Cancer Risk Assessed by Circulating Protein Biomarker Panel
By LabMedica International staff writers
Posted on 10 Aug 2018
The question has been asked whether a risk prediction model based on circulating protein biomarkers improve on a traditional risk prediction model for lung cancer and the current USA screening criteria.Posted on 10 Aug 2018
Current screening criteria for lung cancer risk assessments often miss a large proportion of cases. It has recently been suggested that a panel of specific circulating protein biomarkers may improve lung cancer risk assessment and may be used to define eligibility for computed tomography screening.
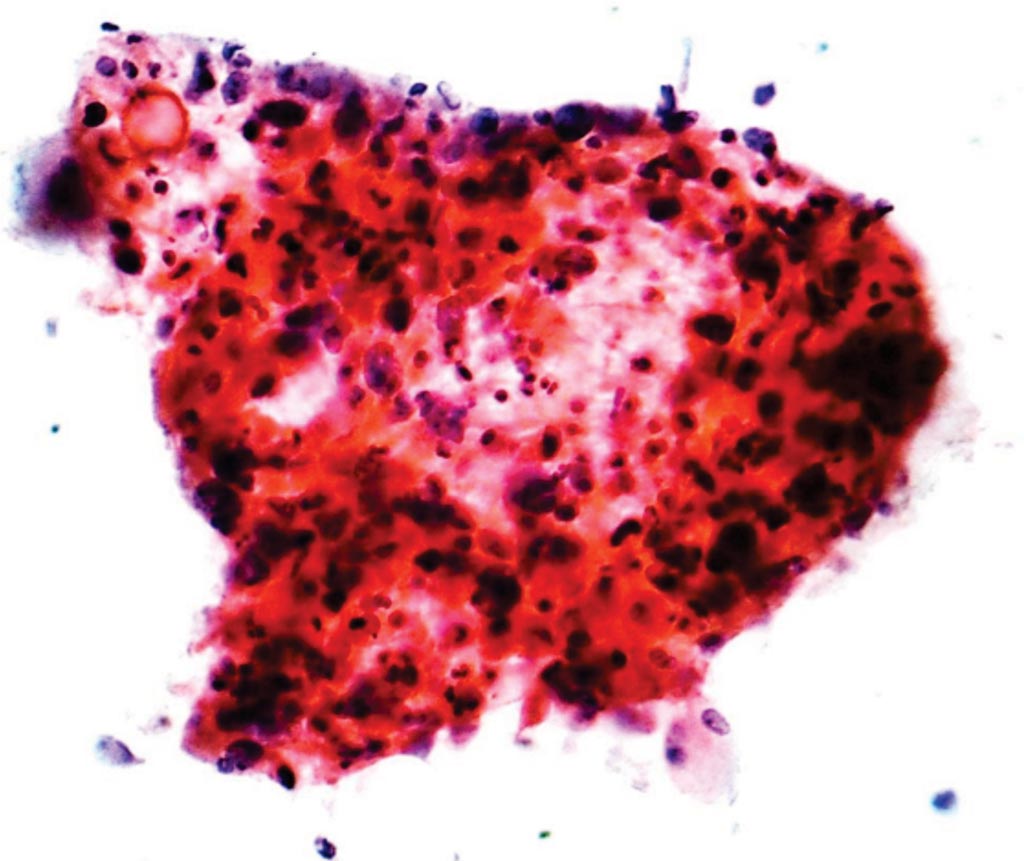
Image: A photomicrograph of squamous-cell carcinoma, a type of non-small-cell carcinoma of the lung, from a fine needle aspiration specimen (Photo courtesy of Nephron).
A large international consortium of scientists led by International Agency for Research on Cancer (Lyon, France) collected prediagnostic samples from 108 ever-smoking patients with lung cancer diagnosed within one year after blood collection and samples from 216 smoking-matched controls from the Carotene and Retinol Efficacy Trial (CARET) cohort. The samples were used to develop a biomarker risk score based on four proteins (cancer antigen 125 [CA125], carcinoembryonic antigen [CEA], cytokeratin-19 fragment [CYFRA 21-1], and the precursor form of surfactant protein B [Pro-SFTPB]). The biomarker score was subsequently validated blindly using absolute risk estimates among 63 ever-smoking patients with lung cancer diagnosed within one year after blood collection and 90 matched controls from two large European population-based cohorts.
In the validation study of 63 ever-smoking patients with lung cancer and 90 matched controls (age, 57.7 ± 8.7 years; 68.6% men) from the cohorts, an integrated risk prediction model that combined smoking exposure with the biomarker score yielded an AUC of 0.83 (95% CI, 0.76-0.90) compared with 0.73 (95% CI, 0.64-0.82) for a model based on smoking exposure alone. With an overall specificity of 0.83, based on the US Preventive Services Task Force (USPSTF) screening criteria, the sensitivity of the integrated risk model was 0.63 compared to 0.43 for the smoking model. Additionally, at an overall sensitivity of 0.41 the integrated risk model yielded a specificity of 0.95 compared with 0.86 for the smoking model, based on the USPSTF screening criteria.
The authors concluded that these improvements in sensitivity and specificity were consistently observed across each evaluated stratum. Their findings also indicated that the improvement in discrimination afforded by the biomarker score is more modest beyond the initial year after blood draw, which suggests that an annual biomarker test may be necessary in a screening program. The study was published on July 12, 2018, in the journal JAMA Oncology.
Related Links:
International Agency for Research on Cancer