Phosphorylated-Tau Blood Test Identifies Asymptomatic Alzheimer’s Disease
By LabMedica International staff writers
Posted on 10 Aug 2020
A blood test that determines circulating levels of the Alzheimer's disease (AD) biomarker protein phospho-tau217 (p-tau217) was found to distinguish AD from other neurodegenerative diseases, with significantly higher accuracy than established plasma- and MRI-based biomarkers, and its performance was not significantly different from key cerebral spinal fluid (CSF)- or PET-based measurements.Posted on 10 Aug 2020
The tau proteins are a group of six highly soluble protein isoforms produced by alternative splicing from the MAPT (microtubule-associated protein tau) gene. They have roles primarily in maintaining the stability of microtubules in axons and are abundant in the neurons of the central nervous system (CNS). They are less common elsewhere but are also expressed at very low levels in CNS astrocytes and oligodendrocytes. Pathologies and dementias of the nervous system such as Alzheimer's disease and Parkinson's disease are associated with tau proteins that have morphed into hyperphosphorylated insoluble aggregates called neurofibrillary tangles.
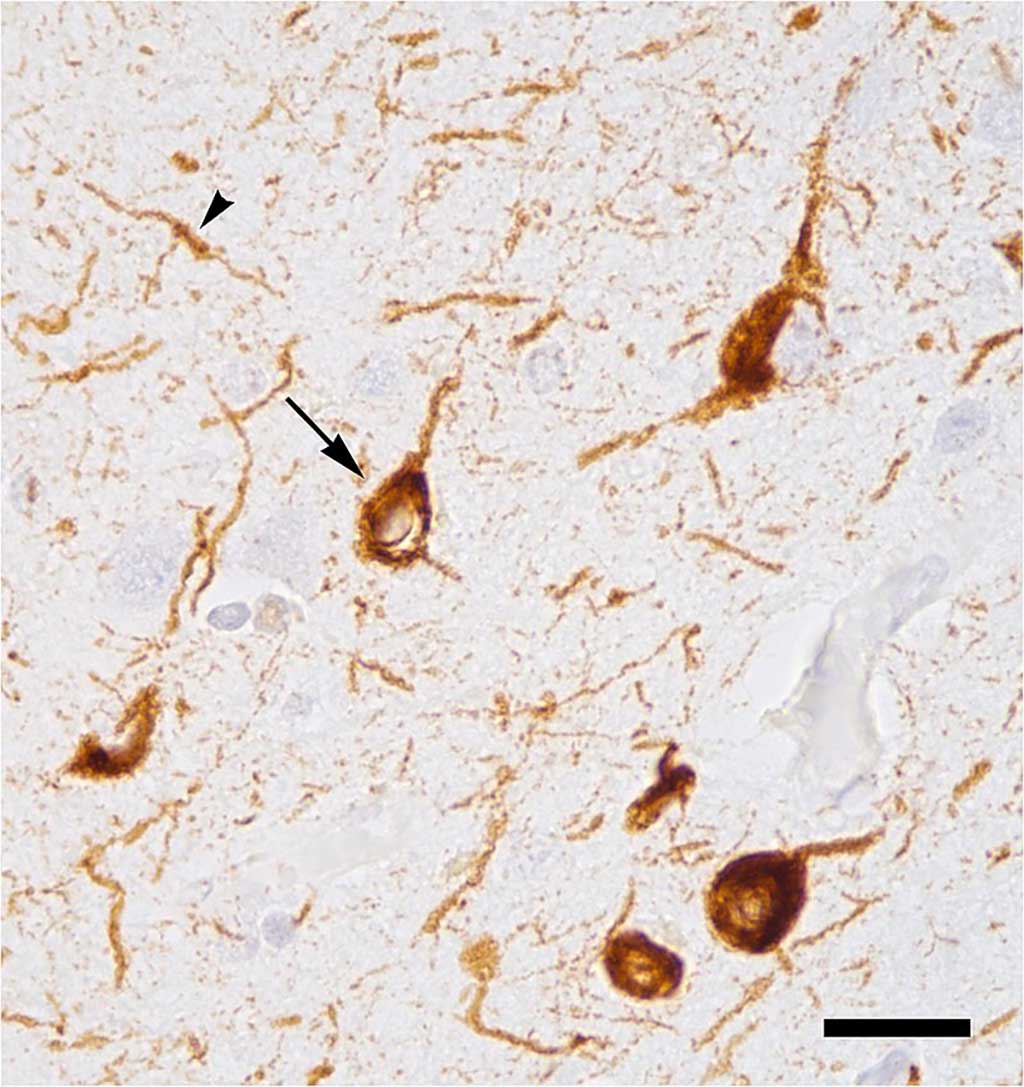
Abnormal accumulation of tau protein in neuronal cell bodies (arrow) and neuronal extensions (arrowhead) in the neocortex of a patient who had died with Alzheimer\'s disease (Photo courtesy of Wikimedia Commons)
In the current study, investigators at Lund University (Sweden) and their collaborators sought to determine the discriminative accuracy of plasma p-tau217 for differentiating Alzheimer’s disease from other neurodegenerative disorders and neuropathologically defined AD from non-AD individuals.
For this study, the investigators worked with a new p-tau217 blood test, developed by Eli Lilly and Company (Indianapolis, IN, USA;), to analyze samples from 1,402 cognitively impaired and unimpaired research participants from studies in Arizona (Cohort 1: 81 Arizona participants in Banner Sun Health Research Institute's Brain Donation program), Sweden (Cohort 2: 699 participants in the Swedish BioFINDER Study), and Colombia (Cohort 3: 522 autosomal dominant Alzheimer's disease (ADAD)-causing mutation carriers and non-carriers).
The accuracy of plasma p-tau217 was compared with other key plasma, CSF, PET, and MRI biomarkers for AD. Secondary objectives were to investigate the age at which plasma p-tau217 levels increased in autosomal-dominant AD and if plasma p-tau217 levels were associated with AD-like tau pathology, determined using neuropathology or tau-PET.
Results revealed that in Cohort 1, plasma p-tau217 differentiated neuropathologically defined AD from non-AD with significantly higher accuracy than plasma p-tau181 and neurofilament light chain (NfL). The discriminative accuracy of plasma p-tau217 in Cohort 2 for clinical AD dementia versus other neurodegenerative diseases was significantly higher than plasma p-tau181, plasma NfL, and MRI measures but not significantly different compared with CSF p-tau217, CSF p-tau181, and tau-PET. In Cohort 3, plasma p-tau217 levels were significantly greater among PSEN1 mutation carriers, compared with noncarriers, from approximately 25 years and older, which is 20 years prior to estimated onset of MCI (mild cognitive impairment) among mutation carriers.
Plasma p-tau217 levels correlated with tau tangles in participants with but not without beta-amyloid plaques in Cohort 1. In Cohort 2, plasma p-tau217 discriminated abnormal versus normal tau-PET scans with significantly higher accuracy than plasma p-tau181, plasma NfL, CSF p-tau181, CSF beta-amyloid 42/beta-amyloid 40 ratio, and MRI measures, but its performance was not significantly different compared with CSF p-tau217.
"The p-tau217 blood test has great promise in the diagnosis, early detection, and study of Alzheimer's," said senior author Dr. Oskar Hansson, professor of clinical memory research at Lund University. "While more work is needed to optimize the assay and test it in other people before it becomes available in the clinic, the blood test might become especially useful to improve the recognition, diagnosis, and care of people in the primary care setting."
The study was published in the July 28, 2020, online edition of the Journal of the American Medical Association.
Related Links:
Lund University
Eli Lilly and Company














