Metabolomics-Based Blood Test Used for Diagnosis of NSCLC
By LabMedica International staff writers
Posted on 22 Jul 2019
A metabolomics-based blood test may reduce the need to rely on low-dose CT (computed tomography) scans for the diagnosis of non-small-cell lung cancer (NSCLC).Posted on 22 Jul 2019
While low-dose CT has shown promise for detecting early stage lung cancer (LuCa), concerns about the adverse health effects of radiation and high cost prevent its use as a population-wide screening tool. Therefore, novel, low-cost, and safe LuCa tests that would prompt patients with suspicious screening results to seek further radiological evaluation are needed.
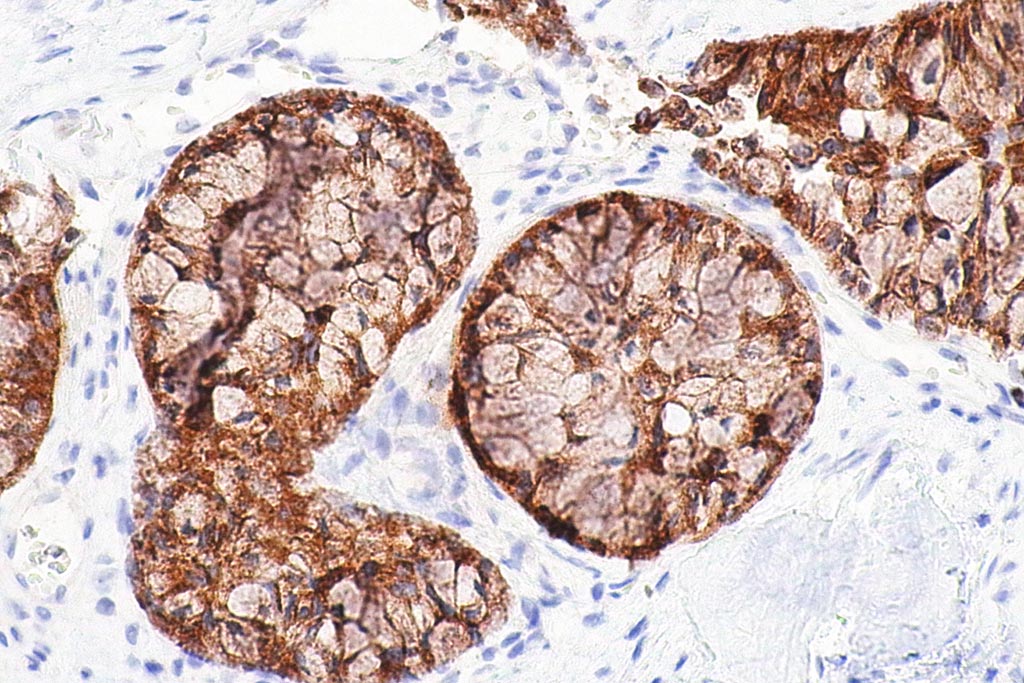
Image: A micrograph showing an adenocarcinoma of the lung (Photo courtesy of Wikimedia Commons).
As part of an effort to develop such screening tests, investigators at Massachusetts General Hospital (Boston, MA, USA) used high-resolution magic angle spinning magnetic resonance spectroscopy (HRMAS MRS) to examine human lung cancer metabolomics from 93 paired tissue-serum samples. This method was developed for metabolomic analysis of intact biological tissues and complex fluids. It allows subsequent histopathology analyses of the same tissue samples, enabling spectroscopic data to be interpreted according to tissue pathologies.
Paired specimens examined in this study originated from 42 patients with squamous cell carcinomas (SCC) of the lung, and 51 patients with adenocarcinomas of the lung. Blood samples from 29 healthy volunteers served as controls. The patients included 58 with early (Stage I) lung cancer, and 35 with more advanced disease (Stage II, III, or IV).
Assay results identified serum metabolomic profiles that could predict patient overall survival for all cases, and more importantly for Stage I cases alone, a prediction, which is significant for treatment strategies but currently cannot be achieved by any clinical method. Prolonged survival was associated with relative overexpression of glutamine, valine, and glycine, and relative suppression of glutamate and lipids in serum.
Since HRMAS MRS could also analyze the complex biofluid of serum and obtain spectra of high resolution, tissue and serum metabolomic measures were correlated in order to investigate the associations between metabolites of potential LuCa biomarkers measured from paired tissue and serum samples.
“The uniqueness of our study is that we have paired samples from patients obtained at the same time as surgery. You cannot use CT as a screening tool for every patient or even for every at-risk patient every year, so what we are trying to do is to develop biomarkers from blood samples that could be incorporated into physical exams, and if there is any suspicion of lung cancer, then we would put the patient through CT,” said senior author Dr. Leo L. Cheng, associate biophysicist in the departments of pathology and radiology at Massachusetts General Hospital.
The paper was published in the July 16, 2019, online edition of the journal Scientific Reports.
Related Links:
Massachusetts General Hospital