Blood Test to Improve Diagnosis and Management of ALS
Posted on 27 Feb 2025
Amyotrophic lateral sclerosis (ALS) is often challenging to diagnose and predict in terms of disease progression. An effective biomarker would be invaluable—not only in assisting with diagnosis but also in predicting prognosis, assessing disease stages, and monitoring patient progress or their response to treatment. Now, a new study has identified which blood tests are most effective for identifying and tracking ALS.
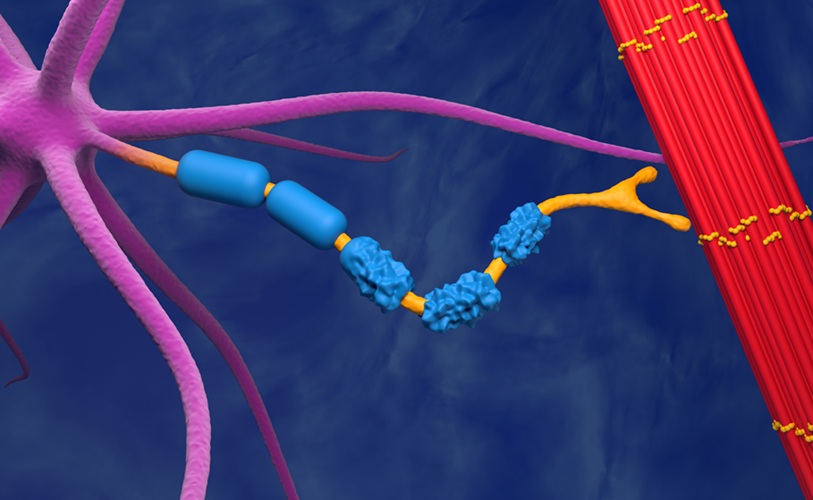
Researchers at Inserm Hospital (Paris, France) and University of Montpellier (Montpellier, France) conducted a study comparing three types of blood biomarkers: neurofilament light chain proteins, glial acidic proteins, and phosphorylated tau 181. Neurofilament light chain proteins are detectable in the blood when nerve cells are injured or die. Glial acidic proteins are released when the body attempts to repair such injuries, while phosphorylated tau 181 is linked to amyloid protein accumulation, a hallmark of Alzheimer’s disease. The study also assessed four different techniques to measure neurofilament light chain levels. The study, published in Neurology, involved 139 individuals diagnosed with ALS and 70 individuals with similar conditions such as lower motor neuron disease and primary lateral sclerosis. The participants’ blood was tested for these three biomarkers.
The study followed the ALS patients for an average of 3.5 years and the non-ALS group for approximately 12 years. During this period, 86% of the ALS patients passed away, compared to only 8% of those with other conditions. For neurofilament light chain proteins, those with ALS had levels three times higher in their blood compared to individuals with other diseases. The study found that tests measuring neurofilament light chain proteins accurately identified ALS patients over 80% of the time. In contrast, the accuracy of tests for glial acidic proteins and phosphorylated tau 181 was much lower, yielding correct results only about 50% of the time. Additionally, the researchers identified a specific threshold level of neurofilament light chain proteins that could predict survival in ALS patients. Within a year, over 40% of those with protein levels below the threshold were still alive, while none of those with higher protein levels survived.
“While more research needs to be done to confirm these findings, having better information about prognosis is valuable for people with ALS and their families as well as the doctors who treat them,” said study author Sylvain Lehmann, MD, PhD.










 Analyzer.jpg)



