic Testing
Blood drawing is performed billions of times each year worldwide, playing a critical role in diagnostic procedures. Despite its importance, clinical laboratories are dealing with significant staff shortages,... Read more.jpg)
Use of DICOM Images for Pathology Diagnostics Marks Significant Step towards Standardization
Digital pathology is rapidly becoming a key aspect of modern healthcare, transforming the practice of pathology as laboratories worldwide adopt this advanced technology. Digital pathology systems allow... Read more
First of Its Kind Universal Tool to Revolutionize Sample Collection for Diagnostic Tests
The COVID pandemic has dramatically reshaped the perception of diagnostics. Post the pandemic, a groundbreaking device that combines sample collection and processing into a single, easy-to-use disposable... Read moreTechnology
view channel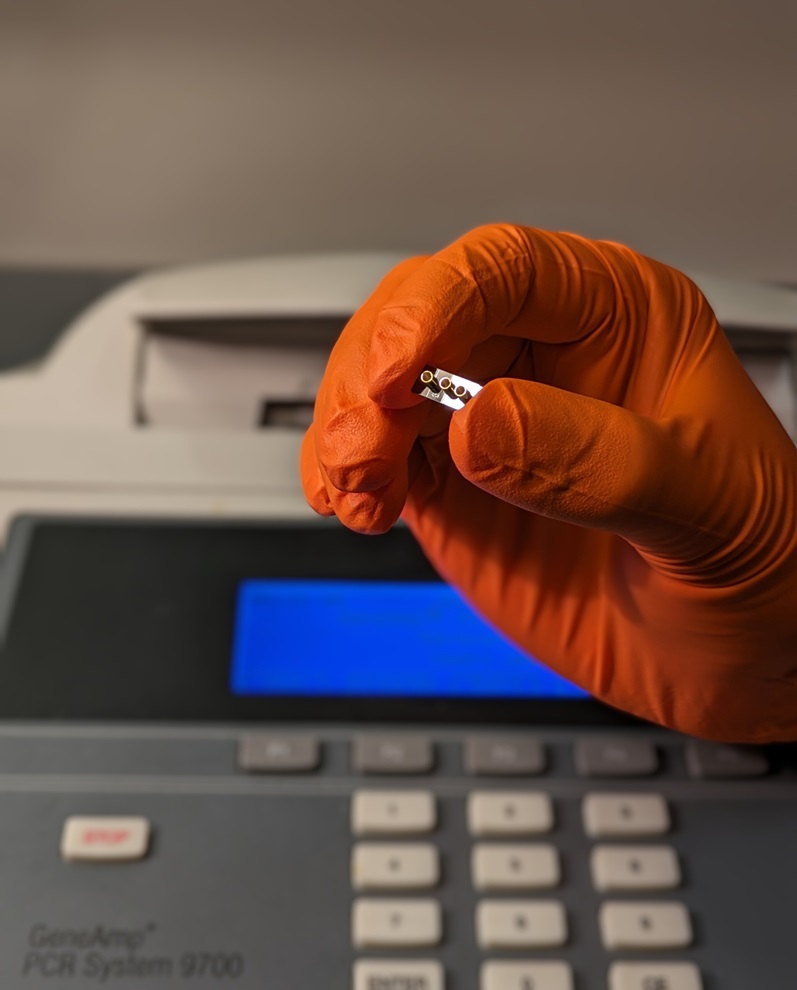
New Diagnostic System Achieves PCR Testing Accuracy
While PCR tests are the gold standard of accuracy for virology testing, they come with limitations such as complexity, the need for skilled lab operators, and longer result times. They also require complex... Read more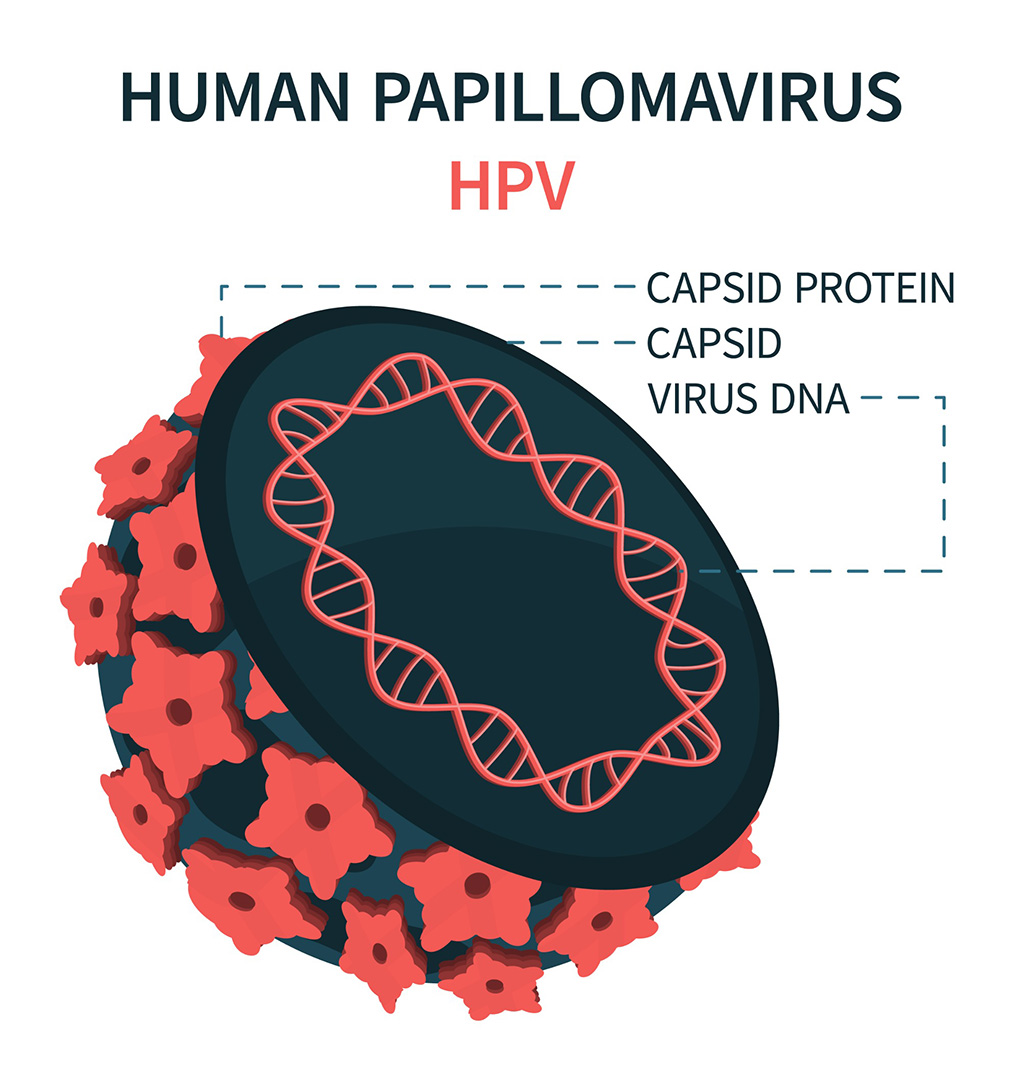
DNA Biosensor Enables Early Diagnosis of Cervical Cancer
Molybdenum disulfide (MoS2), recognized for its potential to form two-dimensional nanosheets like graphene, is a material that's increasingly catching the eye of the scientific community.... Read more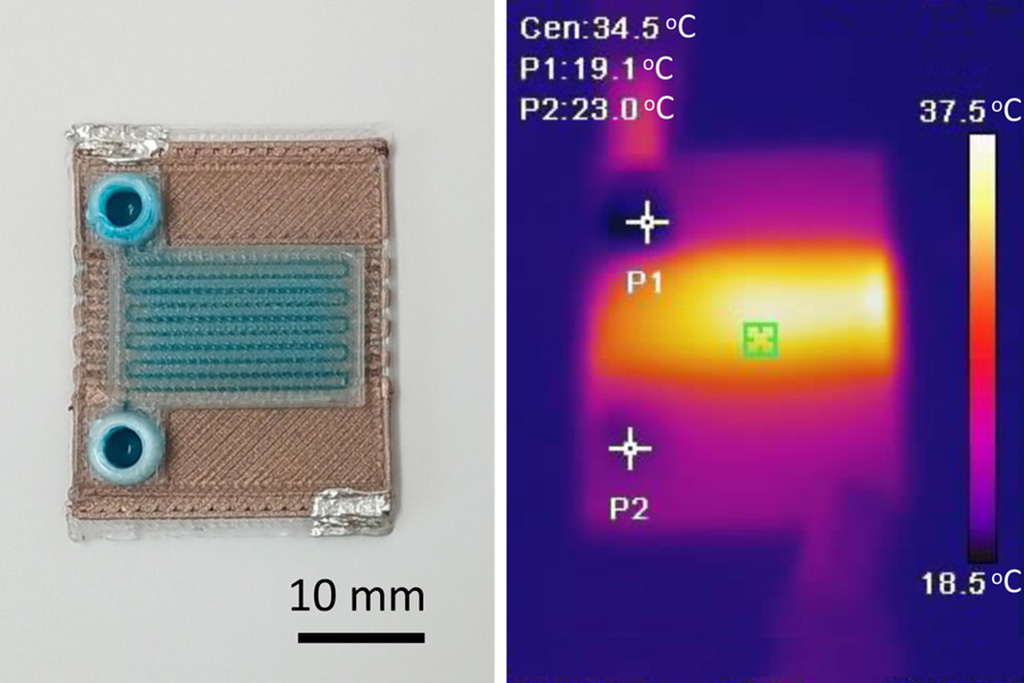
Self-Heating Microfluidic Devices Can Detect Diseases in Tiny Blood or Fluid Samples
Microfluidics, which are miniature devices that control the flow of liquids and facilitate chemical reactions, play a key role in disease detection from small samples of blood or other fluids.... Read more
Breakthrough in Diagnostic Technology Could Make On-The-Spot Testing Widely Accessible
Home testing gained significant importance during the COVID-19 pandemic, yet the availability of rapid tests is limited, and most of them can only drive one liquid across the strip, leading to continued... Read moreIndustry
view channel_1.jpg)
Thermo Fisher and Bio-Techne Enter Into Strategic Distribution Agreement for Europe
Thermo Fisher Scientific (Waltham, MA USA) has entered into a strategic distribution agreement with Bio-Techne Corporation (Minneapolis, MN, USA), resulting in a significant collaboration between two industry... Read more
ECCMID Congress Name Changes to ESCMID Global
Over the last few years, the European Society of Clinical Microbiology and Infectious Diseases (ESCMID, Basel, Switzerland) has evolved remarkably. The society is now stronger and broader than ever before... Read more