Genetic Markers Linked to Development of Lymphedema
By LabMedica International staff writers
Posted on 08 May 2013
A clear association has been revealed between certain genes and the development of lymphedema, after breast cancer surgery and certain other cancer treatments.Posted on 08 May 2013
The risks of developing lymphedema increases significantly for women who had more advanced breast cancer at the time of diagnosis, more lymph nodes removed or a significantly higher body mass index.

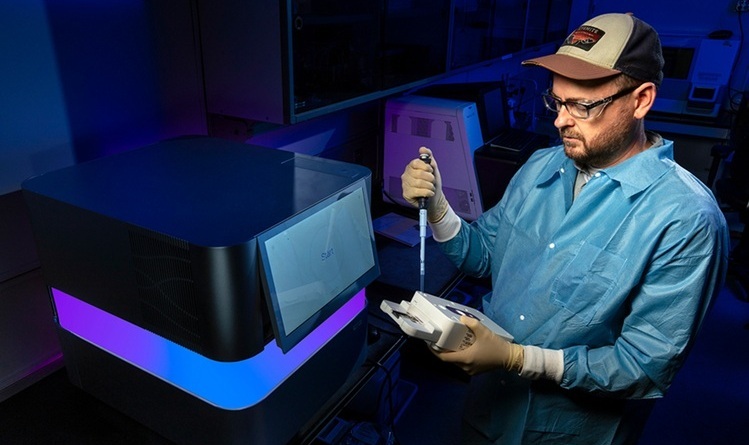
Image: Bioimpedance spectroscopy device (Photo courtesy of ImpediMed).
Scientists at the University of California - San Francisco (CA, USA) investigated 410 women who were at least six months post-treatment for breast cancer surgery on one breast, and either had lymphedema in their upper extremity or did not have the condition.
The team evaluated genetic predictors of lymphedema using a type of technology called bioimpedance spectroscopy (BIS) to measure increases in fluid in the arm. Bioimpedance spectroscopy is a noninvasive procedure that allows one to measure body composition including an increase in fluid in an arm or a leg. Genotyping was done using a custom genotyping array.
The BIS measurements were taken using a single channel BIS device (SFB7 device; ImpediMed; San Diego, CA; USA) in the lymphedema study or the Quantum X Bioelectrical Impedance Device (RJL Systems; Clinton Township, MI, USA) in another study. Genotyping was performed blinded to lymphedema status and positive and negative controls were included. DNA was quantitated with a Nanodrop Spectrophotometer (Wilmington, DE, USA). Samples were genotyped using the GoldenGate genotyping platform (Illumina; San Diego, CA, USA).
The scientist found that while not all of the candidate genes were associated with the development of LE, the significant associations that were identified provide new information on genomic risk factors and potential therapeutic targets. They found that women with lymphedema had more advanced breast cancer at the time of diagnosis; a higher number of positive lymph nodes; and were more likely to have a significantly higher body mass index.
Christine Miaskowski, RN, PhD, the lead author, said, “These findings suggest that complex interactions may exist between a variety of patient characteristics and genetic markers that place some women at higher risk for the development of lymphedema. Our hope is that once our findings are confirmed in a future study, we will be able to identify women at higher risk for lymphedema prior to breast cancer surgery, and initiate measures to prevent the development of this devastating condition." The study was published on April 16, 2013, in the journal Public Library of Science ONE.
Related Links:
University of California - San Francisco
ImpediMed
RJL Systems