Bronchoalveolar Lavage Cell Pattern Determined for Diffuse Alveolar Hemorrhage
By LabMedica International staff writers
Posted on 11 Oct 2021
Diffuse alveolar hemorrhage (DAH) is a clinicopathological syndrome that describes the accumulation of intra-alveolar red blood cells originating from the alveolar capillaries. DAH can induce severe respiratory failure.Posted on 11 Oct 2021
Bronchoalveolar lavage (BAL) is an essential DAH diagnostic method. The BAL fluid (BALF) of DAH presents visually hemorrhagic and cytologically hemosiderin-laden macrophages. Antithrombotic therapy (AT) is known to be one of the causes of DAH, and other etiologies can induce DAH during AT.
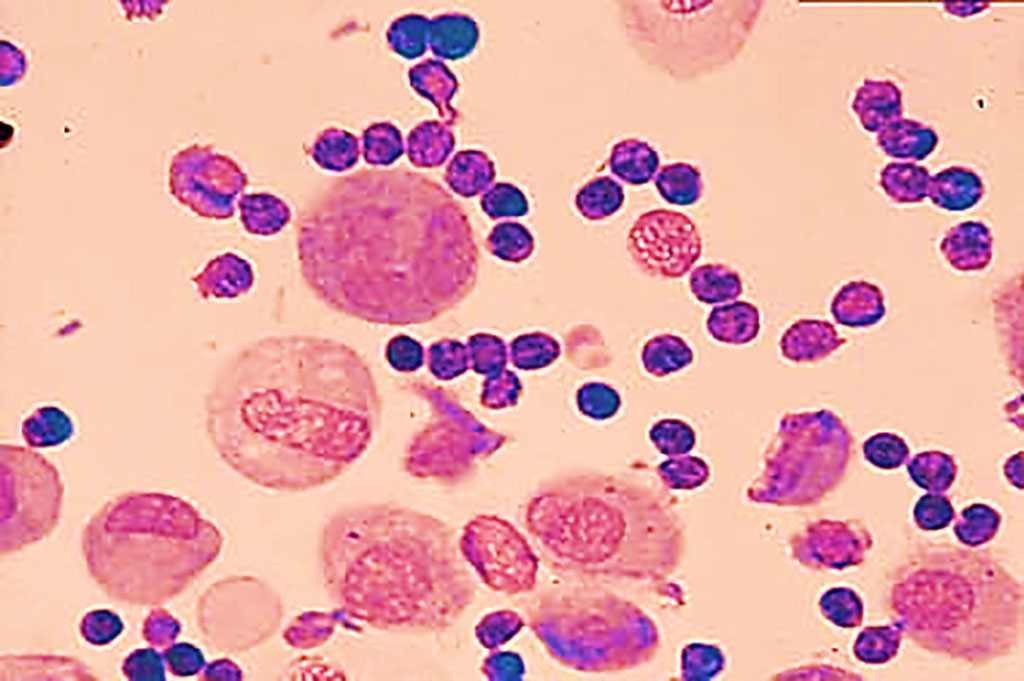
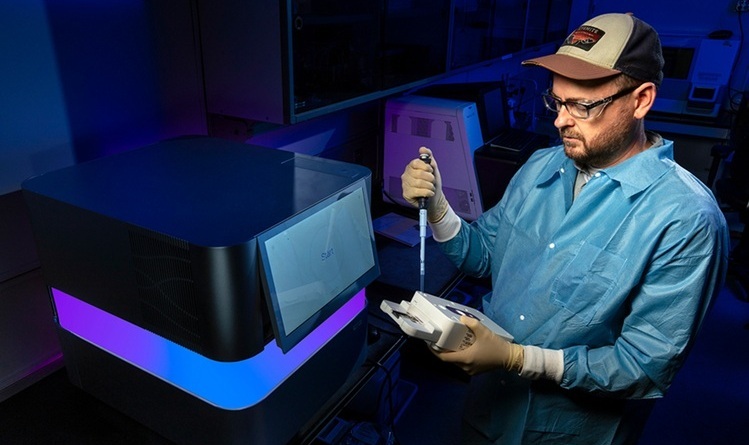
Image: Characteristic bronchoalveolar lavage findings of diffuse alveolar hemorrhage (Photo courtesy of Peter C. Bauer, MD)
Respiratory Specialists at the Osaka Police Hospital (Osaka-City, Japan) conducted a retrospective cohort study of patients admitted between October 2008 and July 2020. The study aim was to identify prognostic factors of DAH, especially bronchoalveolar lavage fluids (BALF) cell pattern. In the study, DAH was defined by the following criteria: Clinical and radiological presentation that was compatible with a diagnosis of DAH, and Bronchoalveolar lavage fluids (BALF) that was macroscopically bloody or cytologically contained hemosiderin-burden macrophages. Infection was confirmed when the specific microorganism was identified by culture or serological test. The team included 68 patients in their analysis with a median age was 75 (72–80) years, and 49 (72%) patients were male.
The investigators reported that in-hospital mortality was 26.5%. Variables associated with in-hospital death were neutrophils percentage in BALF ≥ 44.5% [Odds Ratio (OR) 16.0, 95% confidence interval (CI) 4.33–58.9)], lymphocytes percentage in BALF < 14% (OR 7.44, 95% CI 2.11–26.2), idiopathic DAH (OR 0.31, 95% CI 0.10–0.95), oxygen flow ≥ 4L/min (OR 3.90, 95% CI 1.20–12.6), and estimated glomerular filtration rate < 60 mL/min (OR 5.00, 95%CI 1.29–19.4). In-hospital mortality was significantly higher in patients with neutrophils percentage ≥ 44.5% and lymphocytes percentage < 14% compared with patients with neutrophils percentage < 44.5% and lymphocytes percentage ≥ 14%.
The authors concluded that a higher neutrophils percentage in BALF was found to be significantly associated with in-hospital mortality. On the other hand, a higher lymphocytes percentage in BALF was correlated with lower mortality. The study was published on September 9, 2021 in the journal BMC Pulmonary Medicine.
Related Links:
Osaka Police Hospital









 (3) (1).png)