Liquid Biopsy Can Rule Out Early-Stage Lung Cancer
By LabMedica International staff writers
Posted on 05 Apr 2018
Lung nodules are a diagnostic challenge with an estimated yearly incidence of 1.6 million in the USA. The majority of these patients have benign lung nodules; however, there are significant costs, morbidity and mortality associated with the invasive biopsies needed to determine which nodules are cancerous.Posted on 05 Apr 2018
It has been found that of these pulmonary nodules detected each year more than 90% of those smaller than two centimeters (around 3/4 inch) in diameter are benign, and current detection methods include positron-emission tomography (PET) scans, bronchoscopy, needle biopsy, and surgery. A new study has confirmed the accuracy of a liquid biopsy that can help rule out early-stage lung cancer.
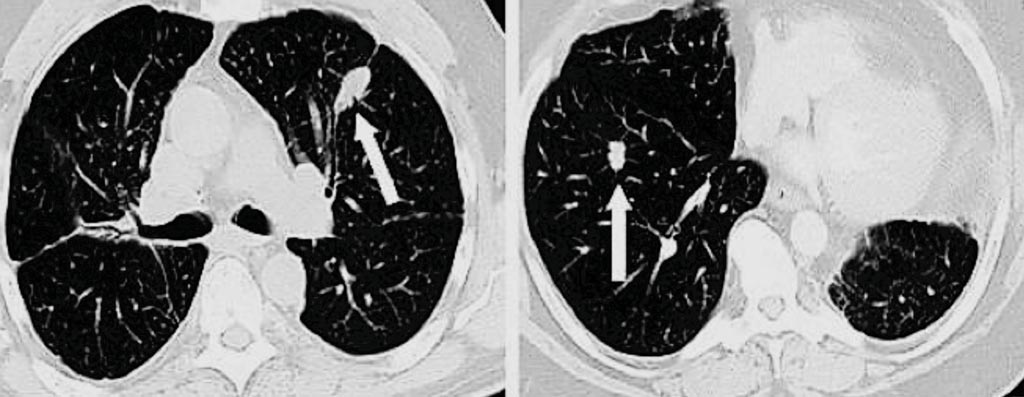
Image: Computerized tomography (CT) scans from two different patients with pulmonary nodules. The arrow on the left points to a benign (noncancerous) nodule, while the arrow on the right shows a small lung cancer (Photo courtesy of The Lung Cancer Center at The Valley Hospital).
A large team of medical scientists working with those at the Medical University of South Carolina, Charleston, SC, USA) carried out a prospective multicenter observational trial of 685 patients with 8-30 mm lung nodules at 33 sites in the USA and Canada. Multiple reaction monitoring mass spectrometry measured the relative abundance of two plasma proteins, galectin-3 binding protein (LG3BP) and scavenger receptor cysteine-rich type 1 (C163A). Results were integrated with a clinical risk prediction model to identify likely benign nodules. Sensitivity, specificity and negative predictive value were calculated.
The liquid biopsy used in the study was the Xpresys Lung 2 ('XL2') a second-generation diagnostic test Integrated Diagnostic (Seattle, WA, USA). A subgroup of 178 patients had a 16% prevalence of lung cancer. The integrated classifier demonstrated a sensitivity of 97% a specificity of 44% and a negative predictive value (NPV) of 98% in distinguishing benign from malignant nodules. The classifier performed better than positron emission tomography (PET), validated lung nodule risk models, and physician cancer probability estimates. If the integrated classifier results were used to direct care, 40% fewer procedures would be performed on benign nodules while 3% of malignant nodules would be misclassified.
Albert Luderer, PhD, president of Integrated Diagnostics, said, “Physicians can often detect whether a patient is at high risk for cancer, but have difficulty determining when a small lung nodule is benign. Patients determined by traditional means to be at low risk are often put into a “watchful waiting” category to be re-tested over time. The XL2 test might help patients with low-to-moderate risk of cancer to avoid unnecessary invasive procedures.” The study was published on March 1, 2018, in the journal Chest.
Related Links:
Medical University of South Carolina
Integrated Diagnostic













